Global Trajectories of Colorectal Cancer Burden From 1990 to 2021 and Projection to 2040
Xiaolu Chen and Xuesi Dong contributed equally to this study.
ABSTRACT
Background
There is significant heterogeneity in patterns of colorectal cancer burden, which is still not well understood. This study examines global trajectories in the colorectal cancer burden, explores associated factors, and predicts future trends.
Methods
Data on the colorectal cancer burden for 204 countries and territories from 1990 to 2021 were sourced from the Global Burden of Disease Study. Growth mixture models identified subgroups of age-standardized incidence and mortality rates. Eleven modifiable risk factors and four socioeconomic determinants were analyzed across the subgroups. Trends to 2040 were predicted using a Bayesian age-period-cohort model.
Results
Three trajectories of colorectal cancer burden were observed: slowly increasing, rapidly increasing, and slowly decreasing age-standardized incidence rate, corresponding to stable, increasing, and decreasing mortality rate. Most countries showed slowly increasing incidence rates (49.0%, n = 100) and stable age-standardized mortality rates (51.0%, n = 104). Latin America and the Caribbean predominantly have a rapidly increasing trend (age-standardized incidence: 69.7%; mortality rates: 63.6%), while high-income countries largely followed decreasing trajectories (incidence: 58.3%; mortality: 75.0%). Higher sociodemographic index, universal health coverage, health expenditure, and gross domestic product per capita were linked to decreasing trends (all p < 0.05). Low consumption of whole grains and milk, and excessive red meat consumption, contributed significantly to colorectal cancer mortality. However, the impact of behavioral factors such as physical inactivity, smoking, and alcohol consumption was relatively small. Mortality attributable to high fasting blood sugar and body mass index is rising. Despite a slight global decline in mortality, disparities are projected to persist through 2040.
Conclusion
Global disparities in colorectal cancer burden highlight the need for targeted interventions, particularly focusing on dietary factors and health inequities.
Abbreviations
-
- ASIR
-
- age-standardized incidence rate
-
- ASMR
-
- age-standardized mortality rate
-
- BMI
-
- body mass index
-
- CRC
-
- colorectal cancer
-
- DALY
-
- disability-adjusted life-year
-
- GBD
-
- global burden of disease
-
- GDP
-
- gross domestic product
-
- GMMs
-
- growth mixture models
-
- PAF
-
- population attributable fraction
-
- TMREL
-
- theoretical minimum risk exposure level
1 Introduction
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of cancer-related deaths globally, with 1,926,425 new cases and 904,019 deaths reported in 2022 [1]. There are significant global geographical and sexual differences in CRC burden. Generally, the prevalence is higher in developed regions such as Australasia, Central Europe, and the high-income Asia Pacific region. Gender variations are less pronounced in regions such as South Asia and parts of Africa, including Eastern and Western Sub-Saharan Africa [2]. Socioeconomic status and regional differences in risk factor trends probably contribute to these differences. Approximately 70%–75% of CRC cases are sporadic, linked to intervenable factors, while 25%–30% are associated with unchangeable factors such as genetics [3, 4]. With the rising trends in modifiable factors such as poor diets, obesity, and smoking, alongside economic development, CRC incidence is increasing rapidly in some low- and middle-income countries [2, 5]. Importantly, the relative influence and distribution of the risk factors differ across regions. For instance, obesity contributed to 8% of global disability-adjusted life years (DALYs) but only 5% in Asia. Smoking accounted for 13% of DALYs globally but less than 5% in many African nations [6]. A thorough understanding of regional differences in CRC burden trends and their causes is therefore essential for designing targeted intervention strategies.
Researchers have largely focused on the consistency and variability in CRC trends across predefined socioeconomic and geographical subgroups, potentially overlooking substantial disparities [7]. For example, predefined subgroups may fail to account for time-varying disease trends or capture emerging patterns in the data. This study used the latest data from the Global Burden of Disease (GBD) study to analyze 32-year global CRC burden trajectories with growth mixture models (GMMs). These models group nations or regions by shared CRC burden trajectories over time, providing a data-driven approach that avoids overlapping correlated variables and enables dynamic, predictive analysis. It allows more accurate identification of emerging trends and better-targeted health interventions. However, very few studies have applied this data-driven method to examine disparities in CRC burden trends across countries. We also aimed to investigate potential socioeconomic determinants and key external risk factors driving changes in the burden of CRC during the past 32 years, and to predict the likely burden of disease by 2040.
2 Methods
2.1 Data Sources
Data on new cases, deaths, incidence rate, and mortality rate of CRC in 204 countries and territories from 1990 to 2021 were obtained from the Global Health Data Exchange query tool. Methods used in the GBD study have been previously described [8]. Briefly: (1) the mortality-to-incidence ratio (MIR) for CRC was calculated using data from cancer registries and the healthcare access and quality index; (2) mortality estimates were generated through cancer-specific cause of death ensemble models, incorporating data from vital registration systems, cancer registries, verbal autopsy reports, and factors such as smoking and alcohol use; and (3) CRC incidence was estimated by dividing mortality estimates by MIR values for each sex, location, year, and age group.
For each risk factor, the GBD study quantified the proportion of disease burden preventable if exposure levels were maintained at the theoretical minimum risk exposure level (TMREL). Population attributable fractions (PAFs) were calculated by comparing TMREL with actual exposure levels, assuming other risk factors remained constant. PAFs of risk factors to disease death were derived through comparative risk assessment [8]. Descriptions of 11 individual risk factors and their corresponding TMREL are shown in Supporting Information S1: Table S1.
The socio-demographic index from GBD 2021 captures regional income levels, educational attainment, and fertility rates. We used this to assess social development disparities across subgroups. Gross domestic product (GDP) per capita was measured by purchasing power parity international dollars in 2021 and served as an indicator of economic development. It was sourced from World Bank Data. Current health expenditure per capita in purchasing power parity international dollars was selected to measure average health spending per person, enabling international comparisons. We also used the universal health coverage service coverage index, reflecting the availability of effective healthcare and financial support [7]. Data for current expenditure and universal health coverage were taken from the WHO Global Health Observatory Data Repository for 2021. To ensure reliability, we opted for the most recent data with minimal missing rates.
Age-standardized rates in subgroups were calculated using the WHO world population standard. Projected population data by age group for 2021 to 2040 were drawn from the United Nations Economic and Social Council for 2024, and used to estimate cancer burden [9].
2.2 Statistical Analysis
2.2.1 GMMs
We used GMMs with random intercepts to analyze the CRC burden during the past 32 years [7]. ASIR and ASMR values obtained from GBD 2021 were transformed by Box–Cox transformation. To capture nonlinear trajectories, models included quadratic terms and random intercepts to address subgroup heterogeneity [10]. To assess the optimal number of subgroups, the model was fitted sequentially from one to five trajectory groups, with the best-fit model selected using goodness-of-fit measures including the Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC), along with the comprehensibility and average posterior probabilities of class membership. A better-fitting GMM was indicated by lower AIC and BIC values, and entropy values nearing 1. When entropy is around 0.8, it means that the classification accuracy has reached more than 90%. If the addition of a latent trajectory group resulted in only marginal improvement in fit statistics, we opted for the more parsimonious model [11]. Countries were assigned to subgroups on the basis of the highest posterior probabilities. Subgroup names were derived from a visual examination of the relative trends in the longitudinal trajectories. Sex-specific trajectory was analyzed, and we examined the distribution of different subgroups across the seven GBD super-regions based on cause-of-death patterns. These regions are as follows: (1) Central Europe, Eastern Europe, and Central Asia; (2) High-income countries; (3) Latin America and Caribbean; (4) North Africa and Middle East; (5) South Asia; (6) Southeast Asia, East Asia, and Oceania; and (7) Sub-Saharan Africa. High-income countries were mainly classified using World Bank criteria (2021 gross national income [GNI] per capita ≥ $13,205, Atlas method). The GBD study does not provide pre-aggregated trajectory group-level data, and thus, we implemented a population-weighted aggregation of country-level data to get the group-level aggregated values [7]. We used joinpoint regression (v5.4.0; National Cancer Institute, Maryland, USA) to test CRC burden trends with the metric of average annual percentage change [12]. Supporting Information S1: Table S2 shows a list of GBD 2021 countries and territories by GBD super-region.
2.2.2 Risk Factors and Socioeconomic Determinants
To explore the risk factors and socioeconomic determinants underlying CRC subgroups, we analyzed mortality attributable to 11 key risk factors across trajectory subgroups in 1990 and 2021. PAF of death within each latent subgroup was estimated by a weighted approach, with the weight being the proportion of CRC deaths in each country relative to the total CRC deaths in the subgroup. We also carried out sex-specific analysis of risk factors and used Boxplots to illustrate the relationships between the socioeconomic determinants and classified subgroups. We used the Wilcoxon rank-sum test with Bonferroni correction to assess the associations between subgroups and socioeconomic variables.
2.2.3 Bayesian Age-Period-Cohort Model
We projected the age-standardized rates for CRC incidence and mortality to 2040 following the Bayesian age-period-cohort model with integrated nested Laplace approximation [13]. This method is known for its lower absolute percentage deviation and has demonstrated good predictive accuracy. It has therefore been widely used [14]. CRC data were organized into 32 annual periods (1990–2021) and 18 5-year age intervals (0–4 to > 85 years). Population data were structured into 51 consecutive annual periods (1990–2040). To account for similar effects across adjacent time intervals, the second-order random walk prior was used to mitigate excessive dispersion by supposing a linear trend [15].
Analyses used R software (version 4.3.2, R Foundation for Statistical Computing, Vienna, Austria). Tests were two-tailed, with statistical significance set at p < 0.05. GMMs were implemented via the “lcmm” package [16]. The Bayesian age-period-cohort model was constructed using the “BAPC” and “INLA” packages [13].
3 Results
3.1 Worldwide CRC Trajectory Subgroups
From 1990 to 2021, the number of new CRC cases globally rose significantly from 916,600 to 2,194,100 (Table 1). During this period, the global ASIR increased by 0.206% annually (95% confidence interval [CI]: 0.152%–0.260%). ASIR trends varied significantly across countries, and three distinct trajectory subgroups were recognized based on model fit and interpretability (Supporting Information S1: Figure S1). Across outcomes, the AIC and BIC values continued to decrease with increasing number of classes, but a closer inspection showed diminishing returns in model interpretability and classification quality beyond the three-class solution. For ASIR analysis, the three-class model showed significantly better fit than the two-class model (BIC: −14705.06 vs. −13391.79), with optimal entropy (0.981) and balanced class distribution (49.0%/21.6%/29.4%). Four- and five-class models showed lower BIC values (e.g., 4-class BIC: −15593.41), but reduced entropy and small subgroups (12.2% and 6.9%), potentially compromising interpretability.
| Trajectory groupa | Number of countries (%) | 1990 | 2021 | 1990–2021 | ||
|---|---|---|---|---|---|---|
| N × 103 (95% UI) | ASR/100,000 (95% UI) | N × 103 (95% UI) | ASR/100,000 (95% UI) | AAPC (95% CI) | ||
| Incidence | ||||||
| Slowly increasing | 100 (49.0) | 282.9 (257.2, 308.3) | 18.8 (16.2, 21.9) | 628.0 (538.1, 715.8) | 19.1 (18.5, 27.2) | 0.074 (−0.068, 0.217) |
| Slowly decreasing | 44 (21.6) | 391.6 (359.7, 417.5) | 38.5 (28.8, 43.5) | 561.1 (497.4, 617.1) | 31.6 (24.1, 33.1) | −0.616 (−0.695, −0.536) |
| Rapidly increasing | 60 (29.4) | 240.9 (208.2, 276.4) | 15.4 (13.4, 17.1) | 1002.6 (815.2, 1207.5) | 25.2 (20.2, 29.6) | 1.617 (1.493, 1.742) |
| Global | 204 (100.0) | 916.6 (866.2, 951.9) | 24.0 (22.5, 25.0) | 2194.1 (2001.2, 2359.4) | 25.6 (23.3, 27.5) | 0.206 (0.152, 0.260) |
| Death | ||||||
| Stable | 104 (51.0) | 290.5 (255.4, 326.8) | 12.1 (10.5, 14.9) | 640.1 (529.7, 755.6) | 10.8 (9.9, 15.1) | −0.402 (−0.557, −0.247) |
| Decreasing | 44 (21.6) | 237.3 (215.0, 255.0) | 20.4 (19.2, 24.3) | 269.8 (231.8, 302.6) | 13.0 (12.0, 16.8) | −1.454 (−1.603, −1.306) |
| Increasing | 56 (27.4) | 41.6 (36.0, 48.1) | 8.3 (7.6, 11.7) | 132.8 (109.8, 157.1) | 10.7 (10.3, 15.7) | 0.854 (0.687, 1.021) |
| Global | 204 (100.0) | 570.3 (536.5, 597.7) | 15.6 (14.5, 16.3) | 1044.1 (950.2, 1120.2) | 12.4 (11.2, 13.3) | −0.717 (−0.804, −0.631) |
- Abbreviations: AAPC, average annual percentage change; ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; ASR, age-standardized rate; CI, confidence interval; UI, uncertainty interval.
- a 95% uncertainty interval of new cases, deaths, and ASR in each latent trajectory were generated using Monte Carlo simulation by assuming a log-normal distribution of age-standardized rates in each country and territory.
For ASMR analysis, the four-class model achieved the best statistical fit (BIC: −26,840.48, entropy 0.986), but we selected the three-class solution because it maintained high classification quality (entropy 0.982) with more balanced proportions (51.0%/21.6%/27.4%), avoiding the small class (7.8%) in the four-class model. Crucially, it ensured trajectory grouping alignment with ASIR classifications, enabling coherent cross-dimensional comparisons, whereas the four-class solution fragmented mortality patterns. Fit indices for one-to-five class solutions of the GMM analysis are shown in Supporting Information S1: Table S3.
Most countries and regions (49.0%, n = 100) showed a slow average increase in ASIR from 1990 to 2021 (slowly increasing group). Despite the slow rise, the absolute number of new cases grew from 282,900 in 1990 to 682,000 in 2021. Regions including South Asia (80.0%, n = 4), North Africa and the Middle East (66.7%, n = 14), Sub-Saharan Africa (65.2%, n = 30), Southeast Asia, East Asia, and Oceania (50.0%, n = 17), and Central Europe, Eastern Europe, and Central Asia (44.8%, n = 13) had a significant proportion of countries in this category (Table 2).
| Incidence (N, %) | Mortality (N, %) | ||||||
|---|---|---|---|---|---|---|---|
| Region | Number of countries | Slowly increasing | Slowly decreasing | Rapidly increasing | Stable | Decreasing | Increasing |
| Global | 204 | 100 | 44 | 60 | 104 | 44 | 56 |
| Central Europe, Eastern Europe, and Central Asia | 29 | 13 (44.8) | 7 (24.1) | 9 (31.0) | 16 (55.2) | 7 (24.1) | 6 (20.7) |
| High-income | 36 | 13 (36.1) | 21 (58.3) | 2 (5.6) | 9 (25.0) | 27 (75.0) | 0 (0.0) |
| Latin America and the Caribbean | 33 | 9 (27.3) | 1 (3.0) | 23 (69.7) | 9 (27.3) | 3 (9.1) | 21 (63.6) |
| North Africa and the Middle East | 21 | 14 (66.7) | 0 (0.0) | 7 (33.3) | 14 (66.7) | 2 (9.5) | 5 (23.8) |
| South Asia | 5 | 4 (80.0) | 1 (20.0) | 0 (0.0) | 5 (100.0) | 0 (0.0) | 0 (0.0) |
| Southeast Asia, East Asia, and Oceania | 34 | 17 (50.0) | 8 (23.5) | 9 (26.5) | 26 (76.5) | 3 (8.8) | 5 (14.7) |
| Sub-Saharan Africa | 46 | 30 (65.2) | 6 (13.0) | 10 (21.7) | 25 (54.3) | 2 (4.4) | 19 (41.3) |
The second subgroup, the slowly decreasing group (21.6%, n = 44), included countries and regions with a significant CRC burden during the 1990s, which gradually declined over time. However, these regions maintained the highest ASIR among the three categories, with 38.5/100,000 in 1990 and 31.6/100,000 in 2021, or 42.7% and 25.6% of new global cases in those years. This group was predominantly located in high-income regions (58.3%, n = 21).
The third subgroup, containing 60 countries and territories (29.4%), showed a rapid rise in ASIR (rapidly increasing group). Between 1990 and 2021, ASIR in these regions expanded by an average annual rate of 1.617% (95% CI: 1.493%–1.742%), increasing from 15.4/100,000 in 1990 to 25.2/100,000 in 2021. The absolute case number in this group surged by 316.2%, from 240,900 in 1990 to 1,002,600 in 2021. A large proportion of countries in Latin America and the Caribbean (69.7%, n = 23) fell into this group. Specific classification of countries and territories by trajectories in ASIR is shown in Supporting Information S1: Table S4.
The average predicted trajectory of ASMR mirrored the pattern of ASIR, although the group with slowly increasing incidence aligned with the stable mortality group (Supporting Information S1: Figure S2). A detailed classification of countries and territories by ASMR trajectories is shown in Supporting Information S1: Table S5. The largest trajectory group, representing 51.0% (n = 104) of countries, had relatively stable ASMR with an average annual percentage change of −0.402 (95% CI: −0.557, −0.247) (Table 1). A majority of countries in South Asia (100.0%, n = 5), Southeast Asia, East Asia, and Oceania (76.5%, n = 26), North Africa and the Middle East (66.7%, n = 14), Central Europe, Eastern Europe, and Central Asia (55.2%, n = 16), and Sub-Saharan Africa (54.3%, n = 25) were in this group (Table 2). The decreasing group, which contained 44 countries (21.6%), initially reported high ASMR but saw a decline from 20.4/100,000 in 1990 to 13.0/100,000 in 2021. By contrast, the increasing group (27.4%, n = 56) had low ASMR levels in the 1990s, but these rose considerably in subsequent decades. Over half of CRC deaths were observed in the stable group in both 1990 and 2021. The geographical pattern of ASMR trends was very similar to those for ASIR, with regions showing increasing ASMR predominantly in Latin America and the Caribbean (63.6%, n = 21), and those with decreasing ASMR mainly in high-income areas (75.0%, n = 27). For greater statistical power, sex-specific trajectory analyses are shown in Supporting Information S1: Figures S3–S6, with results aligned with overall population trends.
3.2 Risk Factors and Socioeconomic Determinants Between CRC Subgroups
Figure 1 shows the percentage of CRC deaths associated with modifiable factors in 1990 and 2021. Globally, low wholegrain intake remains the leading risk factor, accounting for 17.8% of deaths, followed by low milk intake (15.1%) and high red meat intake (14.6%). Diets low in fiber contributed the least (1.3%). The global proportion of deaths linked to high fasting plasma glucose and high body mass index (BMI) has increased significantly, with the former rising from 5.7% to 7.9% (a 38.6% increase) and the latter from 7.3% to 9.5% (a 30.1% increase) from 1990 to 2021. Behavioral factors, including physical inactivity, smoking, and alcohol consumption, contributed less, ranging from 4.4% to 7.0% in 2021. The proportion of deaths attributable to low milk (10.0%) and low calcium (4.0%) intake was the lowest in the decreasing group, while high BMI accounted for the highest proportion at 12.7% in 2021. The distribution of attributable proportions for various risk factors in the stable group closely resembled the global analysis. Low calcium-related mortality was highest in 2021 in the increasing group, despite a decline from 20.6% in 1990 to 16.2% in 2021. Other risk factors, such as insufficient fiber intake, showed no substantial variation across groups. The trend in risk factor attribution for men and women mirrored the global trend (Supporting Information S1: Figures S7 and S8), with men having higher risk from smoking and alcohol, and women from insufficient milk and calcium intake, high BMI, and low physical activity.
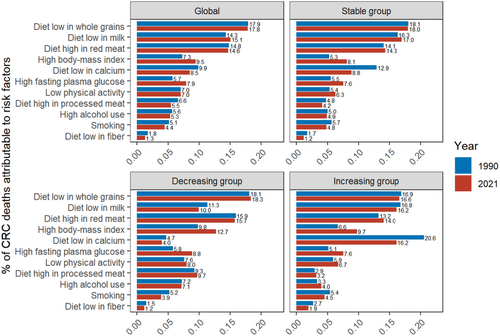
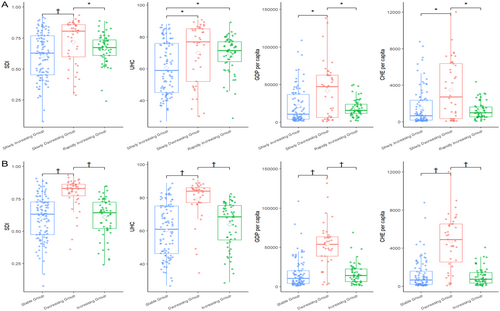
Figure 2 shows the comparison of socioeconomic indicators across different trajectory subgroups. The distribution of socioeconomic indicators in the slowly increasing, slowly decreasing, and rapidly increasing ASIR subgroups is aligned with the stable, decreasing, and increasing ASMR subgroups. Nations experiencing declining cancer burden generally had better socio-demographic index, universal health coverage, GDP per capita and current health expenditure per capita (all p < 0.05), showing significant differences from the other groups. Countries in the rapidly increasing group had slightly better socioeconomic conditions than those in the slowly increasing group, but for most indicators, the differences between the two groups were not statistically significant.
3.3 Projection of CRC Burden to 2040
Figure 3 shows the projected CRC rates by trajectory subgroups from 1990 to 2040, with continued variations in burden. Globally, ASIR is projected to rise from 26.4/100,000 in 2022 to 27.2/100,000 by 2040. After 2022, a gradual decline is anticipated in the slowly increasing group, with the incidence rate projected to reach 15.5/100,000 by 2040. The ASIR trends in the decreasing group are expected to converge toward the global average, reaching an estimated 24.5/100,000 by 2040. The rapidly increasing group is predicted to show a notable and significant rise. From 2022 to 2040, the ASIR of this group is expected to increase from 27.0/100,000 to 36.3/100,000, approximately 34.4%.
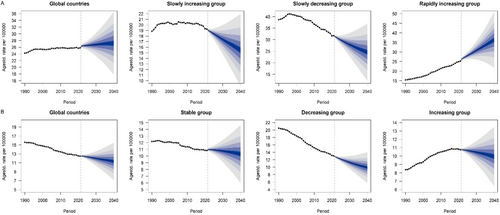
Global ASMR is projected to decrease from 12.6/100,000 in 2022 to 11.3/100,000 in 2040. The stable group is expected to drop slightly from 11.0/100,000 in 2022 to 10.3/100,000 in 2040. The ASMR of the decreasing group is projected to drop significantly from 12.8/100,000 in 2022 to 9.9/100,000 by 2040, a reduction of approximately 22.7% between 2022 and 2040. Even in the increasing group, ASMR is projected to reverse and gradually decrease to 9.9/100,000 by 2040.
4 Discussion
Our research offers a detailed yet succinct overview of the evolving trends in CRC dynamics. Globally, three distinct patterns of ASIR for CRC have been identified: slowly increasing, slowly decreasing, and rapidly increasing groups. These trends correspond to patterns categorized as stable, decreasing, and increasing ASMR. The majority of countries have a slowly increasing ASIR and a stable ASMR. Countries with decreasing ASIR generally have higher socioeconomic status. Over the study period, there was a significant rise in the global mortality rate linked to elevated fasting plasma glucose and increased BMI, but behavioral risk factors (smoking, drinking, low physical activity) had less impact. Insufficient intake of wholegrains and milk, and excessive consumption of red meat, are the main risk factors, and the global CRC burden is expected to remain serious in the future.
Consistent with previous research, we found that the CRC burden is declining in mostly affluent countries such as Australia, the United States, and the United Kingdom. Since the 1970s, these countries have seen decreasing or stabilizing CRC rates [17], largely attributed to effective screening programs [18]. For example, in the United States, CRC screening guidelines introduced in 1997 [19] led to an increase in screening uptake from 38% in 2000 to 66% in 2018 [20]. This was accompanied by declines in CRC incidence and mortality (average annual percentage change −0.69 and −1.05) during 2000 and 2019, highlighting the positive impact of screening initiatives [21]. However, despite these trends, the incidence and mortality rates remained above the global average, mainly due to unhealthy lifestyles.
We found increasing CRC incidence and mortality in low- and middle-income countries, especially in Latin America and the Caribbean (69.7% of ASIR and 63.6% of ASMR globally). From 1990 to 2019, CRC-adjusted mortality in Latin America rose by 20.56% (95% CI: 19.75%–21.25%) [22], consistent with our findings. This trend is probably driven by Westernized lifestyles, rising obesity rates, unhealthy diets, and limited access to effective screening. The lack of resources for sustainable national programs has resulted in limited studies on CRC screening in Latin America. There are a few organized screening initiatives in low- and middle-income countries such as Honduras, Guatemala, and Bolivia. Meanwhile, in upper-middle-income nations such as Brazil and Chile, CRC prevalence rates are consistent with those observed in high-income countries [23]. Notably, only 1.3% of people with CRC in low-income countries and 3.1% in middle-income countries received radiotherapy, far below the ideal rates of 14% and 61% [5, 24]. Untimely healthcare, cultural beliefs, and financial barriers, especially in rural areas, further contribute to the high mortality in this region [5].
In Asia (except high-income Asia-Pacific countries such as Singapore and the Republic of Korea), Africa, and Oceania (except Australasia), CRC incidence is slowly rising and mortality remains stable, in line with previous studies [2]. Trend discrepancies between the trajectory model and joinpoint annual average percentage changes may be explained by nonlinear patterns in GMM and piecewise linear approximations in joinpoint regression. The “slowly increasing” incidence group shows a near-zero AAPC (0.074%, 95% CI: −0.068 to 0.217), suggesting a recent plateau despite a long-term upward trend. Similarly, the “stable” mortality group presents a mild decline (AAPC: −0.402%, 95% CI: −0.557 to −0.247), which may not be sufficient to shift its overall classification in the trajectory model. A multi-country and multi-center study covering at least 12 years in sub-Saharan Africa showed a steady rise in CRC, possibly due to wider exposure to risk factors through unhealthy lifestyles [25]. The epidemiology of CRC has transformed in recent decades, driven by economic globalization, environmental factors, and evolving dietary habits. Southeast Asia has experienced marked lifestyle shifts, including a growing reliance on animal-based diets and reduced physical activity, contributing to increased risk of CRC [26]. In 2019, the North Africa and Middle East region had the lowest CRC burden among the GBD super-regions [27]. However, many countries in Asia and sub-Saharan Africa lack comprehensive cancer registries, potentially underestimating the burden [28].
Countries with decreasing ASIR or ASMR generally had higher socio-demographic index, universal health coverage, GDP per capita, and current health expenditure per capita (all p < 0.05), highlighting associations between better economic status and healthcare access, and improved CRC outcomes. Previous research also showed a strong association between cancer burden and socioeconomic development [29]. Income inequality may increase CRC burden through screening disparities, healthcare access limitations, and behavioral risks. Each 0.1-unit Gini coefficient (which reflects the deviation from a line of perfect income equality) rise correlates with 11% higher CRC incidence and mortality, especially in rural areas [30]. In Ontario, 71.6% of screening inequality stemmed from income, in addition to education and language barriers [31]. Lower-income patients face longer diagnostic delays owing to both patient-level (competing priorities, transportation) and systemic factors [32]. Health behaviors and BMI collectively mediate 36.2% of socioeconomic CRC risk [33]. Similarly, inadequate healthcare resource allocation, particularly in socioeconomically deprived areas, can result in diagnostic delays and poorer treatment outcomes [32]. These results highlight the significant impact of socioeconomic factors on global CRC burden. Despite similar macro-level indicators (current health expenditure, socio-demographic index) in the rapidly and slowly increasing groups, divergent CRC trends suggest underlying structural differences. National averages obscure subnational disparities in healthcare access and spending priorities (treatment vs. prevention). Unmeasured factors such as healthcare quality, policy implementation, and health literacy, combined with rapid behavioral changes outpacing health system capacity, highlight the need for context-specific CRC strategies beyond aggregate indicators.
Our findings are generally consistent with previous work, identifying low intake of wholegrains (17.8%) and milk (15.1%), and high red meat intake (14.6%), as leading global CRC mortality risk factors in 2021. Supporting evidence showed that CRC risk is reduced by 17% for each 90 g/day of whole grains intake, probably through gut microbiota modulation and anti-inflammatory effects [34]. Regional consumption varies widely, with the highest intakes reported in parts of Southeast Asia because of traditional diets and the lowest in Central Europe, where diets are dominated by refined starches [35]. A previous study found that people consuming at least 250 g/day of milk had a 15% lower risk of CRC than those consuming less than 70 g [36]. The mechanism behind this is not known, but one possibility is that the high calcium content of milk may contribute [37]. A strong correlation between milk and calcium intake (r = 0.71) has been observed [38]. CRC mortality attributable to low milk and calcium intake was highest in the increasing group and lowest in the decreasing groups, consistent with East Asia's documented high burden from dairy deficiencies [39]. Asian countries tend to consume less milk than European and American countries [40]. We found that women have a higher CRC risk from insufficient milk intake, probably due to gender-specific metabolic and hormonal differences, particularly postmenopausal declines in estrogen, which may exacerbate calcium deficiency [41]. Red meat intake, a known CRC risk factor, generates carcinogens during cooking and induces oxidative stress via heme iron. Consumption varies regionally, being highest in Western nations versus Asia [42].
We found a growing proportion of the burden caused by metabolic factors, such as high fasting plasma glucose and high BMI, with behavioral factors, such as physical activity, smoking, and drinking, accounting for only a small proportion. Globally, high BMI accounted for just 8.3% of DALYs, with higher percentages in regions like Central Europe (14.0%) and high-income North America (13.8%). The specific mechanism is unclear, but excessive fat accumulation, as reflected by high BMI, may interact adversely with CRC treatment [43]. CRC mortality linked to high fasting plasma glucose rose significantly in most countries, particularly developing nations [44]. Smoking prevalence declined steadily in high-income countries but remained stable or reduced only minimally in low- and middle-income countries. Our study found smoking and alcohol contributed less to CRC burden than expected, potentially because (1) mortality from COVID-19 may have attenuated risk factor impact (though not quantified in GBD 2021), and (2) effective public health policies improved risk factor control [45]. These findings are consistent with GBD 2021 analyses showing behavioral risks play a modest role in CRC burden [46]. The combined effect of diet (excluding alcohol and body fat) is estimated to explain 38% of CRC cases in women and 45% in men. Region- and sex-specific health promotion campaigns can significantly lower CRC risk [43].
From 1990 to 2021, global CRC cases and deaths more than doubled. ASIR showed a slight increase, but ASMR showed a decrease [47]. In Asia (with the exception of high-income areas such as Singapore and the Republic of Korea), Africa, and Oceania (excluding Australasia), the ASIR is projected to decline over the coming decades. This may be attributable to gradual improvements in healthcare infrastructure, increasing public awareness, early detection efforts, and shifts in exposure to key risk factors. Meanwhile, ASMR in these regions has remained stable or declined slightly, probably reflecting modest advancements in treatment accessibility and quality. Projections suggest that globally, ASIR will rise by 8.15% to 145.82 per 100,000 population by 2040, with Andean Latin America expected to see the most dramatic increase (an estimated rise of 106.2%). This is consistent with our finding that countries in Latin America and the Caribbean are predominantly in the rapidly increasing group. A previous study suggested that most countries in Asia, Europe, North America, and Oceania are expected to continue experiencing declines in ASMR to 2035, in contrast with potential increases projected for Latin America and the Caribbean [48]. This divergence may be mainly due to persistent inequalities in healthcare access, delayed implementation of screening programs, and slower improvements in risk factor control across parts of Latin America and the Caribbean. By contrast, many developed nations are projected to see continuous decreases in both ASIR and ASMR during this period [26], reflecting the long-term effectiveness of comprehensive screening initiatives, early intervention programs, and sustained public health efforts targeting modifiable risk factors. Nevertheless, despite anticipated declines in ASIR in some regions, the overall global burden of CRC is expected to continue to rise, driven largely by population growth and aging.
4.1 Strengths
Our study has several strengths. To our knowledge, this study is the first to explore global CRC transition patterns during this 32-year period using a data-driven categorization method and GMMs. This approach facilitated the validation and extension of the cancer transitions theory by analyzing the uniformity and diversity in the shifts of CRC burden across different nations. This method moves beyond the commonly used traditional geographic or socioeconomic stratifications [5, 49] and instead provides a feature-based spectrum of CRC evolution. We leveraged the most recent GBD data to conduct a comprehensive long-term analysis. We also highlighted variations in socioeconomic determinants and modifiable risk factors between different subgroups using indicators from previous studies. Finally, we projected future CRC burdens with different trajectories.
4.2 Limitations
This study also had several limitations. First, the reliability of GBD statistics depends on data quality. Despite efforts to improve data collection and modeling, results should be interpreted cautiously, particularly for countries with limited resources. PAF calculations rely on the TMREL, derived from the lowest exposure levels documented in current studies, but future large-scale trials may reveal even lower levels, potentially introducing biases in forecasting CRC burdens. Potential residual confounding from unmeasured variables (e.g., socioeconomic status, lifestyle) in diet-related CRC mortality attribution may exist, despite using TMREL and meta-analyzed cohort studies adjusted for key confounders. Second, the group-based method in GMMs may oversimplify the true variability of the data, but it provides balanced transition modeling when rigorously applied. Our three-class system and 32-year data may not capture all nuances, but they offer meaningful differentiation and actionable insights for CRC control.
5 Conclusion
CRC rates have shown diverse global trends over the past 32 years. Three trajectories were identified: slowly increasing, slowly decreasing, and rapidly increasing ASIR, corresponding to stable, decreasing, and increasing ASMR, respectively. Decreases were mainly in high-income regions and increases mainly in low and middle-income regions. Low intake of whole grains and milk, and high red meat consumption were key common risk factors. The global disease burden is projected to remain serious in the future.
Author Contributions
Xiaolu Chen: investigation (equal), methodology (equal), visualization (equal), writing – original draft (equal). Xuesi Dong: investigation (equal), methodology (equal), visualization (equal), writing – original draft (equal). Yadi Zheng: writing – review and editing (equal). Chenran Wang: writing – review and editing (equal). Zilin Luo: writing – review and editing (equal). Jiaxin Xie: writing – review and editing (equal). Zeming Guo: writing – review and editing (equal). Xiaoyue Shi: writing – review and editing (equal). Xinyue Zhu: writing – review and editing (equal). Yongjie Xu: writing – review and editing (equal). Wei Cao: writing – review and editing (equal). Fei Wang: writing – review and editing (equal). Ni Li: writing – review and editing (lead).
Acknowledgments
We acknowledge the contributions of the Global Burden of Disease (GBD) 2021 study.
Ethics Statement
This study adhered to the guidelines for accurate and transparent health assessment reporting. Since publicly accessible data were used, ethical approval was not required for this study.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The datasets generated and/or analyzed here are available in the GBD 2021 repository (http://ghdx.healthdata.org/gbd-results-tool).