Effects of the COVID-19 pandemic on gastroenterological surgeries in 2020: A study using the National Clinical Database of Japan
[Correction added on 19 January 2023, after first online publication: The copyright line has been corrected.]
Abstract
Aim
This study aimed to investigate the effect of the coronavirus disease pandemic on the number of surgeries for gastroenterological cancer cases in Japan.
Methods
The data recorded in the National Clinical Database of Japan between 2018 and 2020 were utilized for this study. Five specific surgeries for primary cancers and surgery for acute diffuse peritonitis were considered the primary endpoints. We divided the study period into the prepandemic and postpandemic (after April 2020) periods and examined the number of surgeries in relation to clinical factors.
Results
Overall, 228 860 surgeries were analyzed. Among the five primary cancer surgeries, the number of distal gastrectomies for gastric cancer decreased the most (to 81.0% of the monthly number in the prepandemic period), followed by that of low anterior resections for rectal cancer (91.4%). In contrast, the number of pancreaticoduodenectomies for pancreatic cancer increased by 7.1%, while that of surgeries for peritonitis remained stable. This trend was observed nationwide. We also noted a marked reduction in the number of distal gastrectomy (to 72.5%), low anterior resection (84.0%), and esophagectomy (88.8%) procedures for T1 tumors. The noncurative resection rate and mortalities were low despite the increased proportion of T4 tumors and older patients.
Conclusion
A marked reduction in surgeries for gastric and rectal cancers with early T factors may reflect prioritization of surgeries and reduction in cancer screenings. Although the quality of the surgery was maintained in terms of reduced mortalities and morbidities, the long-term effects of this pandemic should be monitored.
1 INTRODUCTION
Since the early report was published,1 COVID-19 caused by the novel coronavirus (SARS-CoV-2) has resulted in a global pandemic with a high mortality rate.2 At the end of 2020, more than 80 million people worldwide were infected with SARS-CoV-2 and its variant strains, and more than 1.9 million people succumbed to this infection.3 In Japan, the infection rate increased later than that in the Western countries, and the government declared a state of emergency in April 2020 to curb the spread of the virus. During this unprecedented pandemic, government and medical institutions continuously faced two conflicting challenges: treating patients with COVID-19 without acquiring the infection or resulting in nosocomial infections, and maintaining hospital functions at the same level as before,4 especially for critically ill patients, such as patients with malignant diseases and acute abdomen.
A delay in cancer treatment results in worse treatment outcomes.5, 6 A previous study using data from the National Clinical Database provided a perspective of decreased surgical activities in Japan,7 suggestive of delay/loss of cancer treatment. However, a detailed analysis remains to be conducted. Thus, we investigated the effect of the COVID-19 pandemic on the rate of performance of gastrointestinal cancer surgeries in 2020. We intended to focus on the group of patients requiring more attention in our society. We also explored the distribution of surgical cases considering different clinical characteristics, such as age, sex, and tumor–node–metastasis (TNM) factors, and evaluated the short-term results of those surgeries.
2 METHODS
2.1 Patients
The protocol of this study was reviewed and adopted by the Japanese Society of Gastrointestinal Surgery Committee and approved by the Institutional Review Board of Kochi Medical School with the exemption of individual written informed consent (ID: 2021-82).
This study was conducted by utilizing data from the National Clinical Database of Japan; estimated coverage exceeds 90% of the procedures with high data accuracy.8-10 We selected five types of surgeries for primary cancers: distal gastrectomy (DG) for gastric cancer, low anterior resection (LAR) for rectal cancer, esophagectomy (Eso) for esophageal cancer, hepatectomy (Hep) for hepatocellular carcinoma (HCC), and pancreaticoduodenectomy (PD) for pancreatic cancer. Hep was limited to segmentectomy (lateral segmentectomy was excluded) or a larger part of the resection.11 Surgery for acute diffuse peritonitis was also analyzed because we considered that the numbers of this surgery would be stable, and mortality related to acute abdomen was an important indicator for a change in treatment quality. Patients who underwent any of the aforementioned surgeries were selected. Patients with benign tumors or tumors of other organs, aged <18 y, who underwent emergency cancer-related surgery, with T0 or Tis tumors, and with missing data were excluded (Figure S1).
2.2 Endpoints
The primary endpoint was the number of surgeries conducted. The secondary endpoint was determining the effects with different clinical variables, such as age, sex, TNM classification, and cumulative incidence of COVID-19 infections. In addition, 30-d mortalities, surgical mortalities, R0 resection rates, and rates of postoperative complications with Clavien–Dindo classification grade ≥3 were investigated. Surgical mortality is the sum of any 30-d mortality or in-hospital death within 90 d.
2.3 Statistical considerations
We did not conduct any statistical comparisons to ensure that we focused on the description of the data and the overall picture of the change in the number of surgeries performed for cancers in the context of clinical variables. The 3 y were divided into two terms (before the state of emergency [28 mo from January 2018 to April 2020] and after the state of emergency [8 mo from May 2020 to December 2020]) because this would clearly depict the effect of the COVID-19 pandemic. In addition, we investigated the number of surgeries performed in 12 prefectures (of 48 prefectures constituting the country) with a high cumulative incidence (Data S1) to analyze whether the infection itself affected the surgical treatment or other factors had greater influence on the observed results.
3 RESULTS
Overall, 228 860 cases were identified (Table 1; Table S1); 130 840 (57.2%) were from areas with a high cumulative incidence of COVID-19. The number of surgeries performed for gastroenterological cancers changed in 2020, compared with those in 2018 and 2019, while the number of surgeries performed for peritonitis remained stable (Table S1). The degree of change was evident when the number of surgeries per month was compared (Table 1). The number of DGs decreased to 81.0% of the number per month before the pandemic, followed by those of LARs (91.4%), Heps (93.3%), and Esos (96.9%), whereas the number of PDs increased by 7.1%. When we focused on areas with greater infection rates, similar changes in the number of surgeries per month were found (Table 1).
| Total n = 228 860 | DG n = 88 627 | LAR n = 55 842 | Eso n = 17 351 | Hep n = 8201 | PD n = 16 668 | ADP n = 42 171 | |
|---|---|---|---|---|---|---|---|
| Entire country | |||||||
| Number of surgeries per month, n | |||||||
| January 2018 to April 2020 | 6490 | 2570 | 1582 | 485 | 231 | 456 | 1166 |
| May 2020 to December 2020 | 5892 | 2082 | 1445 | 470 | 216 | 488 | 1191 |
| Change after state of emergencya, % | 91 | 81 | 91 | 97 | 93 | 107 | 102 |
| Areas with high rates of infection | |||||||
| Number of surgeries per mo, n | |||||||
| January 2018 to April 2020 | 3709 | 1421 | 930 | 314 | 132 | 271 | 640 |
| May 2020 to December 2020 | 3375 | 1127 | 857 | 301 | 128 | 300 | 662 |
| Change after state of emergencya, % | 91 | 79 | 92 | 96 | 96 | 111 | 103 |
- Abbreviations: ADP, acute diffuse peritonitis; DG, distal gastrectomy; Eso, esophagectomy; Hep, hepatectomy; LAR, low anterior resection; PD, pancreaticoduodenectomy.
- a Change in the number of surgeries per month calculated using the equation
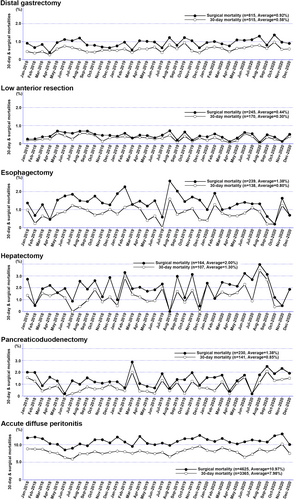
The analysis of monthly surgical cases revealed a steep decline in DGs in May 2020, which slightly increased toward the end of the year but did not reach levels of the previous 2 y (Figure 1). Similarly, the number of LARs dropped in May 2020, which recovered in October. However, the rebound (compensation) of the decreased cases was not observed in 2020. The change in the number of Heps for HCC was similar to that of LARs, although the change was smaller. Changes in the number of surgeries nationwide as well as in the 12 prefectures with a high cumulative incidence of infection were similar (Figure 1; Table 1).
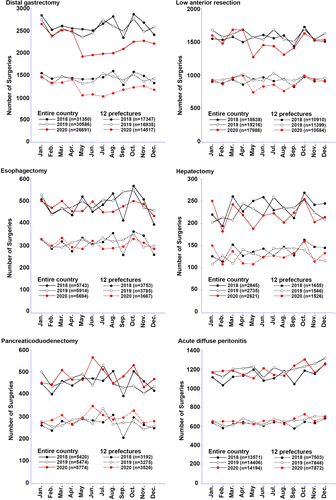
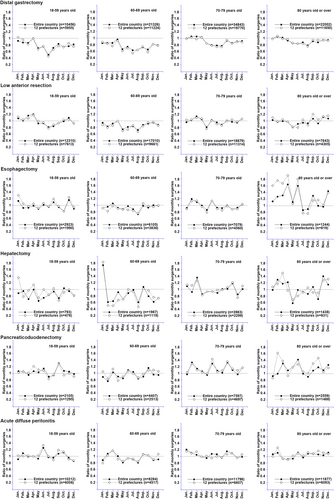
3.1 Age and sex
When patients were divided according to their age at operation, we found that younger patients experienced a greater effect of the COVID-19 pandemic (Table 2), which is also shown in an analysis by year (Table S2). DGs for patients aged 18–59 y decreased to 71.7% of those of the previous period, while DGs for patients aged >80 y decreased to 90%. Similar trends were found for patients who underwent LAR and Hep. For both DG and LAR, the decline in the number of surgeries in May 2020 was also higher among younger patients, while the number of surgeries for older patients showed a slight decline and recovered around September 2020 (Figure 2). Concerning PD, the main reason for the increase in the number of operations in 2020 appeared to be the increased number of older patients (aged 70–79 and >80 y). The change in the number of surgeries after the pandemic was similar among women and men (Table 2; Table S2; Figure S2).
| Age groups (y) | Sex | |||||
|---|---|---|---|---|---|---|
| 18–59 | 60–69 | 70–79 | 80< | Women | Men | |
| DG (n = 88 627) | ||||||
| n (% of total cases) | 10 456 (11.8) | 21 326 (24.1) | 34 843 (39.3) | 22 002 (24.8) | 29 210 (33.0) | 59 417 (67.0) |
| Rate of change, % | 71.7 | 69.6 | 85.6 | 90.0 | 79.5 | 81.8 |
| LAR (n = 55 842) | ||||||
| n (% of total cases) | 12 310 (22.0) | 17 010 (30.5) | 18 879 (33.8) | 7643 (13.7) | 19 286 (34.5) | 36 556 (65.5) |
| Rate of change, % | 91.1 | 83.8 | 95.4 | 99.1 | 92.1 | 90.9 |
| Eso (n = 17 351) | ||||||
| n (% of total cases) | 2923 (16.8) | 6105 (35.2) | 7079 (40.8) | 1244 (7.2) | 3307 (19.1) | 14 044 (80.9) |
| Rate of change, % | 98.1 | 93.3 | 97.3 | 110.3 | 97.2 | 96.9 |
| Hep (n = 8201) | ||||||
| n (% of total cases) | 793 (9.67) | 1987 (24.2) | 3983 (48.6) | 1438 (17.5) | 1579 (19.3) | 6622 (80.7) |
| Rate of change, % | 87.1 | 80.9 | 99.8 | 96.6 | 95.3 | 92.8 |
| PD (n = 16 668) | ||||||
| n (% of total cases) | 2105 (12.6) | 4407 (26.4) | 7597 (45.6) | 2559 (15.4) | 7365 (44.2) | 9303 (55.8) |
| Rate of change, % | 107.6 | 95.3 | 111.1 | 115.8 | 106.1 | 107.8 |
| ADP (n = 42 171) | ||||||
| n (% of total cases) | 10 212 (24.2) | 8284 (19.6) | 11 798 (28.0) | 11 877 (28.2) | 17 268 (40.9) | 24 903 (59.1) |
| Rate of change, % | 101.2 | 93.6 | 105.7 | 105.5 | 104.1 | 100.8 |
- Note: Rate of change: Change in the number of surgeries per month calculated using the equation .
- Abbreviations: ADP, acute diffuse peritonitis; DG, distal gastrectomy; Eso, esophagectomy; Hep, hepatectomy; LAR, low anterior resection; PD, pancreaticoduodenectomy.
3.2 TNM of cancers
For T1 and T2 tumors, the number of surgeries decreased, except for pancreatic cancer. Since T1 tumors represent 49.2% of the gastric cancers treated via DG, the effect on the total number of surgical cases was large (Table 3; Table S3; Figure 3). The number of surgeries for T1 gastric cancer dropped in May 2020 and did not recover to levels of the previous 2 y, similar to that for T3 and T4 gastric cancers. The lowest numbers of T1 tumors of the stomach (DG), rectum (LAR), and esophagus (Eso) were operated upon in July, August, and August, respectively. Similarly, surgeries for T1 and T2 HCC decreased after the pandemic by ~8%. Meanwhile, the number of PD for T1 and T2 pancreatic cancers increased, even after the spread of COVID-19.
| T factors | ||||
|---|---|---|---|---|
| T1 | T2 | T3 | T4 | |
| DG (n = 88 627) | ||||
| N (% of total cases) | 43 574 (49.2) | 12 265 (13.8) | 16 136 (18.2) | 16 652 (18.8) |
| Rate of change, % | 72.5 | 82.8 | 89.7 | 94.6 |
| LAR (n = 55 842) | ||||
| n (% of total cases) | 8442 (15.1) | 9994 (17.9) | 27 833 (49.8) | 9573 (17.1) |
| Rate of change, % | 84.0 | 87.4 | 93.2 | 96.8 |
| Eso (n = 17 351) | ||||
| n (% of total cases) | 6362 (36.7) | 2616 (15.1) | 7082 (40.8) | 1291 (7.4) |
| Rate of change, % | 88.8 | 93.2 | 103.7 | 109.2 |
| Hep (n = 8201) | ||||
| n (% of total cases) | 2813 (34.3) | 3130 (38.2) | 1595 (19.4) | 663 (8.1) |
| Rate of change, % | 92.3 | 92.6 | 102.4 | 79.7 |
| PD (n = 16 668) | ||||
| n (% of total cases) | 3254 (19.5) | 6569 (39.4) | 6471 (38.8) | 374 (2.2) |
| Rate of change, % | 119.3 | 105.5 | 104.3 | 80.6 |
- Note: Rate of change: Change in the number of surgeries per month calculated using the equation
- Abbreviations: ADP, acute diffuse peritonitis; DG, distal gastrectomy; Eso, esophagectomy; Hep, hepatectomy; LAR, low anterior resection; PD, pancreaticoduodenectomy.
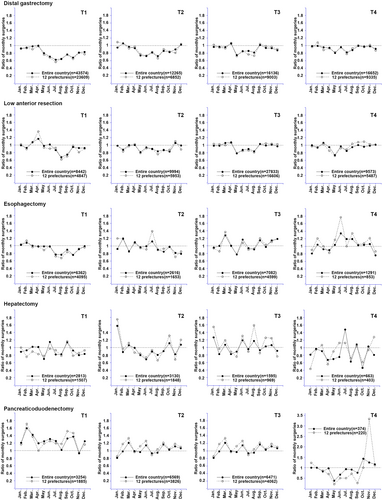
Lymph node metastases were observed in 40%–60% of surgical cases, except in Hep for HCC. A small fraction of patients had distant metastases, with the highest prevalence in LAR cases. The number of surgeries for tumors with nodal and distant metastases was generally low. For instance, the number of DGs for patients with a negative nodal status decreased and for longer (Tables S4 and S5). Meanwhile, the number of PDs for N0 tumors increased.
3.3 Short-term results
The R0 resection rate did not show any remarkable change in all types of surgeries (Table 4; Table S6), despite the increase in the proportion of T4 tumors or tumors with metastasis in DG, LAR, and Eso cases. A slight increase in the number of severe complications was observed in DG, Hep, and PD cases, which may reflect the increased proportion of older patients. The monthly rates of mortalities were stable in DG, LAR, Eso, and ADP cases (Figure 4; Figure S3). A slight increase in mortality after Hep and PD was observed, while a reduction in mortality was observed after LAR and Eso.
| DG | LAR | Eso | Hep | PD | ADP | |
|---|---|---|---|---|---|---|
| R0 resection rate, n (%) | ||||||
| January 2018 to April 2020 | 68 198 (94.8) | 41 549 (93.8) | 12 753 (93.9) | 6173 (95.3) | 11 590 (90.8) | – |
| May 2020 to December 2020 | 15 677 (94.1) | 10 809 (93.5) | 3535 (93.9) | 1652 (95.7) | 3585 (91.8) | – |
| Complications (CD ≥3), n (%) | ||||||
| January 2018 to April 2020 | 4512 (6.3) | 4890 (11.0) | 3078 (22.7) | 829 (12.8) | 2103 (16.5) | 8235 (25.2) |
| May 2020 to December 2020 | 1208 (7.3) | 1275 (11.0) | 848 (22.5) | 248 (14.4) | 675 (17.2) | 2434 (25.6) |
| 30-d mortality, n (%) | ||||||
| January 2018 to April 2020 | 398 (0.6) | 137 (0.3) | 111 (0.8) | 78 (1.2) | 91 (0.7) | 2596 (8.0) |
| May 2020 to December 2020 | 117 (0.7) | 33 (0.3) | 27 (0.7) | 29 (1.7) | 50 (1.3) | 769 (8.1) |
| Surgical mortality, n (%) | ||||||
| January 2018 to April 2020 | 635 (0.9) | 200 (0.5) | 199 (1.5) | 124 (1.9) | 164 (1.3) | 3553 (10.9) |
| May 2020 to December 2020 | 180 (1.1) | 45 (0.4) | 40 (1.1) | 40 (2.3) | 66 (1.7) | 1072 (11.3) |
- Abbreviations: ADP, acute diffuse peritonitis; DG, distal gastrectomy; Eso, esophagectomy; Hep, hepatectomy; LAR, low anterior resection; PD, pancreaticoduodenectomy.
4 DISCUSSION
In the present study, using the data of 228 860 patients who had undergone major gastroenterological surgeries, we demonstrated a marked decline in the number of surgeries performed after the state of emergency declared due to the COVID-19 pandemic, especially in DG, LAR, and Hep. However, the reduction in the number of elective surgeries was not necessarily correlated with the severity of the infections. A similar decline in the number of surgeries performed was seen in the entire country as well as in areas with a high cumulative incidence of infection. Although the infection spread widely in November and December 2020, the number of surgeries performed recovered to the levels seen in the previous 2 y.
On the basis of the changes seen in 2020, there are at least three potential explanations for the drop in the number of surgical cases. First, medical institutions voluntarily restricted elective surgeries to prepare for the pandemic and secure medical supplies in response to a predicted substantial decline in the capacity of medical professionals due to the extra load of patients. Neither the Japan Surgical Society nor the government imposed any restrictions on performing elective surgery, but left the decision to operate to the surgeons who were responsible for their respective patients.4 We consider that the autonomy of the institutes and surgeons contributed to the moderate reduction in and early recovery of the cases thereafter. Nevertheless, a rebound in the number of surgical cases was not observed in 2020, which suggests that there were undiagnosed cancer patients, which is the second potential explanation. The number of undiagnosed patients with gastric cancer, rectal cancer, esophageal cancer, and HCC may be greater than 5000. The detection of cancers through screening significantly decreased after the state of emergency, due to the suspension of screening tests.12 Indeed, the number of surgeries for T1/T2 tumors decreased considerably; these tumors are usually identified through screening tests rather than through consultations for symptoms of the disease. This finding is also supported by a study in a prefecture in Japan, which revealed that the tumors found through screening test decreased.13
Third, there is a possibility that the patients might have chosen “no-further-treatment” or alternative treatment options. In brief, patients who had gastric cancers or colorectal cancers might have opted to not undergo surgical treatment after endoscopic tumor resections despite the fact that the surgeries should be considered additional treatment.14, 15 Patients with HCC could have opted to undergo local ablation therapy rather than surgical resection. Patients with esophageal cancer might have chosen chemoradiation therapy instead of Eso. However, a report from Canada indicating that systemic and radiation treatment decreased during the pandemic16 does not substantiate this theory, and more supporting evidence is required.
In the present study, we demonstrated that patients aged 65–75 y were the most affected by the first wave of COVID-19. No evidence to explain this phenomenon was available: the cause of the phenomenon could be individual factors or the social system. A difference in the cancer screening rates among different age groups was reported in the field of breast cancer in Japan. Women aged 40–49 and 50–69 y showed similar postponement rates for breast cancer screening, whereas women aged 30–39 and 70–79 y had lower rates of postponement of screening procedures.17 The finding was contradictory to our expectation that older individuals would refrain from undergoing cancer screening or attending consultations due to fear of the high mortality rate of COVID-19 in the elderly population.18
Soon after the outbreak of the COVID-19 pandemic, COVIDSurg Collaborative reported that the estimated surgical cancellation rates during the first 12 weeks of the pandemic were 81.7% of operations for benign diseases and 37.7% of cancer operations, 19 and a significant reduction in treatment delivery was subsequently reported from other regions or countries.16, 20 Although we found a decline in the number of surgeries after the state of emergency, the degree of drop was not similar to what can be expected globally. The moderate reduction in the number of surgeries in Japan compared with those in other countries could be partly attributed to the autonomy of the institutes and surgeons, as mentioned above. However, the nonsignificant impact of COVID-19 and recovery at the end of 2020 may have resulted from organized efforts to control the pandemic within Japan. A study from New Zealand showing that surgeries for cardiac diseases did not decrease after successfully suppressing COVID-19 transmission21 supports this hypothesis. In our study, the lower infection prevalence may also protect medical staff and conserve resources and facilities, resulting in low surgical mortalities even after the state of emergency. This speculation will motivate further studies exploring the number of surgeries and mortalities in 2021 and 2022, when infection rates have radically increased in Japan.
4.1 Limitations of the study
Our study had limitations and weaknesses that need to be considered when interpreting the findings. First, we only investigated the number of surgeries performed and the short-term results. The underlying reasons for the reduced number of surgeries were merely speculated upon. To meet this aim, comprehensive research is required, including an analysis of cancer screening, the number of patients who were diagnosed with cancer, and the willingness of the patients to visit the hospital before and after the pandemic.
Second, a natural decrease or increase in the number of surgical cases and the changes in the population were not considered. For instance, surgeries for gastric cancers are decreasing owing to preventive measures such as eradication of the causative organism Helicobacter pylori and the development of endoscopic resection.22 Although a direct comparison cannot be made because the inclusion and exclusion criteria were strictly applied in our study, stomach and duodenal surgeries (for any disease) decreased by 16.5% over 7 y from 2012 to 2019.23 Thus, the rapid reduction early after the state of emergency and the nearly 20% decline in monthly DG cases are attributable to the COVID-19 pandemic. The incidence and causes of newly diagnosed HCCs are also drastically changing24 owing to new treatments for viral hepatitis. A single-institute study has revealed that cancellation (rescheduling) of follow-up for patients with chronic hepatitis C started in March 2020 and reached 49.1% in May 26, 2020.25 Thus, the decline and monthly transition in HCC-related surgeries in 2020 should be the sum of these factors, in addition to selecting alternative treatment options. In contrast, the number of pancreatic cancer surgeries seems to be increasing,23 probably owing to a better understanding, identification, and recognition of pancreatic cystic neoplasms and the expansion of surgical procedures to include the elderly population. Factoring in these trends may further clarify the true impact of COVID-19 on surgical activities in 2020.
Third, the number of T1/T2 tumors, node-negative tumors, and patients in specific age groups decreased in 2020. However, multivariate analysis was not performed to determine which factors were strongly related to the changes in surgical activities. Fourth, a similar trend in the number of surgical cases was observed in areas with high infection rates and in the country as a whole. This does not necessarily indicate that each hospital was affected equally: a questionnaire survey for gastrectomy revealed that selected high-volume centers in Japan were differently affected by COVID-19, with the most significant effects being observed in Tokyo.26
In the present study, we demonstrated that the short-term results were stable as a whole, despite the proportion of older patients and T4 tumors in general. The results show that the quality of surgical treatment for gastroenterological diseases was well maintained during the early phase of the pandemic. However, this study did not reveal how the surgical teams mitigated the effect of the pandemic to avoid adverse results.27 For instance, a Swedish registry-based study suggested that greater use of ostomies and lower participation of residents for colorectal cancer treatment were observed during the COVID-19 pandemic, achieving comparable complication rates despite the increase in T4 tumors.28 This kind of analysis can help clinicians to better cope with cancers during the ongoing and future pandemics at both the administrative and hospital levels. Additionally, the analysis of the mortality rate for each surgery revealed acceptable results in LAR and Eso and adverse results in Hep and PD. Finally, a meta-analysis including gastroenterological cancers demonstrated that a delay in curative treatment for 4 weeks resulted in an increase in the mortality rate by 6%–8%.29 Thus, the long-term ramifications of the COVID-19 pandemic should be investigated by focusing on recurrence rates after surgery, a potential rebound in the decreased number of cases, and the cancer stages after 2020.
4.2 Conclusion
In the present study we demonstrated a decline in the number of surgeries for gastroenterological cancer across Japan soon after the state of emergency was declared during the COVID-19 pandemic. The remarkable decline in T1/T2 tumors is suggestive of the prioritization or loss of the opportunity for cancer screening. The rates of severe complications and mortality were not worsened by COVID-19, even for acute diffuse peritonitis. However, the observed reduction in the cases and lack of rebound deserve further evaluation and public motivation to promote cancer screening.
ACKNOWLEDGMENTS
We would like to express our sincere gratitude and thanks to Dr. Hiroshi Hasegawa (Project Management Subcommittee, The Japanese Society of Gastroenterological Surgery), Dr. Shingo Kanaji (Division of Gastrointestinal Surgery, Department of Surgery, Graduate School of Medicine), Dr. Taizo Hibi (Department of Pediatric Surgery and Transplantation, Graduate School of Medical Sciences, Kumamoto University), Dr. Hiroaki Nagano (Department of Gastroenterological, Breast and Endocrine Surgery, Yamaguchi University Graduate School of Medicine), Dr. Ikeda Norihiko (Department of Surgery, Tokyo Medical University), and Dr. Morito Monden (The Japanese Association of Medical Sciences) for their cooperation in this research.
DISCLOSURE
Author Contributions: Study concepts, design, and data interpretation: all authors. Data acquisition and analysis: Hideki Endo, Hiroyuki Yamamoto, Hiroaki Miyata. Article preparation: all authors. Article review: Akinobu Taketomi, Yoshihiro Kakeji, Yuko Kitagawa, Masaki Mori, Kazuhiro Hanazaki.
Funding Information: This work was supported by the MHLW Special Research Program (Grant Number JPMH20CA2046).
Conflicts of Interest: Hideki Endo, Hiroyuki Yamamoto, and Hiroaki Miyata are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson K.K., and Nipro Co. Yuko Kitagawa received lecture fees from ASAHI KASEI PHARMA CORPORATION, Astra Zeneca K.K., Ethicon Inc., Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Factory, Inc., Olympus Corporation, Nippon Covidien Inc., Shionogi & Co., Ltd., Taiho Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co., Ltd., Bristol-Meyers Squibb K.K., MSD K.K., Smith & Nephew KK, Kaken Pharmaceutical Co., Ltd., Aska Pharmaceutical Co., Ltd., Miyarisan Pharmaceutical Co., Ltd., Toray Industries, Inc., Daiichi Sankyo Company Limited, Chugai Foundation for Innovative Drug, Discovery Science, and Nippon Kayaku Co., Ltd., and grants from Chugai Pharmaceutical Co., Ltd., Taiho Pharmaceutical Co., Ltd., Yakult Honsha Co. Ltd., Asahi Kasei Pharma Corporation, Otsuka Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Tsumura & Co., Kaken Pharmaceutical Co., Ltd., Sumitomo Pharma Co., Ltd., EA Pharma Co., Ltd., Eisai Co., Ltd., Otsuka Pharmaceutical Factory, Inc., Medicon Inc, Kyouwa Kirin Co., Ltd., Takeda Pharmaceutical Co., Ltd., Teijin Pharma Limited, and Nippon Covidien Inc. Yuko Kitagawa disclosed endowed chair supported by Chugai Pharmaceutical Co., Ltd., and Taiho Pharmaceutical Co., Ltd. Yuko Kitagawa is a Chief Editor of Annals of Gastroenterological Surgery. Masaki Mori is Emeritus Editor-in-Chief of Annals of Gastroenterological Surgery. Yasuyuki Seto and Yoshihiro Kakeji are Associate Editors of Annals of Gastroenterological Surgery. Kazuhiro Yoshida and Hiroki Yamaue is Editorial Board Member of Annals of Gastroenterological Surgery. All other authors declare no conflicts of interest relevant to this study.
Ethics Statement: The protocol of this study was reviewed and adopted by the Japanese Society of Gastrointestinal Surgery Committee and approved by the Institutional Review Board of Kochi Medical School with the exemption of individual written informed consent owing to the retrospective study design (ID: 2021-82).