Prediction of testicular atrophy based on sonographic findings immediately after successful manual detorsion
Abstract
Purpose
To investigate and determine the sonographic findings obtained from manually distorted testes to predict testicular atrophy following manual detorsion.
Materials and methods
Twenty-two patients who had been diagnosed with testicular torsion and undergone manual detorsion were included. These patients were classified according to the presence or absence of testicular atrophy. The duration of symptoms, presence or absence of hyperperfusion within the entire affected testis, and echogenicity (homogeneous or heterogeneous) within the affected testis were compared using the Mann–Whitney U-test or Fisher's exact test, as appropriate.
Results
Testicular atrophy was detected in seven patients. There was a significant difference in the frequency of hyperperfusion within the entire affected testis (with atrophy [present/absent] vs. without atrophy [present/absent] = 0/7 vs. 8/7, P = 0.023) between patients with and without testicular atrophy. No significant differences in the duration of symptoms (with atrophy vs. without atrophy = 7 ± 3.3 h vs. 4.7 ± 3.6 h, P = 0.075) or frequency of echogenicity within the testis (with atrophy [heterogeneous/homogeneous] vs. without atrophy [heterogeneous/homogeneous] = 2/5 vs. 2/13, P = 0.565) were observed between the groups.
Conclusions
This small cohort study suggests that the presence of hyperperfusion within the entire affected testis immediately after successful manual detorsion is useful in predicting the avoidance of testicular atrophy.
Introduction
Testicular torsion is one of the most common causes of testicular loss in paediatric patients owing to the resulting interruption of blood flow to the testes.1-3 Rapid diagnosis and treatment via manual or surgical detorsion are required to restore testicular blood flow and prevent necrosis.2, 4, 5 Compared with surgical exploration, manual detorsion is advantageous since this bedside procedure can be performed immediately after torsion. However, in the manual procedure, only detorsion is performed, while orchiopexy to prevent recurrence of testicular torsion and fasciotomy to prevent testicular compartment syndrome due to reperfusion cannot be performed.2, 4, 6-12
Surgical exploration is usually performed following manual detorsion, regardless of whether detorsion is successful; however, the time between manual detorsion and surgical exploration varies among patients and hospitals.6, 8, 13 Therefore, successful manual detorsion is important for decreasing testicular ischemic time. Clinically, the success of manual detorsion is usually determined based on the patients' symptoms and sonographic findings, which are finally recognised during surgical exploration.4, 13, 14 Previous studies have reported that some patients exhibit residual testicular torsion, continued testicular pain, or testicular atrophy even after successful manual detorsion.4, 13, 14
Ultrasound is useful for diagnosing testicular torsion and predicting subsequent testicular atrophy or necrosis; however, previous reports have focused on sonographic findings obtained from twisted testes before successful manual detorsion.1-3, 14-18 In this study, we aimed to investigate and determine the sonographic findings obtained from manually distorted testes to predict testicular atrophy after manual detorsion.
Patients and methods
Patients
This retrospective study was approved by the ethics committee of our institution and was conducted in accordance with the tenets of the Declaration of Helsinki. The requirement for informed consent was waived owing to the retrospective nature of the study.
A review of medical records from September 2017 to December 2021 identified 27 paediatric patients with testicular torsion who had been diagnosed via ultrasound and underwent manual detorsion. The following patients were excluded: (a) patients in whom manual detorsion was unsuccessful and who required urgent surgical exploration (n = 4) and (b) patients who did not undergo surgical exploration after successful manual detorsion (n = 1).
Ultrasound for diagnosis of testicular torsion
Ultrasound was performed immediately after successful manual detorsion by one of four paediatric radiologists (with 25, 20, 15, and 12 years of clinical experience in paediatric ultrasound, respectively) using a 9–15-MHz linear transducer (LOGIQ 7, E9, S8, and E10; GE Healthcare, Waukesha, WI). During the study period, all the patients with suspected testicular torsion underwent sonographic examination by paediatric radiologists. Testicular torsion was diagnosed based on a combination of the following several sonographic findings and clinical symptoms: presence of spermatic cord twisting as whirlpool signs, absence of blood flow within the testis, abnormal testicular axis, enlargement of the affected testis and epidermis without blood flow.1, 3, 15
Patient characteristics
The following patient characteristics were recorded: the side (right or left) of testicular torsion, patient age at the diagnosis of testicular torsion, direction (inner or outer) of testicular torsion, duration of symptoms (the time from the onset of scrotal pain to ultrasound examination), the interval from manual detorsion to subsequent surgical exploration, and the interval from manual detorsion to the last evaluation of testicular size. The inner/outer direction of testicular torsion was defined as lateral to medial/medial to lateral twisting based on manual detorsion.
Manual detorsion
After establishing the diagnosis of testicular torsion via ultrasound, manual detorsion was performed by one of seven paediatric surgeons/urologists (with 22, 12, 12, 7, 7, 5, and 4 years of clinical experience in paediatric surgery or urology). The affected testis was rotated in the outer (medial to lateral) or inner (lateral to medial) direction based on the sonographic findings and patient symptoms during manual detorsion.4, 15, 18, 19 The degree of spermatic cord twisting was recorded during the procedure. No anaesthesia was administered to preserve pain sensation.
Successful manual detorsion was defined as the restoration of blood flow within the testis as confirmed using ultrasound, the disappearance of whirlpool signs on ultrasound, and the absence of residual spermatic cord twisting during surgical exploration after manual detorsion.6, 8, 14, 15
Surgical exploration
Surgical exploration was performed by paediatric surgeons or urologists. Orchiopexy was performed in all the patients to prevent testicular torsion recurrence. Fasciotomy and/or orchiectomy was performed by surgeons when deemed necessary.
Ultrasound after manual detorsion
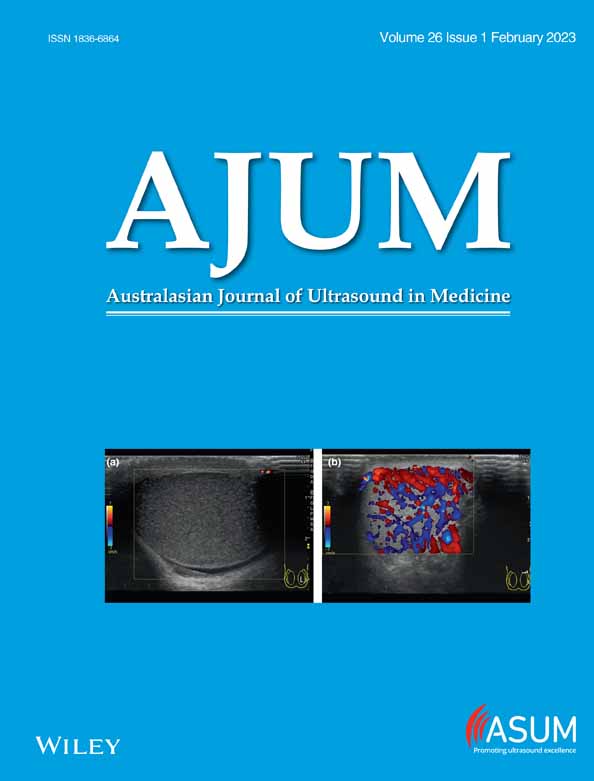
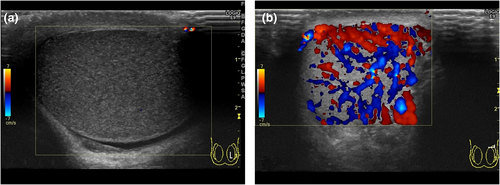
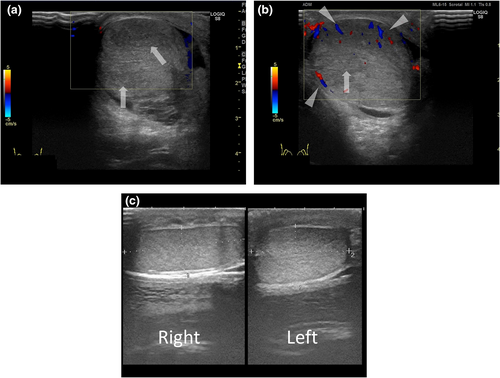
The following sonographic findings were evaluated: hyperperfusion within the entire affected testis and echogenicity within the affected testis compared with the normal side.8, 14 “Hyperperfusion within the entire affected testis” was classified into presence or absence of increased colour flow (>100% compared to the unaffected testis) in the whole area of the affected testis (Figures 1b). Increased colour flow (>100%) in the segmental area, such as the peripheral area of the testis, was not included in the “entire” testis (Figures 2b and 3b). “Echogenicity within the affected testis” was classified into homogeneous (Figures 1a and 3a) or heterogeneous (Figure 2a).17, 20-22
Testicular atrophy
Testicular atrophy was defined as a decrease in testicular size (<80%) when compared with that of the unaffected testis (Figure 3c).23 Testicular size was evaluated via ultrasound 2–3 months after successful manual detorsion. Testicular volume on ultrasound was estimated according to the following ellipsoid formula: length × width × thickness × 0.71 cm3.23, 24
Review process
The sonograms of all the patients were evaluated by two radiologists (with 15 and 12 years of clinical experience in paediatric ultrasonography, respectively) using a 1600 × 1200 picture archiving and communication system monitor (GE Healthcare), and the presence or absence of sonographic findings was determined by consensus. During the review process, the radiologists were blinded to the patients' medical records, including physical examination and imaging data.
Statistical analyses
Data are presented as the mean ± standard deviation. The side and direction of testicular torsion were compared using Fisher's exact test. Patient age, duration of symptoms, degree of spermatic cord twisting, and interval from manual detorsion to subsequent surgical exploration were compared using the Mann–Whitney U-test. The surgical procedure after manual detorsion and the presence or absence of the following sonographic findings were compared using Fisher's exact test: hyperperfusion within the entire affected testis and homoechogenicity within the testis.
All tests were two-sided, and the significance level was set at 5%. Data were analysed using Statistical Package for the Social Sciences version 24 (IBM, Armonk, NY, USA).
Ethical approval
This retrospective study was approved by the ethics committee of our institution and conducted in accordance with the tenets of the Declaration of Helsinki.
Results
Patient characteristics
The characteristics of the 22 patients with testicular torsion are summarised in Table 1. The degree of spermatic cord twisting was not recorded in five patients.
| Case | Side | Age (years) | Direction of testicular torsion | Symptom duration (h) | Echogenicity within the affected testis | Hyperperfusion (>100% compared to the unaffected testis) within the entire affected testis | Degree of spermatic cord twisting* | Interval from manual detorsion to subsequent surgical exploration (days) | Fasciotomy during surgical exploration | Testicular atrophy | Testicular size when compared with the unaffected side (%) | Interval from manual detorsion to the last evaluation of testicular size (days) | Note: |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Left | 14 | Inner | 10 | Homogenicity | Absent | na | 78 | Not performed | Present | 50 | 96 | |
| 2 | Left | 14 | Inner | 8 | Homogenicity | Absent | 360 | 1 | Not performed | Present | 53 | 49 | |
| 3 | Left | 12 | Outer | 7 | Homogenicity | Absent | 360 | 1 | Not performed | Present | 56 | 183 | Figure 3 |
| 4 | Left | 16 | Outer | 5 | Homogenicity | Absent | 360 | 5 | Not performed | Present | 78 | 51 | |
| 5 | Left | 14 | Inner | 3 | Homogenicity | Absent | 360 | 26 | Not performed | Present | 48 | 127 | |
| 6 | Left | 11 | Inner | 4 | Heterogenicity | Absent | 360 | 51 | Not performed | Present | 75 | 348 | |
| 7 | Left | 13 | Outer | 12 | Heterogenicity | Absent | 540 | 1 | Not performed | Present | 75 | 82 | |
| 8 | Right | 13 | Outer | 14 | Homogenicity | Present | na | 21 | Not performed | Absent | 100 | 135 | |
| 9 | Left | 13 | Inner | 5 | Homogenicity | Present | na | 4 | Not performed | Absent | 87 | 83 | |
| 10 | Left | 14 | Inner | 5 | Homogenicity | Present | 720 | 17 | Not performed | Absent | 86 | 465 | Figure 1 |
| 11 | Left | 14 | Inner | 3 | Homogenicity | Present | 540 | 3 | Not performed | Absent | 100 | 215 | |
| 12 | Right | 14 | Inner | 3 | Homogenicity | Present | na | 11 | Not performed | Absent | 100 | 61 | |
| 13 | Left | 12 | Inner | 3 | Homogenicity | Present | 360 | 15 | Not performed | Absent | 100 | 403 | |
| 14 | Left | 14 | Inner | 2 | Homogenicity | Present | 540 | 70 | Not performed | Absent | 98 | 84 | |
| 15 | Left | 14 | Inner | 2 | Homogenicity | Present | 720 | 43 | Not performed | Absent | 101 | 50 | |
| 16 | Right | 13 | Inner | 4 | Homogenicity | Absent | 540 | 31 | Not performed | Absent | 100 | 409 | |
| 17 | Left | 13 | Inner | 4 | Homogenicity | Absent | 360 | 46 | Not performed | Absent | 100 | 205 | |
| 18 | Right | 14 | Outer | 4 | Homogenicity | Absent | 360 | 17 | Not performed | Absent | 101 | 100 | |
| 19 | Left | 14 | Inner | 2 | Homogenicity | Absent | 360 | 4 | Not performed | Absent | 100 | 150 | |
| 20 | Left | 14 | Outer | 2 | Homogenicity | Absent | na | 12 | Not performed | Absent | 87 | 187 | |
| 21 | Left | 12 | Inner | 12 | Heterogenicity | Absent | 360 | 1 | Performed | Absent | 97 | 423 | Figure 2 |
| 22 | Right | 15 | Inner | 6 | Heterogenicity | Absent | 540 | 0 | Performed | Absent | 100 | 122 |
- * Spermatic cord twisting was not available (na) in five patients.
Of the 22 patients, 17 and 5 had torsion on the left and right sides, respectively. The direction of testicular torsion was inner and outer in 16 and six patients, respectively. The mean age of the patients was 13.5 ± 1.1 (range, 11–16) years; the mean duration of symptoms was 5.5 ± 3.6 (range, 2–14) hours; the mean degree of spermatic cord twisting was 455.3 ± 129.1 (range, 360–720) degrees the mean interval from manual detorsion to subsequent surgical exploration was 20.8 ± 23.1 (range, 0–78) days; and the mean interval from manual detorsion to the last evaluation of testicular size was 183.1 ± 135.9 (range, 49–465) days.
Sonographic findings
In the analysis of blood flow within the affected testis, the presence of hyperperfusion within the entire affected testis was detected in eight patients. Four patients had heterogeneous echogenicity in the affected testis.
Surgical exploration
Two of the 22 patients underwent fasciotomy. None of our patients underwent orchiectomy.
Surgical findings
Paediatric surgeons or urologists assessed the testicular colour and size during surgical exploration. The testicular colour was abnormal in three cases. One case showed testicular atrophy during surgical exploration. In case 7 (with testicular atrophy), the affected testis was bluish, and blood flow was restored 15 min after the tissue was soaked in warm saline-soaked gauze. The affected testis was oedematous and dark in cases 21 and 22 (without testicular atrophy). Blood flow was partially restored after soaking in warm saline-soaked gauze, and fasciotomy was performed.
Testicular atrophy
The average size of the affected testis relative to the unaffected side was 86.1 ± 18.8% (range, 50–101%). Testicular atrophy was detected in seven patients. In this group, the average size of the affected testis relative to the unaffected side was 62.1 ± 13.2% (range, 50–78%).
Comparison between patients with and without testicular atrophy
Testicular atrophy did not occur in all patients exhibiting hyperperfusion within the entire affected testis and in some patients without this finding.
The results of the comparison of patient characteristics and sonographic findings between patients with and without testicular atrophy are summarised in Table 2.
| With testicular atrophy | Without testicular atrophy | p value | |
|---|---|---|---|
| Patient characteristics | |||
| Side (left/right) | 7/0 | 10/5 | 0.135 |
| Age | 13.4 ± 1.6 years [range, 11–16 years] |
13.5 ± 0.8 years [range, 13–15 years] |
0.849 |
| Direction of testicular torsion (inner/outer) (n/N) | 4/3 | 12/3 | 0.334 |
| Duration of symptoms (h) | 7 ± 3.3 [range, 3–12] |
4.7 ± 3.6 [range, 2–14 ] |
0.075 |
| Degree of spermatic cord twisting (degrees)* | 390 ± 73.5 [range, 360–540] |
490.9 ± 141.5 [range, 360–702] |
0.123 |
| Interval from manual detorsion to subsequent surgical exploration (days) | 23.3 ± 30.5 [range, 1–78] |
19.7 ± 20.0 [range, 0–70] |
0.832 |
| Fasciotomy during surgical exploration (performed/not performed) | 0/7 | 2/13 | 1 |
| Interval from manual detorsion to the last evaluation of testicular size (days) | 133.7 ± 105.3 [range, 49–348] |
206.1 ± 145.5 [range, 50–465] |
0.245 |
| Sonographic findings | |||
| Hyperperfusion (>100% compared to the unaffected testis) within the entire affected testis (presence/absence) (n/N) | 0/7 | 8/7 | 0.023 |
| Echogenicity within the affected testis (heterogeneous/homogeneous) (n/N) | 2/5 | 2/13 | 0.565 |
- * Spermatic cord twisting was not recorded in five patients.
There was a significant difference in hyperperfusion within the entire affected testis (with atrophy [present/absent] vs. without atrophy [present/absent] = 0/7 vs. 8/7, p = 0.023) between patients with and without testicular atrophy.
The atrophy and non-atrophy groups exhibited no significant differences in terms of affected side (with atrophy [left/right] vs. without atrophy [left/right] = 7/0 vs. 10/5, p = 0.135), direction of testicular torsion (with atrophy [inner/outer] vs. without atrophy [inner/outer] = 4/3 vs. 12/3 p = 0.334), age (13.4 ± 1.6 years [range, 11–16] vs. 13.5 ± 0.8 years, [range, 13–15], p = 0.849), duration of symptoms (with atrophy vs. without atrophy = 7 ± 3.3 h [range, 3–12] vs. 4.7 ± 3.6 h [range, 2–14], p = 0.075), degree of spermatic cord twisting (390 ± 73.5 degrees [range, 360–540] vs. 490.9 ± 141.5 degrees [range, 360–702], p = 0.123), interval from manual detorsion to subsequent surgical exploration (with atrophy vs. without atrophy = 23.3 ± 30.5 days [range, 1–78] vs. 19.7 ± 20.0 days [range, 0–70] p = 0.832), treatment via fasciotomy (atrophy with/without fasciotomy vs. without atrophy with/without fasciotomy = 0/7 vs. 2/13, p = 1), interval from manual detorsion to the last evaluation of testicular size (with atrophy vs. without atrophy = 133.7 ± 105.3 days [range, 49–348] vs. 206.1 ± 145.5 days [range, 50–465] p = 0.245), or echogenicity within the testis (with atrophy [heterogeneous/homogeneous] vs. without atrophy [heterogeneous/homogeneous] = 2/5 vs. 2/13, p = 0.565).
Discussion
In this small cohort study, the presence of hyperperfusion within the entire affected testis, immediately after successful manual detorsion, was useful for predicting the avoidance of testicular atrophy. When this finding was absent, testicular atrophy could not be avoided in all the cases. The presence of hyperperfusion, within the entire affected testis, after successful manual detorsion, could represent that the absence of segmental hypoperfusion and the absence of hyperperfusion, within the entire affected testis after successful manual detorsion, could indicate segmental infarction of the testis or testicular compartment syndrome after reperfusion.9, 10, 12, 14, 20
The terminal branch of the testicular artery supplies blood to the upper pole of the testis, and the interruption of blood flood to this area leads to segmental infarction and subsequent testicular infarction and atrophy.12, 14, 20 In such cases, infarction and atrophy are unavoidable because segmental testicular necrosis occurs before reperfusion. Segmental testicular necrosis or arterial occlusion may result in sonographic hypoperfusion within the affected testis and the inability to detect vascular flow following successful manual detorsion.2, 4, 5, 13, 14, 16, 17, 20 In our cohort, hyperperfusion within the entire affected testis suggested the absence of a necrotic area in the affected testis.
The testis is enclosed by the tunica albuginea, which is strong and inelastic.9, 10, 12, 20 Testicular compartment syndrome is characterised by the reperfusion-induced increase in intratesticular pressure following testicular detorsion, resulting in testicular parenchymal oedema and subclinical ischemic damage.9-12, 20 Fasciotomy is the treatment of choice for testicular compartment syndrome.9-12, 20 In our cohort, the presence of hyperperfusion within the entire testis usually implied that intratesticular pressure did not increase. In this study, two patients who underwent fasciotomy did not exhibit testicular atrophy (Figure 2). This procedure may help prevent testicular compartment syndrome. Manual detorsion is recommended to decrease the ischemic time of the testis; however, our results indicate that this procedure may be insufficient for preventing testicular atrophy without surgical exploration.
In the current study, some patients without testicular atrophy did not exhibit hyperperfusion within the entire testis. Although the best time at which reperfusion can be observed on ultrasound following manual detorsion has not been determined, some studies have reported that reperfusion may be detectable within hours after detorsion.9-12 In these cases, the final state of hyperperfusion may not be detectable on ultrasound. Hence, multiple sonographic examinations may be necessary to detect hyperperfusion within the entire testis after successful manual detorsion.
Echogenicity within the testis has been reported to be an important finding in cases of testicular necrosis.2, 3, 16-18, 21, 22 In our cohort, two patients with heterogeneous echogenicity within the affected testis exhibited testicular atrophy. However, the small number of patients with this sonographic feature may have affected the results.
The degree of spermatic cord twisting, which can increase or decrease during testicular torsion,1, 18 was not fixed and did not predict testicular atrophy in our cohort. Symptom duration is an important predictor of testicular loss and tended to be higher in the group with testicular atrophy.
Despite the small sample size, the results suggest that sonographic features are helpful in the management of patients with testicular torsion after manual detorsion. Hyperperfusion within the entire affected testis immediately after successful manual detorsion may indicate the absence of complications, such as testicular necrosis or testicular compartment syndrome. Conversely, the absence of this feature suggests the presence of complications, and surgical exploration, including fasciotomy, is recommended. Therefore, future studies are necessary to compare the testicular size between patients who undergo emergency surgery, including fasciotomy immediately after successful manual detorsion, and those who undergo elective surgery.
Our study has certain limitations. First, the outcome was the evaluation of the testicular volume, and the time of ultrasonographic evaluation of testicular atrophy varied among the patients. Second, the impact of testicular atrophy on hormone production and fertility was not investigated. Third, image acquisition depended on operator skills and experience. In addition, the evaluations of vascular follow were subjective, which might have affected the results, although sonograms were obtained by experienced radiologists. Fourth, the number of patients was small, and the study had a retrospective design. Thus, additional studies with larger sample sizes and long-term prospective designs are required to validate our findings.
Conclusion
This small cohort study suggests that the presence of hyperperfusion within the entire affected testis immediately after successful manual detorsion is useful in predicting the avoidance of testicular atrophy.
Acknowledgements
We would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for English language.
Authorship statement
T.H. and Y.T. designed the study; A.U, Y.S, T.I, K.O. and H.K. collected and analyzed the data; T.H. wrote the manuscript; T.H. and E.O. critically reviewed the manuscript and supervised the whole study process. All authors have read and approved the final manuscript.
Funding
No funding information is provided.
Conflict of interest
The authors declare no conflict of interest.