Longitudinal effect of eteplirsen versus historical control on ambulation in Duchenne muscular dystrophy
Collaborators in the DMD Italian Network and Eteplirsen Study Group and their affiliations are available as an online supplementary file.
Abstract
Objective
To continue evaluation of the long-term efficacy and safety of eteplirsen, a phosphorodiamidate morpholino oligomer designed to skip DMD exon 51 in patients with Duchenne muscular dystrophy (DMD). Three-year progression of eteplirsen-treated patients was compared to matched historical controls (HC).
Methods
Ambulatory DMD patients who were ≥7 years old and amenable to exon 51 skipping were randomized to eteplirsen (30/50mg/kg) or placebo for 24 weeks. Thereafter, all received eteplirsen on an open-label basis. The primary functional assessment in this study was the 6-Minute Walk Test (6MWT). Respiratory muscle function was assessed by pulmonary function testing (PFT). Longitudinal natural history data were used for comparative analysis of 6MWT performance at baseline and months 12, 24, and 36. Patients were matched to the eteplirsen group based on age, corticosteroid use, and genotype.
Results
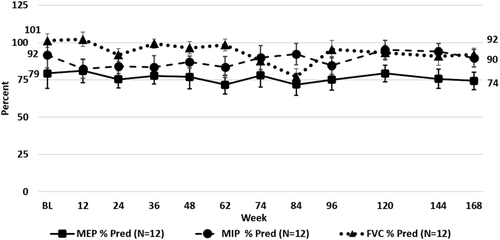
At 36 months, eteplirsen-treated patients (n = 12) demonstrated a statistically significant advantage of 151m (p < 0.01) on 6MWT and experienced a lower incidence of loss of ambulation in comparison to matched HC (n = 13) amenable to exon 51 skipping. PFT results remained relatively stable in eteplirsen-treated patients. Eteplirsen was well tolerated. Analysis of HC confirmed the previously observed change in disease trajectory at age 7 years, and more severe progression was observed in patients with mutations amenable to exon skipping than in those not amenable. The subset of patients amenable to exon 51 skipping showed a more severe disease course than those amenable to any exon skipping.
Interpretation
Over 3 years of follow-up, eteplirsen-treated patients showed a slower rate of decline in ambulation assessed by 6MWT compared to untreated matched HC. Ann Neurol 2016;79:257–271
This paper reports on results of continuous, 3-year treatment of Duchenne muscular dystrophy (DMD) patients with eteplirsen, a 30-nucleotide-long phosphorodiamidate morpholino oligomer (PMO) that induces skipping of exon 51 in DMD pre-mRNA. The etiology of this rare but devastating disease, the eteplirsen mode of action, and the course of the clinical studies (studies 201/202) have been described in detail in an earlier publication1 and in several reviews.2-4 Briefly, DMD is caused by deletions and other mutations in the dystrophin (also known as DMD) gene that abrogate the mRNA reading frame and prevent expression of dystrophin protein. As a result, affected newborn boys experience severe, progressive neuromuscular impairment starting in early childhood,5 typically lose ambulation in their midteens, and succumb to respiratory failure or cardiomyopathy by their mid-20s.3, 6-8 Eteplirsen-induced skipping of exon 51 restores the mRNA reading frame, allowing production of an internally deleted but functional dystrophin protein. This is supported by the finding that internally deleted dystrophin proteins occur in patients with Becker muscular dystrophy, a dystrophinopathy allelic to DMD, but with a less severe phenotype.9 The ability of eteplirsen to induce expression of dystrophin in DMD patients was demonstrated by an observed increase of dystrophin-positive fibers in skeletal muscle, observed increases in dystrophin intensity in this1 and other studies,10, 11 and by the observed restoration of the dystroglycan complex, as evidenced by localization of neuronal nitric oxide synthase and B-dystroglycan to the sarcolemma.12
The ability of eteplirsen to confer clinical benefit in study 201, a randomized, placebo-controlled study, and study 202, its ongoing open-label extension, was primarily evaluated by the 6-Minute Walk Test (6MWT). The 6MWT is an ambulatory outcome measure that has been utilized in clinical trials for 3 DMD therapeutics (eteplirsen, drisapersen, and ataluren) and has been shown to be accurate and reproducible.13 Understanding of DMD disease progression as measured by 6MWT has increased in recent years with publications of natural history data14-19 as well as placebo-arm reporting from DMD trials.20-22 Published data support that on average, 6MWT distance is stable or increases in patients <7 years of age, whereas it declines in older patients.15, 17, 18, 23, 24 Evidence also suggests that DMD genotype may influence disease severity.25
Given that there is no control group in the open label, long-term extension study, eteplirsen's effect on disease progression as measured by 6MWT was evaluated by comparison to matched historical controls from 2 DMD natural history cohorts: the Leuven Neuromuscular Reference Center (LNMRC) and the Italian Telethon registry.15, 26 These 2 investigator-initiated studies are the only DMD natural history data sets that have prospectively and consistently collected 6MWT assessments for a substantial number of patients for 36 months or longer. Comparability to the eteplirsen data set is supported by equivalent requirements across the studies for genetic confirmation of DMD diagnosis, patient care according to the same international treatment guidelines for DMD,27, 28 6MWT administration following generally accepted standards,13, 29, 30 and exclusion of patients with cognitive impairment that could interfere with test adherence. Patient-level data from the registries were pooled, and analysis was performed to evaluate impact of genotype on disease natural history as well as to compare an appropriately matched historical control group to eteplirsen-treated patients.
The ability of eteplirsen to confer clinical benefit was secondarily evaluated by pulmonary function testing. Because long-term matched patient-level natural history data were not available, eteplirsen-treated patients were compared to published data31, 32 in a DMD population.
Patients and Methods
Patients
Eteplirsen studies 4658-201/202 were approved by the relevant institutional review boards prior to implementation, and informed consent/assent was obtained from each subject and family prior to enrollment. Patients eligible for this study were 7 to 13 years old, were able to walk 180 to 440m on the 6MWT, had confirmed out-of-frame dystrophin deletion mutations amenable to exon 51 skipping, and were on stable corticosteroid therapy for ≥24 weeks (Tables 1 and 2).
| Demographic | All Patients, N = 12 |
|---|---|
| Age, yr | |
| Mean (SD) | 9.3 (1.22) |
| Median | 9.7 |
| Min, Max | 7, 11 |
| Height, cm | |
| Mean (SD) | 123.7 (8.40) |
| Min, Max | 116, 138 |
| Weight, kg | |
| Mean (SD) | 31.52 (6.411) |
| Min, Max | 22.1, 39.8 |
| Time since DMD diagnosis, mo | |
| Mean (SD) | 56.4 (26.40) |
| Median | 57.0 |
| Min, Max | 18, 112 |
- Age, height, weight, and time since diagnosis are shown for the 12 eteplirsen-treated patients at baseline.
- Max = maximum; Min = minimum; SD = standard deviation.
| All Patients, N = 12 | ||
|---|---|---|
| Characteristic | Baseline | Month 36 |
| 6MWT,a m | ||
| No. | 12 | 12 |
| Mean | 363.2 | 263.1 |
| SD (SE) | 42.19 (12.18) | 151.74 (43.80) |
| Min, Max | 256, 416 | 0, 483 |
| MIP, % predicted | ||
| No. | 12 | 12 |
| Mean | 91.7 | 89.5 |
| SD (SE) | 29.98 (8.65) | 20.53 (5.93) |
| Min, Max | 50, 145 | 60, 133 |
| MEP, % predicted | ||
| No. | 12 | 12 |
| Mean | 79.3 | 74.3 |
| SD (SE) | 34.80 (10.04) | 20.02 (5.78) |
| Min, Max | 37, 147 | 41, 99 |
- 6MWT distance and percentage of predicted MIP/MEP are shown for eteplirsen-treated patients at baseline and month 36.
- a Based on day 1 distance when there were 2 consecutive days of testing.
- 6MWT = 6-Minute Walk Test; Max = maximum; MEP = maximum expiratory pressure; Min = minimum; MIP = maximum inspiratory pressure; SD = standard deviation; SE = standard error.
Study Design
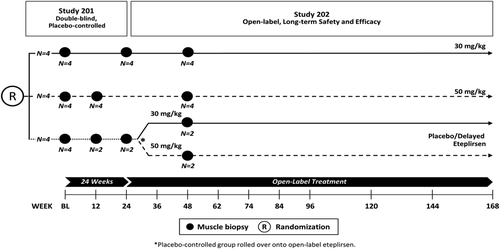
As described previously,1 patients were randomly assigned to 3 cohorts (n = 4 each) in a double-blind fashion and received weekly intravenous (IV) eteplirsen 30mg/kg or 50mg/kg or placebo for 24 weeks (Fig 1). Thereafter, patients who had received eteplirsen continued at the same dose on an open-label basis, whereas those patients who had received placebo were randomized 1:1 to weekly 30mg/kg or 50mg/kg eteplirsen on an open-label basis.
All infusions and assessments were performed at Nationwide Children's Hospital through the double-blind phase and thereafter until a study site geographically closer to the patient was initiated. Collections of adverse events, concomitant medication, vital signs, weight, and laboratory assessments were performed at these sites. All functional assessments continued to be performed at Nationwide Children's Hospital by the same evaluators to ensure consistency.
Evaluations
All functional measures were assessed at least semiannually. The 6MWT33 was administered once, or twice on consecutive days, according to predetermined schedules outlined in the protocol, with each patient following the same schedule. When the 6MWT was administered on 2 consecutive days, the day 1 results were used for this analysis for comparison to matched controls who had 1 value for each time point. Pulmonary function testing (PFT) was performed at each functional assessment visit and included maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP), and forced vital capacity (FVC). Up to 5 efforts were allowed, and the best effort results were used for analysis. Results were converted to percentage of predicted values employing the widely used methodologies of Wilson et al34 for MIP and MEP and Polgar and Varuni35 for FVC.
Safety Assessments
Safety assessments included adverse event monitoring and clinical laboratory evaluation with special emphasis on events commonly observed with other oligonucleotide therapeutics such as inflammatory events, coagulopathies, and hepatic and renal toxicity. Safety laboratory assessments were performed at scheduled visits, and adverse events were continuously monitored.
Patients' Natural History Data
Patient-level historical control data were provided by E.M. on behalf of the Italian DMD Registry database,26 and N.G.15
The Italian DMD Registry includes patient data from 11 neuromuscular care centers in Italy (Catholic University of Rome, Rome; University of Messina, Messina; Infant Jesus Hospital, Rome; Mondino Institute, Pavia; Gaslini Institute, Genoa; Besta Institute, Milan; Stella Maris Institute, Pisa; Greater Hospital, Bologna; University of Naples, Naples; University of Turin, Turin; University of Padua, Padua; University of Milan, Milan). The patients in N.G.'s registry attended LNMRC for clinical care and management.
All patients in the 2 investigator-initiated studies (historical control group) had a genetically confirmed diagnosis of DMD and met predefined entry criteria.25, 30 All eligible patients visiting the participating centers during the enrollment period were enrolled, supporting that the population analyzed represented an appropriate and unbiased control cohort of DMD patients.
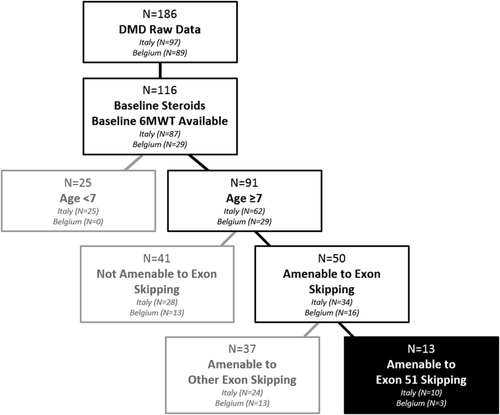
The historical control group included a total of 186 patients. For the purpose of the current analysis, only patients with corticosteroid therapy at baseline who had a baseline and at least 1 postbaseline assessment were included (n = 116), that is, 87 of 97 patients from the Italian DMD Registry and 29 of 89 patients from LNMRC (Fig 2).
Clinical Assessments
The 6MWT was performed by specifically trained physiotherapists according to accepted clinical standards.19 Assessments were done annually for the Italian DMD Registry, and at routine clinical visits in the LNMRC study.
Statistical Analysis
Analyses were based on 6MWT results at baseline and months 12, 24, and 36 (discrete months). Most but not all individuals had results reported through month 36. Distance walked was set to 0m when a patient became nonambulant. There were no other data imputations performed for 6MWT data.
All analyses were performed on patients in the eteplirsen intent-to-treat (n = 12) population. The data for both eteplirsen dose groups are pooled throughout this report. For all analyses, the data for the placebo to eteplirsen patients (n = 4) while on placebo for the first 24 weeks in studies 4658-201/202 were excluded to enable comparison of the on-treatment time period. As such, for these 4 patients the baseline data are equivalent to week 24, and months 12, 24, and 36 data are equivalent to weeks 74, 120, and 168, respectively. Day 1 6MWT results were used when the test was assessed on 2 consecutive days.
For historical control data, if a clinic's protocol did not specify a baseline and/or visit frequency, the first visit for eligible patients was termed the baseline visit, and if no assessment was available at the discrete time points, an assessment within 3.5 months of the corresponding discrete month was used.
Historical control data were evaluated for eligibility based on the criteria outlined in Figure 2. Key parameters examined to enable a robust statistical comparison to eteplirsen-treated patients were (1) corticosteroid use, (2) existence of sufficient longitudinal data to allow for identification of a baseline visit and follow-up values, (3) age <7 or ≥7 years, and (4) genotype and type of therapy to which patient is amenable. The assessment of eligibility and identification of subgroups were carried out programmatically by applying the same algorithm to all patients. The following subgroups are presented for comparative 6MWT analyses (Table 3): (1) amenable to any exon skipping and <7 years old (n = 17), (2) amenable to any exon skipping and ≥7 years old (n = 50), (3) not amenable to exon skipping and ≥7 years old (n = 41), (4) amenable to exon 51 skipping and ≥7 years old (n = 13), and (5) amenable to other exon skipping (nonexon 51) and ≥7 years old (n = 37). The subgroup that most closely matched the eteplirsen-treated patients was amenable to exon 51 skipping and ≥7 years old (n = 13).
| Group | No., Baseline | Age at Baseline, yr, Mean (SD) | 6MWT at Baseline, m, Mean (SD) | No., Month 36 | 6MWT at Month 36, m, Mean (SD) |
|---|---|---|---|---|---|
| Amenable to exon skipping, <7 years old | 17 | 5.97 (0.687) | 380.8 (64.75) | 17 | 396.2 (90.96) |
| Amenable to exon skipping, ≥7 years old | 50 | 9.68 (1.523) | 355.7 (87.28) | 47 | 175.7 (165.06) |
| Not amenable to exon skipping, ≥7 years old | 41 | 8.98 (2.019) | 383.2 (89.79) | 36 | 289.4 (194.08) |
| Amenable to other exon skipping [non-51], ≥7 years old | 37 | 9.76 (1.558) | 355.0 (94.24) | 36 | 199.3 (167.48) |
| Amenable to exon 51 skipping, ≥7 years old | 13 | 9.45 (1.454) | 357.6 (66.75) | 11 | 98.5 (136.28) |
| Eteplirsen-treated [ITT] | 12 | 9.41 (1.183) | 363.2 (42.19) | 12 | 263.1 (151.74) |
- Age and 6MWT distance at baseline and month 36 are shown for both eteplirsen-treated and historical control groups in reported comparative analyses.
- 6MWT = 6-Minute Walk Test; ITT = intent-to-treat; SD = standard deviation.
In the comparison of eteplirsen-treated patients to historical controls, observed 6MWT data at baseline and months 12, 24, and 36 were used, and mean ± standard error of the mean was plotted over time for both groups (eg, eteplirsen-treated and historical controls), and was compared using the analysis of covariance (ANCOVA) model with group (eg, genotype, age, eteplirsen vs untreated, etc) as a fixed-effect term and baseline 6MWT as a covariate. No adjustments were made for multiple comparisons. In addition, change from baseline in 6MWT was summarized for months 12, 24, and 36, and as a sensitivity analysis, compared between the 2 groups using the Wilcoxon rank sum test. Finally, sensitivity analysis by last observation carried forward (LOCF) was performed.
Results
Selection of Matched Historical Control Cohort
Corticosteroid Treatment
Based on the documented effect of corticosteroids on disease progression,3 only patients treated with corticosteroids were included in the current analyses.
Disease Progression by Mutation Type and Age (<7 vs ≥7 Years Old)
It has been previously suggested that disease severity may be affected by mutation type,25 and multiple publications have demonstrated an age-dependent change in disease trajectory, showing that when younger than 7 years, boys with DMD experience a steady increase in 6MWT distance, whereas boys aged ≥7 years experience progressive decline.15, 26 In the current study, the pooled historical control data set was analyzed to further elucidate the effect of mutation type and age on disease progression to further the field's understanding of DMD disease progression and to identify the most comparable patient subset for comparison to the eteplirsen-treated cohort.
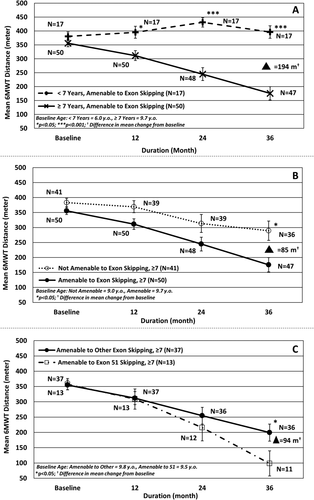
Age
The previously reported age dichotomy15, 26 observed for the general DMD population was confirmed for the subpopulation of patients with genotypes amenable to exon skipping (see Fig 3A). Consistent with previous reports, patients <7 years of age showed improvement over the first 2 years of observation, followed by a decline (although remaining above the baseline value by 25m) between months 24 and 36. In contrast, the older age group showed a disease progression trajectory characterized by declines of 93m by 24 months, and 142m by 36 months. The difference between the 2 age groups was statistically significant over the entire observation period (p < 0.05 at 12 months, p < 0.001 at 24 and 36 months). Two patients in the older group did not contribute data at the 36-month time point. Sensitivity analysis by LOCF, an approach that imputes the last observed value for these patients at the 36-month time point, showed a difference of 187m (p < 0.001) in favor of the younger age group.
The decline of the younger group in the 3rd year of observation demonstrates internal consistency of the data as the patients in this younger population become older (reaching a mean age of 8 years by month 24) and begin to enter the decline phase (see Fig 3A).
Given the confirmation of age dichotomy and the older mean baseline age of eteplirsen-treated patients of 9.3 years (range = 7–11; see Table 1), only historical control patients ≥7 years old, who will therefore be in the same decline phase of disease as the eteplirsen-treated patients, are appropriate for consideration as a comparator group.
Genotype
Whether all patients ≥7 years old or only a genotypically similar subset of these patients should be used for comparison to the eteplirsen cohort was further analyzed. Comparison of patients ≥7 years old by genotype demonstrates that patients amenable to exon skipping experience more severe disease progression than those who are not (see Fig 3B), with those amenable to exon skipping showing an 85m greater decrease in 6MWT distance at 36 months that is statistically significant (p < 0.05). Patients from both groups did not contribute data to all time points, and sensitivity analysis by LOCF showed a difference of 84m (p < 0.05) in favor of the group not amenable to exon skipping at 36 months.
Further comparison of patients ≥7 years old by genotype demonstrates that patients amenable to exon 51 skipping experience even more rapid disease progression than patients amenable to skipping other exons. This difference is statistically significant by 36 months (see Fig 3C), with patients amenable to exon 51 skipping showing a 94m greater decrease in 6MWT distance (p < 0.05). Two patients from the exon 51 amenable group and 1 patient from the group amenable to skipping other exons did not contribute data at all time points. Sensitivity analysis by LOCF showed a smaller but clinically meaningful difference of 67m (p = 0.12) in favor of the group amenable to skipping other exons.
These analyses indicate that the historical control subset of patients ≥7 years old amenable to exon 51 skipping constitutes the most appropriate matched historical control subset for comparison to the eteplirsen-treated cohort. This comparative subset consists of 13 patients. As noted above, 2 historical control patients in this subset did not have data available at all time-points; 1 historical control patient contributed data at baseline and 12 months, a second contributed data at baseline and 12 and 24 months. The remaining 11 historical control patients contributed data at all time points (baseline, 12, 24, and 36 months), and therefore these 11 patients were used for the final comparison at 36 months.
Comparison of 6MWT in Eteplirsen-Treated Patients to Matched Historical Controls
Baseline Characteristics of the Eteplirsen-Treated and Matched Control Cohorts
The 12 eteplirsen-treated patients represented 5 different genotypes amenable to exon 51 skipping: deletions of exons 45 to 50 (n = 3), 48 to 50 (n = 1), 49 and 50 (n = 5), 50 (n = 1), and 52 (n = 2). Their baseline mean age was 9.4 years and mean 6MWT distance at baseline was 363.2m (Table 4). Mean pulmonary function tests (MIP, MEP, and FVC percentage of predicted) at baseline were within normal ranges34 (see Table 2).
| Characteristic | Pivotal Study | 6MWT Historical Control Group |
|---|---|---|
| Parameter | Eteplirsen-treated, study 201/202, n = 12 | Untreated, external, exon 51 skipping, n = 13 |
| Male gender | 100% | 100% |
| Age, yr | ||
| Mean (SD) | 9.41 (1.183) | 9.45 (1.454) |
| Median | 9.7 | 9.0 |
| Minimum, maximum | 7.3, 11 | 7.3, 11.8 |
| Steroids, % yes | 100 | 100 |
| Standard of care, % yes | 100 | 100 |
| Ambulatory status, % yes | 100 | 100 |
| 6MWT distance, m | ||
| Mean (SD) | 363.2 (42.19) | 357.6 (66.75) |
| Minimum, maximum | 256, 416 | 200, 458 |
| Genotype, exon skippable | Exon 51 | Exon 51 |
| Represented exon 5-skipping amenable deletion mutations, No. | ||
| Exons 45–50 | 3 | 3 |
| Exons 48, 50 | 1 | 2 |
| Exons 49, 50 | 5 | 3 |
| Exon 50 | 1 | 2 |
| Exon 52 | 2 | 3 |
- Baseline comparability of the eteplirsen-treated and historical control population ≥7 years old and amenable to exon 51 skipping is explored here. Populations consist of ambulatory, steroid-treated patients with similar genotypes who had received similar standards of care.
- 6MWT = 6-Minute Walk Test; SD = standard deviation.
The matched historical control cohort of patients ≥7 years of age amenable to exon 51 skipping (n = 13) represented deletions of exons 45 to 50 (n = 3), 48 to 50 (n = 2), 49 and 50 (n = 3), 50 (n = 2), and 52 (n = 3). Their baseline mean age was 9.5 years and mean 6MWT distance was 357.6m (see Table 4).
Comparison of Ambulatory Function
Evaluation of 6MWT results of eteplirsen-treated patients and historical control patients ≥7 years of age amenable to exon 51 skipping showed comparable baseline 6MWT distances that diverged through the second and third year, culminating in a 75m difference in 6MWT decline between the groups by 24 months, and a statistically significant (p < 0.01 from both ANCOVA and Wilcoxon rank sum test) and clinically meaningful29 difference in 6MWT decline of 151m between the groups by 36 months (Fig 4A).
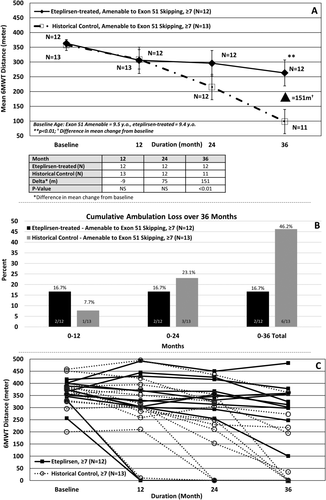
Sensitivity analysis by LOCF, imputing the 12- and 24-month values at 36 months for the 2 historical control patients who did not have 36-month values available, showed a difference of 121m (p = 0.028) in favor of the eteplirsen group.
The proportion of patients who lost ambulation was also evaluated. Over a 3-year period, eteplirsen treatment markedly reduced loss of ambulation compared to matched historical controls. After 3 years, 2 of 12 (16.7%) eteplirsen-treated patients lost ambulation, compared with 6 of 13 (46.2%) historical control patients ≥7 years of age amenable to exon 51 skipping (see Fig 4B).
Given the perceived variability in DMD patients on 6MWT over time, it is important to evaluate the extent to which individual patients may impact the overall results. As such, individual patient data provide an important perspective when comparing eteplirsen patients versus matched historical controls. Individual patient data further detail the differences between eteplirsen-treated patients and the group of steroid-treated natural history controls ≥7 years old and amenable to exon 51 skipping (see Fig 4C).
Pulmonary Function Tests
Over 36 months of treatment, mean percentage of predicted MIP (%pMIP) declined by 2.2% (from 91.7% at baseline to 89.5%), mean percentage of predicted MEP (%pMEP) declined by 5.0% (79.3% to 74.3%), and mean percentage of predicted FVC (%pFVC) declined by 9.4% (101.3% to 91.9%; Fig 5). Pulmonary function data were not available for the matched historical control patients, and therefore comparison can only be made to published natural history. Pulmonary function data from recent natural history studies in patients with DMD suggest that %pMEP and %pMIP decline at a rate of 4% per year for patients in the age range of 6 to 19 years, and %pFVC declines at a rate of 5% per year for patients in the age range of 5 to 24 years.3, 31 Thus, over a period of 36 months, patients not receiving eteplirsen might be expected to show declines in MEP and MIP of approximately 11.5% and declines in FVC of approximately 14.3%.
Safety
Over approximately 3 years, weekly eteplirsen infusions were well tolerated, with no reports of systemic reactions and no serious adverse events related to treatment. The most frequently reported adverse events on eteplirsen over 3 years of evaluation were headaches (n = 8), procedural pain related to biopsy and catheter placement (n = 7), and proteinuria (n = 6; Table 5). A total of 8 adverse events (7 while receiving eteplirsen, 1 on placebo) occurring in 7 subjects were considered to be possibly or probably related to study drug by the investigator. Treatment continued uninterrupted through these events, which involved 2 patients whose tunneled port catheters were observed to be thrombosed prior to study drug infusion; 1 placebo patient with mild nausea; 1 patient with 2 events of mild erythema (reddened cheeks); 1 patient with a previous history of low white blood cell counts whose count fell to 3.70 × 109/l (lower limit of normal range = 4.00 × 109/l); and 2 patients with mild, transient proteinuria.
| Treatment-Emergent
Adverse Event |
Placebo for 24 Weeks,a n = 4 (%) |
Eteplirsen for 24 Weeks,a n = 8 (%) |
Eteplirsen for 144 Weeks,b n = 4 (%) |
Eteplirsen for 168 Weeks,c n = 8 (%) |
|---|---|---|---|---|
| Procedural pain | 3 (75) | 4 (50) | 1 (25) | 6 (75) |
| Vomiting | 0 | 3 (38) | 2 (50) | 4 (50) |
| Hypokalemia | 2 (50) | 4 (50) | 0 | 4 (50) |
| Cough | 2 (50) | 2 (25) | 1 (25) | 3 (38) |
| Back pain | 2 (50) | 1 (12) | 1 (25) | 4 (50) |
| Fall | 1 (25) | 1 (12) | 0 | 1 (12) |
| Headache | 2 (50) | 1 (12) | 4 (100) | 4 (50) |
| Balance disorder | 0 | 3 (38) | 0 | 4 (50) |
| Diarrhea | 1 (25) | 1 (12) | 1 (25) | 2 (25) |
| Contact dermatitis | 0 | 2 (25) | 0 | 3 (38) |
| Pyrexia | 2 (50) | 1 (12) | 0 | 1 (12) |
| Hematoma | 1 (25) | 2 (25) | 0 | 2 (25) |
| Abdominal pain | 2 (50) | 0 | 1 (25) | 1 (12) |
| Nausea | 1 (25) | 1 (12) | 2 (50) | 1 (12) |
| Rhinitis | 1 (25) | 1 (12) | 0 | 1 (12) |
| Polyuria | 0 | 1 (12) | 0 | 1 (12) |
| Muscle spasms | 0 | 1 (12) | 2 (50) | 1 (12) |
| Musculoskeletal pain | 0 | 1 (12) | 1 (25) | 1 (12) |
| Proteinuria | 1 (25) | 0 | 1 (25) | 5 (62) |
| Injection site pain | 0 | 1 (12) | 0 | 1 (12) |
- Events commonly observed in study 201/202 are reported. Events reported through 24 weeks represent those observed in the placebo-controlled phase, whereas those reported through 144 or 168 weeks represent those observed while patients were on eteplirsen treatment.
- a Double-blind treatment period for the continuous eteplirsen cohort and placebo/delayed cohort.
- b Open-label treatment period for the placebo/delayed cohort.
- c Double-blind and open-label treatment periods for the continuous eteplirsen cohort.
Protein was detected in 19 of 609 urine samples tested over the approximate 3-year period in all patients who received eteplirsen. All levels were low (1+ on dipstick assay) except 2 instances of 2+ that were accompanied by bacteriuria; all increases were transient and resolved spontaneously with no indication of renal toxicity assessed by elevated KIM-1 or cystatin C, or clinical signs or symptoms. An episode of proteinuria, which was determined to be unrelated to the study treatment, also occurred in 1 patient on placebo. Like the other episodes of proteinuria, this episode was mild, and required no pharmacologic intervention or interruption of study treatment. Hematology and coagulation parameters were generally within normal range. Blood chemistry reflected the expected disease-related abnormalities, with markedly elevated creatine kinase, aspartate aminotransferase, and alanine aminotransferase, all of which decreased over the course of treatment with eteplirsen. There were no signs or symptoms of hepatic toxicity.
None of the adverse events led to treatment interruption or dose adjustments. All patients continued to be treated with the assigned dose of eteplirsen, and there were no deaths or treatment discontinuations.
Discussion
Eteplirsen has been previously demonstrated to reliably induce the production of functional dystrophin in patients with DMD,1, 10-12 and in so doing, significantly slowed the rate of progression of this devastating disease as demonstrated here by comparison of longitudinal 6MWT results to untreated, matched historical controls over 36 months. This was evidenced by a slower decline in walking ability in eteplirsen-treated patients compared to age-matched historical controls amenable to exon 51 skipping, with a clinically relevant 75m difference by 24 months, and a statistically significant and clinically relevant difference of 151m by 36 months.
Because 2 historical control patients did not have data available at the 36-month time point (1 patient contributed data at baseline and 12 months, whereas the second contributed data at baseline and 12 and 24 months), sensitivity analysis was conducted by LOCF. In this approach, the last observed value for the first patient at 12 months (375m) and for the second patient at 24 months (320m) was imputed as a 36-month result. This is an extremely conservative approach, as neither patient would be expected to remain stable over such a long period of time given their respective ages at baseline (8.6 years and 11.5 years, respectively) and last reported 6MWT distances. Even using this very conservative approach, the analysis favored the eteplirsen group by 121m, a difference that is clinically meaningful and statistically significant.
Not only did eteplirsen-treated patients experience a slower decline in 6MWT distance, fewer eteplirsen-treated patients lost ambulation than untreated, matched historical controls. During the 3-year treatment period, 2 of 12 eteplirsen-treated patients lost ambulation by year 1 and none thereafter (16.6%). In contrast, 6 of 13 (46%) historical control patients lost ambulation by 36 months.
To validate the approach for selecting the natural history control cohort, it was essential to ensure comparability of the cohort to eteplirsen-treated patients at baseline as well as comparability of their expected rates of disease progression. The overall historical control cohort used was considered a valid comparator group based on the following: (1) all patients who met the predefined entry criteria and visited the participating centers during the enrollment period were included in the historical control studies, supporting that the population enrolled represents an unbiased control cohort of DMD patients; (2) patients with cognitive impairment that could impact 6MWT outcome were excluded from all studies; (3) the participating clinics specialize in neuromuscular care and follow the internationally recognized treatment guidelines for patients with DMD27, 28 that is used for the eteplirsen-treated patients, including recommendation for corticosteroid use, dose, and dose adjustment; (4) assessments of the 6MWT were performed by specifically trained physiotherapists according to the same established standards used for the eteplirsen-treated patients.13 To further increase comparability between the groups not only at baseline but also by rate of disease progression, control patients were matched to the eteplirsen population based on (5) corticosteroid use, (6) age, and (7) genotype.
Selection based on these parameters is supported by recent reports indicating that the main variables impacting disease progression in ambulatory DMD patients as measured by 6MWT are age, genotype, 6MWT distance at baseline, and corticosteroid use.3, 16, 24, 25, 29 Given the data that support the effect of corticosteroid therapy on delaying disease progression in DMD,3 corticosteroid use at baseline was required for all patients in the eteplirsen-treated as well as the control cohort.
Results of these analyses have important implications for the field's understanding of disease natural history as well as for clinical trial design. Confirmation of the previously reported age dichotomy for the subset of steroid-treated patients amenable to exon skipping, showing a rapid and consistent decline in ambulation, endurance, and muscle function as measured by the 6MWT in boys with DMD who are ≥7 years of age, whereas those <7 years old are stable or increase in their 6MWT distance, supports the exclusion of patients <7 years old from studies that aim to prognostically enrich for a declining population.
Earlier analysis of the Italian DMD registry had suggested the potential for mutation type to affect disease progression.25 In the current analysis, patients amenable to exon skipping were shown to experience more rapid declines on 6MWT than those with mutations not amenable to exon skipping, a difference that was statistically significant at 36 months. Furthermore, patients amenable to exon 51 skipping experienced an even more rapid disease progression than patients amenable to skipping other exons. These data are consistent with the literature and suggest that matching placebo and treated patients by amenability to any exon skipping may be important in evaluating drug effect.
Of note, the mean 6MWT distance of the eteplirsen-treated patients at 12 months was essentially equivalent to the historical control cohort. This is most likely due to the early loss of ambulation experienced by 2 eteplirsen-treated subjects in a small study population. Whether this suggests that longer evaluation periods are needed to observe a treatment effect will be explored further in the larger, PROMOVI confirmatory study that is currently underway.
Taken together, these analyses confirm that steroid-treated patients ≥7 years old who are amenable to exon 51 skipping are the most appropriate natural history control for the eteplirsen study 4568-201/202 cohort. Furthermore, these analyses confirm the validity of the 4568-201/202 eteplirsen study design, indicating that enrolling patients ≥7 years old enables the sensitive evaluation of functional treatment effect without the confounding impact of data from patients <7 years old who, although lagging behind their healthy age-matched peers, show gains in motor function due to growth and development. Limitations of the eteplirsen clinical study presented here include the small number of patients as well as the unblinded treatment of patients in the extension phase, although disease natural history suggests that placebo effect would be unlikely to preserve ambulation over 3 years in the advanced population studied. The close concordance of the mean baseline 6MWT of the eteplirsen-treated patients and the historical controls was somewhat unexpected but may suggest that the heterogeneity observed for the general DMD population decreases significantly when patients are comparable on factors known to influence disease progression, namely age, steroid use, baseline 6MWT, and genotype.
The 6MWT has been widely used as an outcome measure in DMD, as it is an integrated assessment of global muscle function and endurance. In addition, loss of ambulation is a crucial disease milestone that carries significant emotional as well as physical and practical implications for patients and families, marking a transition to progressively decreasing independence and increasing need for assistance with activities of daily living.36-39
Although preservation of ambulation is strongly desired, respiratory failure is a leading cause of death for patients with DMD.36, 38 The importance of respiratory abnormalities is well understood in later stages of DMD, but early subclinical deterioration of respiratory muscles with a mean annual decline in %pMIP and %pMEP of approximately 4% and %pFVC of approximately 5% has only recently been recognized.3, 31 %pMIP and %pMEP assess progression of DMD regardless of ambulatory status and are the most sensitive indicators of decreasing respiratory muscle strength, with %pMEP being the first pulmonary parameter to decline in patients with DMD.39, 40 Thus, the observed relative stability of respiratory muscle function over >3 years observed in this study is important supporting evidence for the clinical efficacy of eteplirsen above and beyond endurance, ambulation, and muscle function that is measured by the 6MWT.19
Eteplirsen was well tolerated over 3.2 years. Notably, adverse events frequently seen with other RNA analogs, including administration site reactions, flulike symptoms, coagulopathies, inflammatory response, and renal or hepatic toxicity,20, 33 were observed rarely, if at all.20, 33 This is consistent with the safety profile and tolerability of eteplirsen and other PMO-based oligomers seen in animals41-43 and in other human studies.44 This lack of toxicity is attributed to PMO chemistry, which is charge-neutral, largely unmetabolized, and not linked to immune activation,10, 45 platelet activation, or hepatotoxicity.
Outcome assessment in comparison to an appropriately matched natural history or historical control population has been used to support regulatory approval of several therapies targeted to ultra-orphan populations over the past decade including Myozyme for Pompe disease46 and CEPROTIN for patients with severe congenital protein C deficiency.47 These present results indicate such an approach may also be appropriate for DMD, especially as it would spare declining patients from receiving placebo rather than potentially disease-altering treatment.
In summary, this analysis shows that eteplirsen-treated patients with DMD experienced a slower decline in disease progression over 3 years as measured by the 6MWT than historical control patients who were appropriately matched for age, steroid use, and mutation type. The observed differences were clinically meaningful, statistically significant, and supported by differences in the rate of loss of ambulation and by the relative stability seen on pulmonary function testing over the same time period.
Acknowledgment
Studies 201/202 were funded by Sarepta Therapeutics and registered on ClinicalTrials.gov under identification numbers NCT01396239 and NCT01540409. E.M. received a grant from the Italian Telethon to support this study.
We thank the patients and their families for their participation in the studies or registries; the members of the Eteplirsen Study Group and their supporting staff who were instrumental in the conduct of this study and collection of the data: H. Abdel-Hamid, B. J. Byrne, A. M. Connolly, R. A. Dracker, L. M. Frank, P. T. Heydemann, K. C. O'Brien, S. E. Sparks, and L. A. Specht; the staff of the Paul D. Wellstone Muscular Dystrophy Clinical Research Center who have made contributions to this effort: L. Rodino-Klapac, Z. Sahenk, S. Al-Zaidy, L. H. Cripe, and S. Lewis; to the staff and nurses of Clinical Research Service at Nationwide Children's Hospital; to M. vanden Hauwe and A. Van Impe, clinical evaluators, for their contribution to the natural history study at the LNMRC; the members of the DMD Italian network for their contributions to the natural history study detailed in this report: M. Pane, E. Mazzone, S. Messina, G. L. Vita, A. D'Amico, E. S. Bertini, A. Berardinelli, Y. Torrente, F. Magri, G. P. Comi, G. Baranello, T. Mongini, A. Pini, R. Battini, E. Pegoraro, C. Bruno, L. Politano, and S. Previtali; J. B. Saoud for his vital contributions to design and execution of reported analyses; and P. Duda, J. Friedman, R. Kole, E. Naughton, and K. Lucas for their valuable comments and editorial help in the preparation of this paper.
Author Contributions
Concept and study design: J.R.M., N.G., E.M.K., E.M. Data acquisition and analysis: J.R.M., N.G., L.P.L., L.N.A., K.B., J.S. Drafting the manuscript and figures: J.R.M., N.G., J.S., E.M.K., E.M.
Potential Conflicts of Interest
J.S. and E.M.K. are employed at Sarepta Therapeutics. The study data were generated at Nationwide Children's Hospital, and they were not involved in that process. J.R.M. worked in cooperation with Nationwide Children's Hospital as related to these studies. N.G. is principal investigator of several antisense oligonucleotide exon skip studies in DMD (compensation limited to trial costs), none of which is sponsored by Sarepta. The LNMRC Natural History study has been supported by the Klinisch Onderzoeksfonds UZ Leuven and the Fonds voor Spierzieke Kinderen. E.M. has served on advisory boards for Sarepta Therapeutics.