Paediatric orbital ultrasound: Tips and tricks
Abstract
Background
The orbital structures are ideally suited for ultrasound examination due to their superficial location and cystic composition of the eye. However, orbital ultrasound remains an underutilised modality due to preference for other cross-sectional modalities in general practice.
Aim
In this article, we review the basic principles, clinical uses and technique of orbital ultrasound in peadiatric patients.
Materials and methods
The clinical utility of orbital ultrasound in peadiatric patients is demonstrated using selected cases.
Results
Ultrasound is useful in the diagnosis of various posterior segment pathologies, especially in conditions causing opacification of light-conducting media of the eye. It is also beneficial in diagnosing various orbital pathologies, particularly in differentiating solid from cystic lesions.
Discussion
The added advantages of its use in children include lack of ionising radiation and reduced requirement of sedation or general anesthesia. Ultrasound is the most practical initial investigation in cases where ophthalmoscopy is limited by opacification of ocular media. The addition of color Doppler on ultrasound can give additional information about the vascularity of the lesion.
Conclusion
Use of ultrasound can be streamlined into the workup of various orbital and ocular pathologies either as an initial investigation or as a problem-solving tool in cases with a diagnostic dilemma on other modalities.
Introduction
Orbital ultrasound is a very valuable modality, especially in the paediatric age group. However, owing to lack of adequate training and over-dependence of radiologists on magnetic resonance imaging (MRI), it remains relatively underutilised. The superficial location and cystic composition of the eye make it ideally suited for ultrasound examination, particularly with the advent of high-frequency transducers. Ultrasound examination is rapid, cost-effective, easily available and enables dynamic study of the orbital structures. The added advantages of its use in children include lack of ionising radiation, reduced requirement of sedation or general anaesthesia and a quick comprehensive evaluation in an often apprehensive child.1 Detailed cross-sectional anatomy of the entire globe and surrounding orbital structures can be visualised using conventional ultrasound transducers. The cornea and anterior chamber structures of the eye rarely require ultrasound as they are amenable to clinical inspection, slit lamp and ophthalmoscopic examination. However, B-mode ultrasound can help in diagnosis of various posterior segment pathologies especially in conditions causing opacification of light-conducting media of the eye. Ophthalmologists have long been using ultrasound for eye examination, often with dedicated equipment such as biomicroscope. However, radiologists are increasingly recognising the role of orbital ultrasound, usually as an adjunct to other cross-sectional modalities. In select situations, ultrasound can even act as a problem-solving tool owing to its better resolution and solid-cystic differentiation. Herein, we will mention the basic principles, clinical uses and techniques of orbital ultrasound in paediatric patients.
Clinical problems and uses
Paediatric ophthalmic pathologies are not an uncommon clinical occurrence. The most common presentations include leukocoria, strabismus, proptosis and delayed visual development. Ophthalmic pathologies can broadly be categorised into ocular and extraocular diseases.
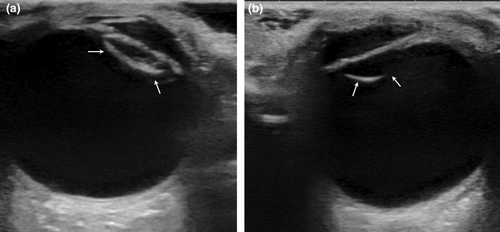
In case of ocular diseases, initial examination is often done by ophthalmologists using slit lamp, ophthalmoscopy and A-mode ultrasound. General B-mode ultrasound is especially useful in cases where there is opacification of the light-conducting media of the eye as a result of cataract, vitreous haemorrhage or hyphema, which leads to obscuration of the posterior segment of the eye on ophthalmoscopic examination. In such cases, B-mode ultrasound can visualise the posterior structures of the globe and help in diagnosing the underlying pathology (Figures 1 and 2). Another important indication for ocular ultrasound is for further workup and characterisation of a mass identified during ophthalmoscopy. Sonographic characteristics that help in formulating differential diagnoses include echogenicity and shape of the mass, its relationship to the coats of the eyeball and the presence of calcifications. Although computed tomography (CT) and MRI are also useful in patients with ocular masses, Ultrasound has been shown to have a better resolution for small lesions (<2 mm size).2 Ultrasound can also delineate a mass underlying a retinal detachment which can be difficult to detect on ophthalmoscopy. Interrogation of the mass with colour Doppler can show its internal vascularity and can help in confidently diagnosing pathologies with a characteristic vascular supply, such as persistent fetal vasculature (PFV).
Ultrasound is also beneficial in diagnosing various orbital pathologies. In the evaluation of a case of periorbital cellulitis, ultrasound is an excellent modality to delineate any drainable liquefied abscesses.3 In case of vascular malformations, ultrasound can show their cystic nature and help characterise them into slow- or high-flow lesions on the basis of their vascularity. Retro-orbital deep-seated lesions causing proptosis are not amenable to clinical or ophthalmic evaluation. Ultrasound can be a first quick imaging tool to ascertain the nature of pathology and suggest further investigations accordingly.
Basic technique and interpretation
Before starting the procedure, it is usually helpful to give a detailed explanation of the examination to alleviate any anxiety the patient or their parents might have. The ultrasound is then performed, with the patient lying in supine position with their eyes closed, by scanning through the eyelids. Ample amount of gel is necessary to ensure adequate contact and examination of the superficial part of the globe.4
Linear high-frequency (5–12 MHz or higher if available) transducers should be used to evaluate the eye. A smaller footprint linear transducer, such as a hockey stick transducer, facilitates easy contact with the eyelid. The transducer settings should include multiple focal zones over the field of view and sufficient depth to encompass the entire globe as well as the retrobulbar fat and extraocular muscles in the field of view. Transducer pressure should be kept to a minimum to avoid collapse of the anterior chamber structures especially in cases of traumatic eye injuries. Low-gain settings help to delineate thin echogenic structures (such as cornea and lens capsule) in the anechoic background of aqueous and vitreous humour. Increasing the brightness is beneficial to demonstrate any debris or haemorrhage in the vitreous.5 Both the globes are scanned in their entirety systematically in axial view from superior to inferior and sagittal view from lateral to medial. Dynamic images with gentle eye movements can show motion of echoes in vitreous and improves visualisation of extraocular muscles.6 The addition of colour Doppler using low-velocity settings can help to demonstrate any abnormal vascularity especially in a case of retrolental soft-tissue or an intraocular mass.
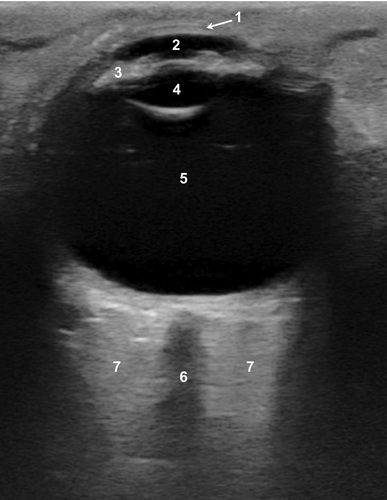
Table 1 describes the normal ultrasound appearance of the various structures of the eye. The anechoic fluid contents of the globe help in easy delineation of normal anatomy as echogenic lines in an anechoic background (Figure 3).
| Structure | Appearance | Comments |
|---|---|---|
| Cornea | Most anterior convex echogenic line | Transducer pressure kept minimum to avoid anterior chamber collapse |
| Lens | Anechoic with thin echogenic anterior and posterior capsules | Anterior chamber is present between cornea and lens |
| Ciliary bodies | Hypoechoic | Seen on both sides of lens |
| Vitreous | Anechoic area posterior to lens | Use high-gain settings to look for vitreous debris or haemorrhage |
| Posterior wall | Concave echogenic line | All three layers—retina, choroid and sclera—are seen as a single echogenic line interrupted by optic disc |
| Optic nerve | Hypoechoic band posterior to optic disc | – |
| Retrobulbar fat | Hyperechoic | – |
| Extraocular muscles | Hypoechoic | Dynamic imaging with moderate eye movements helps in better visualisation |
Despite the obvious utility of ultrasound for paediatric orbital pathologies, the examination can often be compromised due to an anxious, uncooperative child and the inability of children to follow instructions due to their age, medical condition or development. Ocular movements during the examination may preclude optimal visualisation of anatomy. Whenever feasible in neonates and toddlers, ultrasound should be planned in the same sitting with another examination being done under anaesthesia. Other practical tips while scanning paediatric patients have been tabulated in Table 2.
Calming techniques for anxious child
|
| Clear instructions to the parents and patient (older children) before starting exam |
| Scan the worse eye first |
| Short scan time |
| Comparison with contralateral eye using dual screen function and same scanning parameters |
Biosafety concerns and their alleviation
Potential bioeffects from ultrasound can arise from two different mechanisms: thermal and mechanical. Although diagnostic ultrasound has not been demonstrated to cause ocular damage, it is worth noting that for ocular ultrasound, the maximum recommended values for thermal index (TI) and mechanical index (MI) are significantly lower than rest of the body tissues. In general, TI should be kept <1.0 and MI <0.3 while insonating the eye. Always using a factory-installed ocular present, using high-gain setting instead of high-power output and utilising minimum scan time for diagnostic quality images as per the ALARA (as low as reasonably achievable) principle significantly lessens the likelihood of an ocular injury. Doppler examination is associated with high acoustic power output and thus, indiscriminate use of Doppler during ocular examination should be avoided. Currently, there are no established indications for the use of elastography in ocular ultrasound and should be used cautiously in research settings as the acoustic output used in this modality is significantly higher than B-mode ultrasound.7
Case 1
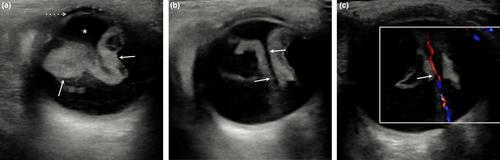
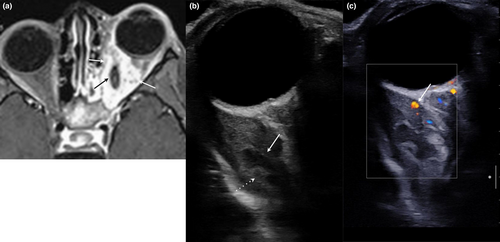
A 3-month-old boy presented to the outpatient department with a complaint of leukocoria in left eye since birth. There was no redness, excessive watering or headache. Ultrasound showed the presence of irregular lobulated echogenic soft-tissue mass in the retrolental location suspicious for a neoplasm (Figure 4a). Multiple low-level echoes were also seen in the surrounding vitreous suggestive of vitreous haemorrhage. Colour Doppler showed the presence of a linear vascular channel extending from the posterior wall of the lens to optic disc suggestive of a persistent hyaloid artery (Figure 4b,c). Based on the characteristic Doppler findings, a diagnosis of PFV was made.
Case 2
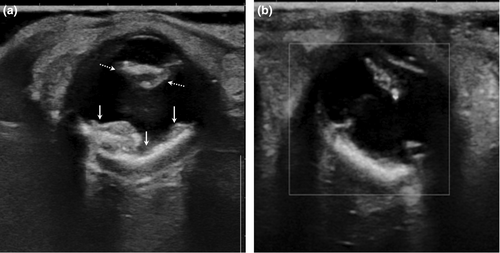
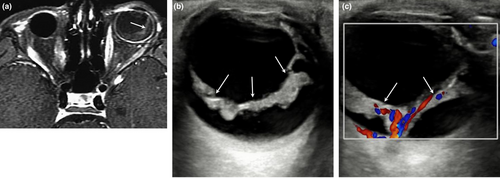
A 6-year-old boy presented with retro-ocular pain and restriction of movement in left eye for the last 6 months. There was no proptosis, fever or other systemic symptoms. An MRI previously done showed a bulky hyperenhancing left medial rectus muscle (Figure 5a). Ultrasound showed increased bulk of medial rectus muscle belly with the presence of an intramuscular well-defined cystic lesion. An eccentric echogenic focus was also seen within the cystic lesion suggestive of a scolex and a diagnosis of myocysticercus was made (Figure 5b,c). The child was put on a medical treatment of cysticercosis, with added steroids.
Case 3
A 7-year-old boy, a known case of bilateral intraocular retinoblastoma, came for a routine follow-up hospital visit. He underwent right eye enucleation and chemotherapy 6 years back. Initial post-chemotherapy, MRI showed resolution of left eye mass. However, on a follow-up MRI, there was the presence of retinal detachment in the left eye with suspicious retinal thickening noted on post-contrast images (Figure 6a). On ultrasound, diffuse nodular retinal thickening was easily appreciated which was suggestive of recurrence (Figure 6b,c). Patient was subsequently started on augmented chemotherapy.
Discussion
A wide variety of intraocular and orbital pathologies affect the paediatric population. These include diverse neoplasms which can be divided into intraocular lesions (such as retinoblastoma, medulloepithelioma and retinal hamartoma) and orbital lesions (such as rhabdomyosarcoma, neuroblastoma metastases, leukaemic deposits, optic pathway gliomas and neurofibromas). Other pathologies include congenital anomalies (PFV and coloboma), inflammatory pseudotumor, infections and vascular malformations. Presenting clinical findings may include leukocoria (white pupillary reflex), restricted eye movements, strabismus, loss of vision or inflammatory signs.8 The initial detection or suspicion of pathology is usually done on an ophthalmological examination which is followed by further radiological workup. Clinically unequivocal retinoblastoma needs contrast-enhanced MRI for local staging. In case of clinically doubtful diagnosis, alternative imaging modalities may be required. Ultrasound fits this situation perfectly because of its easy availability, and excellent spatial resolution and solid/cystic tissue characterisation.
First, ultrasound is the most practical initial investigation in cases where ophthalmoscopy is limited by opacification of ocular media. In such a scenario, ultrasound can give a view of the entire globe and extraocular structures and visualise the underlying pathology. The next pertinent diagnostic investigation can then be decided and tailored based on the ultrasound findings. Suspicion of calcifications or a bony lesion on ultrasound requires a CT scan for further evaluations. However, MRI is a better option for further imaging of ocular and orbital soft-tissue masses.
Second, addition of colour Doppler can give additional information about the vascularity of the lesion which is not available on CT and MRI without contrast injection. Specifically, as in our case no. 1, a Doppler examination can demonstrate the abnormal persistent hyaloid artery within an echogenic retrolental mass extending from posterior lens capsule to optic disc in a case of PFV.9 This is a diagnostic finding for PFV and is poorly visualised on other modalities including CT and MRI. Other imaging findings described in PFV include microphthalmos, shallow anterior chamber, retinal detachment and abnormal lental morphology.10 A close clinical and imaging differential for PFV is retinoblastoma. The presence of calcifications, normal or increased size of the affected globe and bilaterality are the imaging features which favour a diagnosis of retinoblastoma.11 However, upto 10% cases of PFV can also show bilaterality, and in intricate cases, ultrasound and Doppler examination can help in reaching the correct diagnosis.
Third, as anywhere else in the body, ultrasound helps in better characterisation of vascular malformations by demonstrating the cystic areas as well as the type of blood flow in these lesions. However, CT and MRI can better visualise the extent of involvement and vascular supply of these lesions. Another advantage of ultrasound is that it can be easily performed using dynamic manoeuvres such as Valsalva. On straining, the venous channels get distended and show increased blood flow which can be easily seen on ultrasound.12 Capillary haemangiomas constitute the most common intraorbital vascular tumours in childhood. On ultrasound, these lesions appear hyperechoic, show internal vascularity and lack cystic spaces. Lobulated shape, intense contrast enhancement and intralesional flow voids on CT or MRI are helpful diagnostic features.12
Lastly, in a case of myocysticercus, the underlying cystic lesion may be obscured on CT or MRI because of the increased bulk and oedema in the surrounding muscle tissue. The appearance may be mistaken for cellulitis or pseudotumor on these modalities. However, as shown in our case no. 2, ultrasound is an excellent modality to demonstrate the echogenic scolex within the cyst of myocysticercus and helps in making the correct diagnosis.13
One of the recent ultrasound advances, contrast-enhanced ultrasound (CEUS), can help in better characterisation and delineation of extent of the tumours by showing differential enhancement as compared with the normal structures of the globe and the optic nerve.14 CEUS also holds a great potential as a non-invasive modality for follow-up of retinoblastoma patients on chemotherapy as these patients may have a higher susceptibility to develop radiation-induced neoplasms.
Orbital ultrasound remains a less recognised modality due to preference for other cross-sectional modalities such as CT and MRI in general practice. Table 3 summarises the situations where ultrasound alone can be diagnostic, and where it can be a useful complementary tool. Overall sensitivity of ultrasound for detecting orbital lesions has been reported to be as high as 94%.15 In paediatric patients with orbital pathologies, ultrasound is an excellent modality owing to its inherent benefits of lack of radiation and no need for sedation. Use of ultrasound can thus be streamlined into the workup of orbital and ocular pathologies as an initial step to decide further best investigation, as a problem-solving tool in cases with a diagnostic dilemma on other modalities and for follow-up of cancer patients on a case-to-case basis.
| Conditions where ultrasound can be used as a primary imaging modality | Conditions where ultrasound acts as problem-solving tool, even after Computed Tomography (CT)/ Magnetic Resonance Imaging (MRI) | Conditions where ultrasound is not useful as a primary imaging modality |
|---|---|---|
| Leukocoria | Treated retinoblastoma, presenting with equivocal nonenhancing mass on MRI | Suspected intracranial extension of ocular mass |
| Visible orbital swelling/ masses (ocular as well as extraocular) | Nonenhancing mass in the background of vitreous haemorrhage | Orbital injury, with suspected globe rupture |
| Suspected secondary retinal detachment, where posterior chamber opacity precludes ophthalmoscopic examination | Orbital vascular malformations | Neuro-ophthalmological disorders |
Author contributions
Amit Gupta: Data curation (equal); investigation (equal); writing – original draft (equal). Shilpa Khanna Arora: Data curation (equal); methodology (equal). Rachna Seth: Supervision (equal); writing – review and editing (equal). Rakesh Kumar: Data curation (equal); methodology (equal). Manisha Jana: Supervision (equal); writing – original draft (equal); writing – review and editing (equal).
Authorship statement
Amit Gupta: Data Curation, Investigation, Writing – Original draft; Shilpa Khanna Arora: Data Curation, Methodology; Rachna Seth: Supervision, Writing – Review and Editing; Rakesh Kumar: Data Curation, Methodology; Manisha Jana: Supervision, Writing – Original draft, Writing – Review and Editing
Funding
No funding information is provided.
Conflict of interest
There is no conflict of interest.
Patient consent
Prior parent/guardian consent was taken for performing the ultrasound examination and use of images for publishing purposes at a later date.




