Skinfold over toenail is pathognomonic for the popliteal pterygium syndrome in a Congolese family with large intrafamilial variability
Key Clinical Message
We report on three related Congolese popliteal pterygium syndrome (PPS) patients concordant only for the skinfold over the toenail. Mutation analysis revealed that the three affected individuals carried a heterozygous missense mutation in the Exon 4, NM_006147.2:c.250C>T; p.Arg84Cys. This is the first molecularly confirmed PPS family from central Africa.
Introduction
The popliteal pterygium syndrome (PPS, OMIM 119500) is a rare autosomal dominant disorder affecting about 1 in 300,000 births 9. Clinical manifestations include cleft lip/palate, lower lip pits, syngnathia, ankyloblepharon filiforme, pterygium in the popliteal region, pyramidal skinfold overlying the nail of the hallux, syndactyly, oligodactyly, and abnormal genitalia 5. The condition is caused by mutations in the Interferon Regulatory Factor 6 (IRF6) gene. The inheritance is autosomal dominant, and there is marked intra- and interfamilial variability in the phenotype 6, 12. Of interest, the association of cleft lip and/or palate with the typical feature of lower lip pits has been recognized as a separate disorder, the Van Der Woude Syndrome (VWS, OMIM 119300) 10. Since both disorders are observed in the same family and can be caused by the same mutations in the IRF6, the term “IRF6 related disorders” was coined to indicate the spectrum, with VWS and PPS being the milder and the severe variants, respectively 3, 5.
Only few African VWS/PPS patients have been reported thus far, many of them lacking molecular diagnosis 1, 7, 8, 18. From a scientific point of view, it is of interest to perform clinical and genetic studies in Africa, for well characterized disorders with phenotypic and genetic heterogeneity. First, as evidenced by a recent study on secondary variants in exome sequencing, existing databases lack sufficient data on individuals from African descent 4. Next, differences in genetic background may result in different phenotypes, and may offer additional opportunities in identifying modifiers. Here, we report a pedigree of African patients from Democratic Republic of Congo, with PPS, molecularly confirmed.
Observation
This is a clinical case report of a male new born who was admitted at the Pediatric department of the University Hospitals, University of Kinshasa, 9 h after birth because of congenital malformations. He was the seventh child of unrelated Congolese parents. Pregnancy and delivery were uneventful. Morphological features were consistent with 39.5 weeks of gestational age (Finnström scale). Weight was 3340 g (P₅₀–P₇₅), length 47 cm (P₁₀–P₂₅) and occipital-frontal circumference (OFC) 36 cm (>P90). Dysmorphic manifestations included ankyloblepharon filiforme of the right eye, syngnathia, and isolated left-sided cleft lip. There was bilateral pterygium extending from the proximal part of the thigh to the heel, and hampering extension movements. He had a bilateral skinfold overlying the nail of the second toe, dysplastic toenails, bilateral feet oligodactyly, syndactyly of the second and third toes on the left foot, and cryptorchidism (Fig. 1A). A CT-Scan excluded bony malformations of the oral region (data available on request).
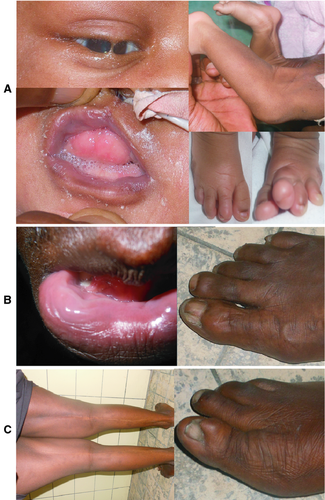
The 42-year-old father had lower lip pits and a skinfold over the nail of the right hallux (Fig. 1B). Index's 16-year-old sister had fibrous bands extending from the mid-thigh to the heels, bilaterally, and a pyramidal skinfold covering part of the right hallux's nail (Fig. 1C). Both the father and sister had normal intelligence and had normal development. Clinical examination of the mother and one index's brother was normal. The other siblings were not available for clinical examination, but reportedly were normal.
The child was discharged from the hospital at age 2 weeks, without surgical treatment, and was lost to follow-up.
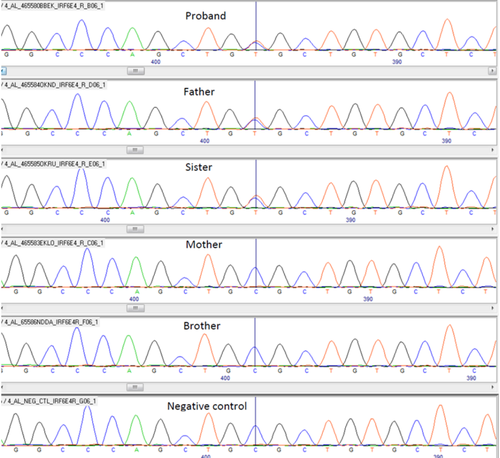
Genomic DNA was extracted from peripheral lymphocytes by the salt saturation method 15 at the genetic laboratory of Institut National de Recherche Biomédicale in Kinshasa. The exons 3 to 9 of the IRF6 were Sanger sequenced at the Center for Human Genetics of University of Leuven in Belgium. The primer sequences are available on request. Mutation analysis revealed that the index, his father and the affected sister carried a heterozygous missense mutation in the Exon 4, NM_006147.2:c.250C>T; p.Arg84Cys. The mother as well as the unaffected brother did not carry the mutation (Fig. 2).
Discussion
We report on three PPS patients from a Congolese pedigree. The index presented with a severe phenotype comprising malformations of oral region (cleft lip, syngnathia), skin (ankyloblepharon, pterygia, and skinfolds), extremities (oligosyndactyly), and genitalia (cryptorchidism). His sister had a moderate phenotype with skin defects (pterygia and unilateral pyramidal skinfold). The father was mildly affected and presented only with lower lip pits and a unilateral skinfold. The condition in this family shows a large variability both in terms of number and severity of abnormal features. Similar large intrafamilial variability was previously reported 6, 12, 16.
The only feature shared by the three affected individuals is the skinfold over toenail. It is suggested that the skinfold over the hallux is sufficiently pathognomonic to consider the diagnosis of PPS when it is associated with cleft lip and/or palate, even in the absence of a distinct popliteal pterygium [5, 11, 12]. Whereas lip pits have been observed in a small number of other syndromes (such as Kabuki and Simpson–Golabi–Behmel syndrome), the skinfold over the toe nail has only been reported in PPS thus far. Consistent with that suggestion, the skinfold over the toenail is associated with cleft lip in the index. In addition, the skinfold feature cosegregates with the IRF6 mutation in the current Congolese family. However, there are two different topographies for the skinfolds in this family: the classical position, that is, over the hallux's nail in the father and sister; and an unusual position in the index, on the second toenails. In addition, the shape of the skinfold in pyramidal only in the sister. This unusual topography and the variable shape add to the clinical variability reported so far in PPS.
The genetics of clinical variability in IRF6-related disorders is not fully understood. Genotype–phenotype correlations revealed that mutations causing PPS are mainly restricted in the highly conserved DNA-binding domain (exons 3 and 4), whereas those causing VWS are observed in both in- and out- of the DNA-binding domain, mostly in exons 3, 4, 7, and 9 2. In the present family, a recurrent missense mutation (c.250C>T; p.Arg84Cys) was resides in the DNA-binding domain. The p.Arg84Cys (rs121434226 C>T) mutation was previously associated with PPS in families of northern European descent 13. The present report further confirms previous genotype–phenotype associations observed in other populations. Also, recent genetic association studies suggested that mutations in FOXE1, TGFB3, and TFAP2A genes could influence condition's severity 14. Nongenetic modifiers had also been suggested 17. Clinical and genetic characterization of multiple VWS/PPS families from Central Africa will be useful in future association studies.
Thus far, this is the first molecularly confirmed PPS family to be reported from central Africa. This rarity may be explained in part by the large phenotype variability, which complicates diagnosis and delays genetic counseling. This is especially true in Africa where there is limited access to genetic testing.
Acknowledgment
The authors would like to thank members of the reported family for their cooperation. This work was made possible in part by a grant GOA/2012/015.
Conflict of Interest
None declared.