18F-FDG PET/CT findings of paratesticular alveolar rhabdomyosarcoma
Xueqi Chen and Jiayin Shou contributed equally to this study and shared the first authorship.
Abstract
Rhabdomyosarcoma (RMS) originates from primitive mesenchymal cells and is the most common soft tissue tumor in childhood. 18F-fluoro-deoxyglucose (18F-FDG) positron emission tomography (PET)/computed tomography (CT) has been reported to be valuable in RMS staging and risk stratification. Paratesticular RMS is a relatively uncommon form of RMS, most of which are of the embryonal histologic type. Paratesticular alveolar RMS is associated with aggressive behavior, high metastatic potential, and poor outcomes. To the best of our knowledge, 18F-FDG PET/CT imaging findings of paratesticular alveolar RMS have never been described. Here, we report on a 16-year-old boy's rare paratesticular alveolar RMS with multiple metastases and its findings on 18F-FDG PET/CT. This case also demonstrates the potential value of 18F-FDG PET/CT in RMS staging and treatment decisions, and may aid in the differential diagnosis.
Abbreviations
-
- 18F-FDG
-
- 18F-fluoro-deoxyglucose
-
- PET/CT
-
- positron emission tomography/computed tomography
-
- RMS
-
- rhabdomyosarcoma
1 BACKGROUND
Rhabdomyosarcoma (RMS) originates from primitive mesenchymal cells, and is the most common soft tissue tumor in childhood, accounting for approximately half of all soft tissue sarcomas in this age group [1]. According to the World Health Organization (WHO) 2020 classification of soft tissue and bone tumors, RMS can be classified into four main histologic types: embryonal, alveolar, pleomorphic, and spindle/sclerosis subtypes. RMS occurs primarily in the head and neck, genitourinary tract, and extremities [1]. Paratesticular RMS develops from the spermatic cord, epididymis, and testicular capsule and accounts for 7% to 10% of cases of genitourinary RMS (23% of all RMS). Among them, the most common pathological subtype is embryonal variation (approximately 80%) [2]. Paratesticular RMS has a bimodal age distribution, peaking at 1 to 5 years of age and then at 16 years [3]. Treatment of paratesticular alveolar RMS includes surgery, multiagent chemotherapy, and radiation therapy [2]. Paratesticular alveolar RMS is rare and may be associated with aggressive behavior, high metastatic potential, and poor prognosis [4]. Here, we present a rare case of paratesticular alveolar RMS with distant metastases and its findings on 18F-fluoro-deoxyglucose (18F-FDG) positron emission tomography (PET)/computed tomography (CT).
2 CASE STUDY
A 16-year-old boy presented with a 1-month of history of painless scrotal swelling. Ultrasonography revealed a solid paratesticular mass and multiple enlarged inguinal lymph nodes. Laboratory tests showed elevated serum creatinine (809.3 µmol/L, reference range 44–133 µmol/L), uric acid (1117 µmol/L, reference range 90–360 µmol/L), LDH (1691 IU/L, reference range 100–240 IU/L), and normal alpha-fetoprotein and beta-human chorionic gonadotropin levels.
An 18F-FDG PET/CT was performed to investigate the paratesticular mass, distant metastases, or potential malignancy of disease extent. The maximal intensity projection (MIP) image showed a strong uptake of 18F-FDG in the scrotum, multiple lymph nodes in the left supraclavicular area, right hilum, abdomen, and bilateral inguinal region. Slight heterogeneity was observed in multiple vertebral bodies with 18F-FDG-affinity. Coronal CT images, corresponding PET, and fused PET/CT revealed 18F-FDG accumulation in the lymph nodes in the left supraclavicular, right hilum, and retroperitoneal region. The para-aortic and iliac lymph nodes were severely enlarged and fused and showed the most active FDG affinity (SUVmax 7.5). On axial CT image, the paratesticular soft tissue mass (measured 12.2 cm × 9.0 cm × 8.4 cm) was posterior to the testis with a well-defined marginal border. The corresponding PET and fusion PET/CT revealed increased 18F-FDG activity with an SUVmax of 6.0 (Figure 1).
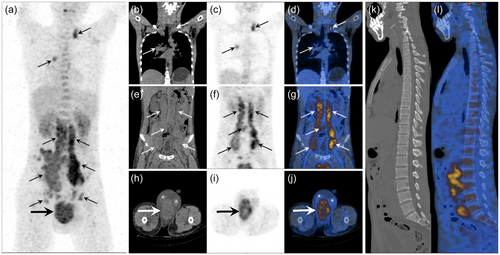
PET/CT findings suspected paratesticular malignancy with multiple metastases or extensive lymphoma involvement, while ultrasound-guided core needle biopsy histopathologically showed paratesticular alveolar RMS and fluorescence in situ hybridization (FISH) showed positive FOXO1 mutations. The clinical diagnosis of multiple lymph nodes and bone metastases was based on a comprehensive diagnostic evaluation that included PET/CT findings.
3 DISCUSSION
Alveolar RMS accounts for 15% of cases, tends to occur in older children, and has a worse prognosis compared with embryonal RMS. At the molecular level, most alveolar RMSs have a characteristic fusion of the PAX3 or PAX7 genes with FOXO1, which is caused by a specific chromosomal translocation [3]. In this setting, the presence of FOXO1 rearrangements identified by FISH or reverse-transcriptase polymerase chain reaction supports the diagnosis of alveolar RMS.
Imaging is important for the diagnosis and evaluation of RMS, including assessment of tumor spread, lymph node involvement, and distant metastases. Ultrasound, CT, and magnetic resonance imaging (MRI) have been widely used in the evaluation of RMS. Ultrasound can be used as an initial examination, particularly in the evaluation of scrotal masses. Patients typically present with a painless hypoechoic scrotal mass and a solid, heterogeneous extratesticular mass on ultrasound [2]. CT has advantages in detecting pulmonary nodules and assessing bone involvement [3, 5]. MRI is considered the best imaging modality for most primary RMS with moderate to high intensity on T1-weighted and T2-weighted images [6]. However, radiographic findings of RMS are largely nonspecific. 18F-FDG PET/CT has been reported to be of great value in RMS staging and risk stratification, and is also used to detect unknown primary sites or sites of rare metastases, treatment decisions, prognostic prediction, and treatment response evaluation [7, 8].
Although the superficial location of paratesticular RMS facilitates early diagnosis, previous studies have shown that lymph node involvement is more common in patients with paratesticular RMS older than 10 years of age [5]. Therefore, these patients require special attention to lymph node evaluation. Although 18F-FDG PET/CT may have advantages in identifying lymph node involvement compared with conventional imaging, with higher sensitivity for a single positive node and fewer uncertain results [9], 18F-FDG PET/CT may present more closely to lymphoma in RMS [10]. Therefore, the accurate diagnosis of lymphatic metastases relies on biopsy core needle biopsy or resection rather than PET/CT [5]. In this case, ultrasound-guided core needle biopsy results confirm paratesticular alveolar RMS and positive FOXO1 mutations.
4 CONCLUSION
We present a rare case of paratesticular alveolar RMS with distant metastases, demonstrating the potential value of 18F-FDG PET/CT in the staging and treatment decisions of RMS. Further exploration is warranted to validate the differential diagnostic value of malignancies with similar presentations and to explore the clinical prognostic potential of 18F-FDG in larger studies.
AUTHOR CONTRIBUTIONS
Xueqi Chen: Conceptualization (equal); data curation (lead); investigation (equal); methodology (equal); writing—original draft (equal). Jiayin Shou: Conceptualization (equal); investigation (equal); methodology (equal); writing—original draft (equal). Shanshi Li: Data curation (supporting); investigation (supporting); methodology (supporting); writing—original draft (supporting). Yan Fan: Conceptualization (equal); data curation (lead); funding acquisition (equal); investigation (equal); methodology (equal); supervision (equal); writing—review and editing (equal). Jianhua Zhang: Conceptualization (equal); data curation (lead); funding acquisition (equal); investigation (equal); methodology (equal); supervision (equal); writing—review and editing (equal).
ACKNOWLEDGMENTS
We thank Dr. Qi Shen from Department of Urology, Peking University First Hospital for the interpretation of the pathological result.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Not applicable.
INFORMED CONSENT
Written informed consent was obtained from the patient's next of kin for publication of this case study and accompanying images.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




