Serum Neurofilament Light Chain Levels Correlate With Skin Inflammation and Scratch Lesions in Patients With Pruritus
Abstract
Background: Neurofilament light chain (NfL) has been identified as a biomarker in neuroaxonal injury. Cutaneous nerve injury resulting from inflammation and/or forced scratching may also potentially affect serum NfL (sNfL) levels.
Objectives: We aimed to explore the relationship between sNfL levels and the severity of skin inflammation and scratch lesions in patients with pruritus.
Methods: In this cross-sectional pilot study, we measured the sNfL levels of 10 patients with pruritus of different aetiologies, and calculated age- and BMI-adjusted sNfL percentiles based on a normative database consisting of 4532 control individuals. Next, we investigated the relationship between the levels of sNfL and the severity of skin inflammation and scratching injuries in these patients using a newly-created Skin Inflammation and Scratch Lesions (SISL) score.
Results: A positive correlation was observed between sNfL levels and the severity of skin inflammation and scratch lesions as measured by the SISL score (Spearman’s rho = 0.70, p = 0.031). When correlated separately, both the “skin inflammation only” and “scratch lesions only” scores correlated positively with sNfL levels (Spearman’s rho = 0.68, p = 0.031; Spearman’s rho = 0.66, p = 0.041, respectively).
Conclusions: sNfL may be a potential biomarker for cutaneous nerve injury associated with skin inflammation and/or scratching.
1. Introduction
Neurofilament light chain (NfL), a cytoskeletal protein, is a promising biomarker specific to neuroaxonal injury in various diseases such as dementia, multiple sclerosis, and peripheral neuropathies [1, 2]. Pruritus (syn. itch) is defined as an unpleasant sensation evoking the urge to scratch [3]. In the skin, itch is mainly transmitted by nonmyelinated C and thinly myelinated Aδ nerve fibers [4], with C-fibers extending into the upper epidermis [5]. Itch signals are transmitted by these fibers to the spinal cord, then via the spinothalamic tract to the thalamus, from where they are distributed to a functional network consisting of itch processing brain structures [6]. Numerous mediators play a role in itch pathophysiology, such as cytokines (e.g., IL-4 and IL-13), neuropeptides and neurotrophins (e.g., substance P and nerve growth factor), hormones (e.g., corticotropin-releasing hormone), opioids (e.g., mu and kappa-opioids), and proteases (e.g., kallikrein and tryptase) [7–9].
To the best of our knowledge, no biomarker indicating cutaneous nerve injury is known so far. A biomarker in this context could be particularly relevant in the setting of chronic pruritus (defined by a duration of ≥ 6 weeks), which is highly prevalent and associated with a substantial individual and economic burden of disease [3]. Such a biomarker could not only help to better objectify the individual course of the disease and anticipate flares, but also help to compare clinical severity and treatment outcome in clinical trials. In the present study, we hypothesized that skin inflammation and/or scratching could result in elevated serum neurofilament light chain (sNfL) levels, potentially serving as a biomarker for cutaneous nerve injury.
2. Materials and Methods
This single-center cross-sectional study was carried out at the Department of Dermatology, University Hospital Basel, Basel, Switzerland. The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants for participation in the study and for publication of descriptions or identifying materials.
The Skin Inflammation and Scratch Lesions (SISL) score was created to assess the (macroscopic) clinical severity of skin inflammation and scratch lesions. This score assesses (a.) the severity on a 0–3 scale for each of the following items: erythema, thickness, lichenification, scaling, dryness, dyspigmentation, erosion/excoriation and (b.) the area of inflamed and/or scratch-injured skin (ranging from 0 to 10, with 1 point representing 10% of body surface area), resulting in a total score of 0–31. We based the SISL score on the frameworks established by the validated the Eczema Area and Severity Index (EASI); the Psoriasis Area Severity Index (PASI), and the SCORing Atopic Dermatitis (SCORAD). The grading breakdown (0–3) of the items in the SISL follows the same criteria as used in these scores.
Levels of sNfL were measured blinded. Blood samples were obtained from all ten participants, and then sNfL levels were measured using single-molecule array (Simoa) NF-light Advantage kit (Quanterix, Billerica, MA, USA) according to manufacturer’s instructions on the single molecule array HD-X platform. Age- and BMI-adjusted sNfL percentiles were then calculated based on a reference database consisting of 4532 control individuals [10]. Patients with comorbidities potentially affecting sNfL levels such as neurodegenerative, cardiovascular, chronic kidney disease, or diabetes were excluded. The correlation between sNfL levels and the severity of skin inflammation and scratch lesions in patients with acute or chronic pruritus was investigated using Spearman’s rank correlation coefficients.
3. Results
Ten patients participated in this study (4 females, 6 males; mean age 53.10 (standard deviation [SD] ± 20.71) years). The demographic and diagnostic information of these participants is presented in Table 1. One patient had acute pruritus, 9/10 chronic pruritus. The mean SISL score of the participants was 14.30 (SD ± 7.26).
| Diagnosis | Age (y) | Sex | SISL score | NfL (pg/mL) | NfL percentile |
|---|---|---|---|---|---|
| Acute urticaria | 35.9 | F | 10 | 8.2 | 83 |
| Atopic dermatitis | 60.7 | M | 24 | 27.6 | 98 |
| Atopic dermatitis | 15.9 | M | 17 | 5.1 | 93 |
| Atopic dermatitis | 49.2 | M | 20 | 8.0 | 53 |
| Atopic dermatitis | 78.7 | M | 16 | 19.2 | 57 |
| Atopic dermatitis | 51.1 | M | 25 | 12.5 | 89 |
| Bullous pemphigoid | 74.3 | F | 14 | 23.6 | 87 |
| Chronic prurigo | 77.9 | M | 9 | 24.0 | 82 |
| Chronic pruritus on primary nondiseased skin | 25.8 | F | 1 | 2.5 | 1 |
| Chronic pruritus on primary nondiseased skin | 61.4 | F | 7 | 10.6 | 44 |
- Abbreviations: NfL, neurofilament light chain; SISL score, skin inflammation and scratch lesions score.
As shown in Figure 1, sNfL levels correlated positively with the severity of skin inflammation and scratch lesions as measured by the SISL score (Spearman’s rho = 0.70, p = 0.031). When correlated separately, both the “skin inflammation only” (SISL score minus the score attributable to scratching) and “scratch lesions only” (body surface area affected by erosions/excoriations) scores correlated positively with sNfL levels (Spearman’s rho = 0.68, p = 0.031; Spearman’s rho = 0.66, p = 0.041, respectively).
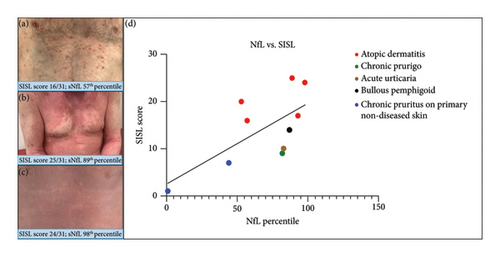
This suggests that both skin inflammation and scratching may contribute independently to the elevated sNfL levels.
In addition, we investigated the correlation between itch intensity and the level of sNfL (data and figure shown in Supporting Information (available here)) but did not find a correlation between either the average or peak 0-10 NRS scores and sNfL levels (Spearman’s r = 0.17, p = 0.70; Spearman’s r = 0.10, p = 0.81, respectively).
4. Discussion
NfL has been proposed as “the neurologist’s troponin” to indicate neuroaxonal injury [11]. Our results suggest that this biomarker may also serve to identify and quantify cutaneous nerve injury from inflammation and/or forced scratching. Interestingly, two other recent studies have reported elevated sNfL levels in patients with psoriasis: Okan et al. [12] found that sNfL levels correlated positively with disease severity as measured by the Psoriasis Area Severity Index (PASI). Nowowiejska et al. [13] did not find a direct correlation between sNfL levels and the PASI values, but observed a statistical trend towards higher levels in patients with moderate and severe psoriasis compared to healthy controls. The authors of both studies hypothesised that the elevated sNfL levels in more severely affected psoriasis patients may reflect central neural inflammation. In a recent MRI study, brain structural changes were reported in patients with atopic dermatitis (AD) [14] which could theoretically be a source of sNFL. We therefore cannot completely rule out this central cause of the increase in sNfL in our AD patients. However, none of our participants had known causes of extracutaneous sources to explain their elevated sNfL, and our data analysis showed a significant correlation between both skin inflammation scores and scratch lesion scores, respectively, with the sNfL levels. In addition, all AD patients had higher SISL scores (presumably reflecting more pronounced cutaneous nerve injury) than the non-AD patients. We therefore assume that the elevated sNfL in our study group is more likely to reflect peripheral neuroaxonal damage.
This study has several limitations, including the small sample size and a cross-sectional design. Additionally, the study lacks ethnic diversity, as both patients and controls were exclusively of Fitzpatrick skin phototype I–III, limiting generalizability of the results to people of color. Larger studies with prospective and ideally longitudinal sNfL measurements, standardized pruritus assessments, and skin biopsies including visualization of axonal nerve damage are needed to confirm our findings.
5. Conclusions
In this pilot study, sNfL correlated positively with the clinical severity of skin inflammation and scratch lesions in patients with pruritus of various aetiologies, suggesting that sNfL may have the potential to serve as a biomarker of cutaneous nerve injury associated with skin inflammation and/or scratching.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
The authors received no financial support for the research and authorship of this article.
Supporting Information
Additional supporting information can be found online in the Supporting Information section.
Open Research
Data Availability Statement
The data are available from the corresponding author upon reasonable request.




