Does Screw Number of Zero-profile Implants in Fusion Segment Influence Intervertebral Stability?
Abstract
Objective
The unclear clinical outcomes of two different zero-profile implants with different number of screws in hybrid surgery restricts the choice of patient-specific implants. This study aims to compare two different implants on its postoperative subsidence, motion stabilization and clinical outcomes. It also provides references to the most reasonable implant choice in fusion surgery.
Methods
This was a retrospective study. From February 2014 to March 2022, 173 patients who underwent hybrid surgery were included. Among them, 122 received surgery with a four screw implant, while 51 received a two screw implant. We analyzed the significance of patient-specific factors, radiographic factors and clinical outcomes. The Wilcoxon rank sum test, t tests/analysis of variance (ANOVA) test and stepwise multivariate logistic regression were adopted for statistical analysis.
Results
No statistically significant difference was observed between the two screw and four screw groups in terms of immediate, middle, and long-term stability and fusion rate (p > 0.05). However, the two screws group had higher FSU height subsidence at 3, 6, and 12 months postoperatively and higher rates of significant subsidence at three and 6 months postoperatively (p < 0.05). Both groups showed significant clinical improvements at the final follow-up.
Conclusion
Two screw and four screw implants provide comparable stability, fusion rates and clinical outcomes. However, the two screw implant was inferior to the four screw implant in subsidence prevention. Therefore, the two-screw implant is non-inferior to the four-screw implant in most patients. It can be used as the priority choice in the fusion segment by its easy manageability. However, the patients with a high risk of subsidence such as multilevel surgery, the elderly, lower BMD, bad cervical alignment should receive a four screw implant rather than a two screw implant.
Introduction
Cervical degenerative disc disease (CDDD) is a major cause of myelopathy and radiculopathy, substantially compromising the patient's quality of life.1 Anterior cervical discectomy and fusion (ACDF) surgery, a gold standard for treating cervical myelopathy and radiculopathy, has conventionally been used to treat CDDD when conservative treatment failed.2 For ACDF, the most crucial aspects are restoring the stability of the surgical segment3 and ensuring stable fixation to promote fusion of the surgical segment.4, 5
The implants used for fusion after discectomy included the traditional anterior cervical cage and titanium plate, zero-profile implants. The zero-profile implant has been employed extensively in fusion surgery in recent years due to its reduced rate of adjacent-level ossification development (ALOD), lower incidence of dysphagia, shorter operation duration, and less blood loss than traditional titanium plate.6-8 Among the zero-profile implant systems, the implant with screws was found to have better immediate stability than the implant with anchor and blade intervertebral fixation methods.9 In the implant with screws (Zero-P), four screws were used to fix the vertebrae. However, in certain conditions, placing a four-screw implant into the narrow space across the disc in the cervical spine was challenging. Moreover, some surgeons favor a construct without hard screw fixation.10 To improve the fusion promotion and simplify the clinical procedure, the modified two-screw implant (Zero-P VA) has been applied in fusion segments.11 Compared to Zero-P, Zero-P VA decreases the number of screws from two screws in the upper and lower vertebrae to one screw in each while increasing the diameter of the screws and the angle of the screws. These changes improve maneuverability and make it easier for the surgeon to place the screws and prostheses in the best position. Nonetheless, the fixation status of two-screw implants versus four-screw implants in patients has not been reported. The influence on the patient's clinical outcomes and fusion rate after fusion surgery was also unclear. Numerous studies have sought to elucidate the risk factors of stability and fusion to improve stability and promote fusion after surgery. Lee et al. reported that the implant's screw length influences the stability and fusion after ACDF, so the screw length divided by the anterior–posterior vertebral body length should be greater than 75%.12 Moreover, Conrad et al. reported that thread pitch substantially impacted the pullout force, but there were no differences between self-tapping and self-drilling screws or screw diameter.13 To better analyze the difference between the two-screw implant and the four-screw implant, hybrid surgery (incorporating ACDF and ACDR at different levels) was chosen as the application scenario for the fusion implant. In our spinal center, we encourage the fusion after ACDF by instructing the patient to wear a neck brace strictly, limiting cervical mobility. In hybrid surgery, patients were required to engage in intermittent activity to ensure the range of motion of the replacement segment post-surgery. The biomechanical environment of the fusion segment to the implant is more severe and will maximize the differences between different implants.
The purposes of the study are: (i) to compare the two different implants with two screws or four screws on its postoperative subsidence, motion stabilization and clinical outcomes; and (ii) to provide references to the most reasonable implants choice in fusion surgery in clinical practice.
Materials and Methods
Study Population
The Institutional Review Board (IRB) approved the current study (Ethics Committee on Biomedical Research, West China Hospital of Sichuan University, No. 2023 [1690]). The informed consent was waived due to the retrospective nature of the research. From February 2014 to March 2022, we consecutively enrolled patients who underwent hybrid surgery for degenerative cervical disease causing radiculopathy or myelopathy. At our institute, all four-screw implants were used for patients who had undergone surgery before May 2020, and two-screw implants were used from May 2020 to the present. The following were the inclusion criteria for the study: (i) a precise radiological diagnosis of cervical myelopathy and/or radiculopathy; (ii) ineffectiveness of conservative treatment for over 6 weeks; (iii) having undergone Hybrid surgery; and (iv) patients aged over 18 years. The following were the exclusion criteria: (i) patients who did not undergo imaging follow-up at our hospital; (ii) prior spine surgery history; (iii) patients with oncologic, traumatic, or infectious pathology; and (iv) patients with incomplete imaging data [Correction added on 22 July 2024, after first online publication: The first exclusion criteria has been amended in this version.].
Surgical Technique
A single surgeon (H. L.) performed these surgeries. The methods were performed under relevant guidelines and regulations. The supine position was assumed after general anesthesia, and the standard right anterior approach was used. The intervertebral disc tissue, cartilage, osteophytes, and other tissue were removed at the surgical level. The intervertebral space and vertebral canal were flushed with normal saline after complete decompression. Gelatin sponge, epinephrine-saline sponge, and fluid gelatin were used to achieve complete hemostasis. For the replacement segment, after the endplates were well prepared, an accurately sized Prestige-LP disc (Medtronic Sofamor Danek, Memphis, TN, USA) was inserted along with channels in the endplates. And in the fusion segment after determination of the appropriate size of the trail spacer, a corresponding Zero-P or Zero-P VA implant (Synthes, Oberdorf, Switzerland) packed with β-tricalcium phosphate or an autograft with excised osteophyte was inserted into the prepared intervertebral space. Next, four or two locking screws were tightened to fix the implant. Then, C-arm fluoroscopy was performed to verify the proper placement of the implants.14 In Zero-P, the screw setting angle is fixed, it is difficult to balance the optimal depth and position of the screws, and after three screws were fixed, the insertion of the remaining fourth screw was difficult and could not achieve the best position and angle. In order to ease the operation and obtain the best insertion depth and angle, the two-screws implant with variable angle screws was applied to ACDF. The patients who underwent the surgery with two-screw implants were included in the two screw group, the patients who underwent the surgery with four-screw implants were included in the four screw group.
Data Collection
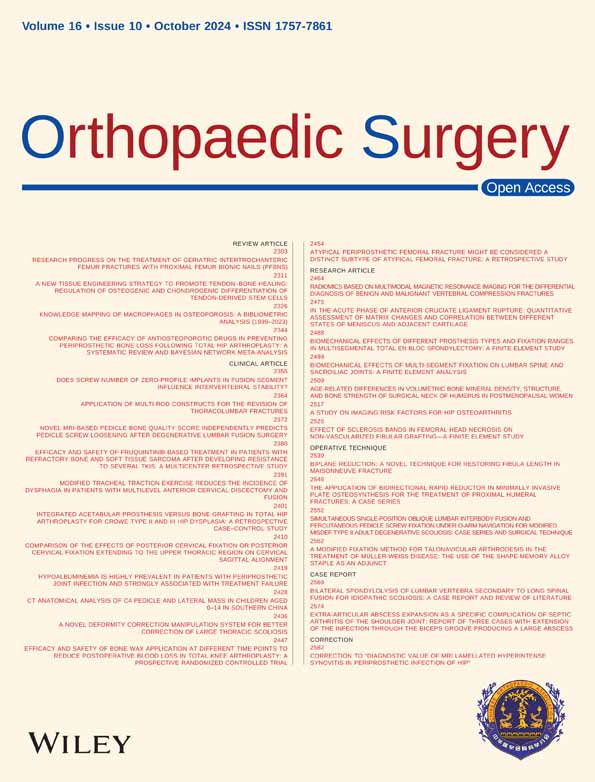
The union was evaluated by the presence of continuous bone bridges behind the fusion segments on CT three-dimensional reconstruction. The radiographs were recorded at preoperative, postoperative, 3-month, 6-month, 1-year, and last follow-up. These radiographs included functional spine unit (FSU), Cobb angle, FSU range of motion (ROM), disc ROM and FSU height at anterior, middle and posterior to analyze the subsidence of the prosthesis. Moreover, we not only compared the absolute value of subsidence, the subsidence of > 2 mm demonstrated in at least one of the upper or lower endplate-allograft interface was defined as significant subsidence, but also compared the significant subsidence rate.15 The clinical evaluation was performed in a blinded fashion by three spine surgeons (Z.P., Y.M., and Y. X.D.) who were absent in the surgical procedures. The radiological evaluation was performed by two independent spine surgeons (X.S. and X.P.), and the mean values were used for statistical analysis, when disputes arose, all researchers discussed them and reached a conclusion. A schematic diagram of the parameters is shown in Figure 1.
Clinical outcomes were acquired at preoperative and last follow-ups. These included Japanese Orthopaedic Association (JOA) scores and visual analogue scale (VAS) scores for neck and arm pain. The Hirabayashi method measured the JOA Recovery rate: (postoperative score − preoperative score) × 100/ (17 − preoperative score).
Statistical Analysis
For non-normally distributed continuous variables such as weight, the Wilcoxon rank sum test was used (presented as Median (25th percentile, 75th percentile)). For continuous variables such as age, height, body mass index (BMI), bone mineral density (BMD), Cobb angle, ROM, FUS height, and clinical outcomes, the t-tests/analysis of variance (ANOVA) was used (presented as mean ± SD). The chi-square and Fisher's exact test were used for the categorical data. The p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS, version 18.0 (SPSS Inc. Chicago, IL, USA) software.
Results
Demographic Data
Out of the 221 patients evaluated, 173 met the inclusion criteria and were included in this study. The four screw group had 122 patients, while the two screw group had 51 in post-operative. All patients underwent hybrid surgery with one level ACDF and one level ACDR. There were no statistically significant differences in age, gender, BMI, BMD, or operative level(s) between the two groups. There were 134 patients (Four screws/Two screws 94/40) in 3 months follow-up, 63 patients (Four screws/Two screws 41/22) in 6 months follow-up and 51 patients (Four screws/Two screws 41/10) in 1 year follow-up had imaging taken in our hospital. Table 1 shows the patient characteristics [Correction added on 22 July 2024, after first online publication: Preceding paragraph has been corrected in this version.].
| Characteristic | Four screws | Two screws | χ2 /t | p value |
|---|---|---|---|---|
| Number of cases | 122 | 51 | ||
| Age (years) | 46.74 ± 6.84 | 46.75 ± 7.37 | 0.003 | 0.997 |
| Gender | 0.018 | 0.892 | ||
| Male | 54 | 22 | ||
| Female | 68 | 29 | ||
| Operative level | 4.609 | 0.203 | ||
| C3/4 | 5 | 1 | ||
| C4/5 | 12 | 11 | ||
| C5/6 | 88 | 33 | ||
| C6/7 | 17 | 6 | ||
| BMD (SPINE, T value) | 0.485 ± 1.135 | 0.391 ± 1.400 | 0.444 | 0.658 |
| BMD (HIP, T value) | 0.075 ± 1.045 | −0.043 ± 0.997 | 0.661 | 0.509 |
| High (cm) | 160.71 ± 8.11 | 163.29 ± 7.72 | 1.935 | 0.055 |
| Weight (kg) | 61.11 (53.00, 70.00) | 62.50 (55.80, 70.80) | 0.857 | 0.392 |
| BMI (kg/m2) | 23.96 ± 2.97 | 23.82 ± 2.84 | 0.285 | 0.776 |
Stability of Two Implants
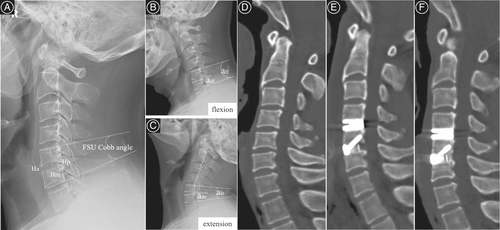
Measuring the implant's stability, the range of motion of FSU and disc were compared (Table 2, Figure 2). In pre-operation, there were no significant differences between the two groups in FSU ROM (p = 0.981) and Disc ROM (p = 0.380). The immediate stability of two implants, including FSU ROM (p = 0.695), △FSU ROM (p = 0.870), disc ROM (p = 0.4540), and △disc ROM (p = 0.852), also did not differ significantly in post-operation. Regarding medium and long-term stability, there were no significant differences at 3 months follow-up (four screws vs two screws: FSU ROM (P = 0.309), △FSU ROM (P = 0.832), disc ROM (P = 0.124) and △disc ROM (P = 0.148)), 6 months' follow-up (four screws vs two screws: FSU ROM (p = 0.527), △FSU ROM (p = 0.614), disc ROM (p = 0. 394) and △disc ROM (p = 0. 459)) and 1-year follow-up (four screws vs two screws: FSU ROM (p = 0.615), △FSU ROM (p = 0.756), disc ROM (p = 0.087) and △disc ROM (p = 0.492)).
| Characteristic | Four screws | Two screws | t/x2/z | p value |
|---|---|---|---|---|
| FSU Cobb angle (°) | 4.95 ± 3.89 | 4.77 ± 4.07 | 0.275 | 0.786 |
| △ FSU Cobb anglea (°) | −0.30 ± 5.00 | 0.74 ± 5.09 | 1.244 | 0.215 |
| △ FSU Cobb angleb (°) | −1.35 ± 4.24 | −1.31 ± 4.35 | 0.049 | 0.961 |
| △ FSU Cobb anglec (°) | −1.11 ± 4.30 | −0.50 ± 4.04 | 0.546 | 0.587 |
| △ FSU Cobb angled (°) | −0.81 ± 3.68 | −0.16 ± 3.36 | 0.524 | 0.603 |
| FSU ROM (°) | 10.02 ± 4.49 | 10.04 ± 4.44 | 0.024 | 0.981 |
| FSU ROMa (°) | 2.91 ± 2.40 | 2.75 ± 2.47 | 0.392 | 0.695 |
| FSU ROMb (°) | 3.70 ± 3.35 | 3.11 ± 2.28 | 1.022 | 0.309 |
| FSU ROMc (°) | 2.99 ± 2.50 | 2.59 ± 2.01 | 0.636 | 0.527 |
| FSU ROMd (°) | 3.23 ± 2.57 | 2.78 ± 2.21 | 0.506 | 0.615 |
| △FSU ROMa (°) | −7.33 ± 4.33 | −7.15 ± 4.20 | 0.164 | 0.870 |
| △FSU ROMb (°) | −6.67 ± 5.41 | −6.47 ± 5.41 | 0.212 | 0.832 |
| △FSU ROMc (°) | −8.01 ± 5.25 | −7.33 ± 4.27 | 0.506 | 0.614 |
| △FSU ROMd (°) | −6.98 ± 4.91 | −6.45 ± 4.49 | 0.313 | 0.756 |
| disc ROM (°) | 8.07 ± 3.77 | 8.63 ± 4.05 | 0.880 | 0.380 |
| disc ROMa (°) | 2.50 ± 1.83 | 2.73 ± 1.85 | 0.751 | 0.454 |
| disc ROMb (°) | 3.39 ± 2.73 | 2.66 ± 1.81 | 1.548 | 0.124 |
| disc ROMc (°) | 2.73 ± 2.08 | 3.25 ± 2.28 | 0.858 | 0.394 |
| disc ROMd (°) | 2.87 ± 2.10 | 1.21 ± 0.82 | 1.751 | 0.087 |
| △disc ROMa (°) | −5.79 ± 3.58 | −5.91 ± 4.15 | 0.186 | 0.852 |
| △disc ROMb (°) | −4.79 ± 4.56 | −6.00 ± 3.80 | 1.455 | 0.148 |
| △disc ROMc (°) | −5.75 ± 5.32 | −4.70 ± 3.89 | 0.746 | 0.459 |
| △disc ROMd (°) | −5.59 ± 4.76 | −7.15 ± 4.24 | 0.694 | 0.492 |
- a Post-operative, △: The improvement between pre-operative and post-operative.
- b 3-month follow-up, △: The improvement between pre-operative and 3-month follow-up.
- c 6-month follow-up, △: The improvement between pre-operative and 6-month follow-up.
- d 1 year follow-up, △: The improvement between pre-operative and 1 year follow-up.

Subsidence of Two Implants
In subsidence comparison (Table 3, Figure 3), the FSU height did not differ significantly between the two groups in pre-operation and post-operation showing comparable baseline between the two groups. There was a significant difference in △FSU height among anterior, middle and posterior at the 3 month, 6 month and 1-year follow-ups indicating that the four screw group has lesser FSU height subsidence than the two screw group [Correction added on 22 July 2024, after first online publication: FUS has been corrected to FSU in this version.].
| Characteristic | Four screws | Two screws | t/x2/z | p value |
|---|---|---|---|---|
| Pre-operation | ||||
| FSU height (anterior) (cm) | 3.35 ± 0.30 | 3.43 ± 0.29 | 1.578 | 0.116 |
| FSU height (middle) (cm) | 3.15 ± 0.30 | 3.22 ± 0.28 | 1.503 | 0.135 |
| FSU height (Posterior) (cm) | 3.43 ± 0.29 | 3.49 ± 0.30 | 1.195 | 0.234 |
| Post-operation | ||||
| FSU height (anterior) (cm) | 3.65 ± 0.34 | 3.69 ± 0.30 | 0.802 | 0.424 |
| FSU height (middle) (cm) | 3.45 ± 0.31 | 3.50 ± 0.28 | 1.012 | 0.313 |
| FSU height (posterior) (cm) | 3.60 ± 0.29 | 3.63 ± 0.31 | 0.503 | 0.615 |
| 3 months follow-up | ||||
| △FSU height (anterior) (cm) | −0.03 ± 0.17 | −0.20 ± 0.17 | 5.435 | 0.000 |
| △FSU height (middle) (cm) | 0.001 ± 0.14 | −0.16 ± 0.16 | 5.600 | 0.000 |
| △FSU height (posterior) (cm) | −0.001 ± 0.14 | −0.12 ± 0.19 | 4.088 | 0.000 |
| 6 months follow-up | ||||
| △FSU height (anterior) (cm) | −0.04 ± 0.19 | −0.25 ± 0.21 | 3.929 | 0.000 |
| △FSU height (middle) (cm) | −0.001 ± 0.15 | −0.14 ± 0.18 | 3.329 | 0.001 |
| △FSU height (posterior) (cm) | 0.012 ± 0.15 | −0.16 ± 0.18 | 4.092 | 0.000 |
| 1 year follow-up | ||||
| △FSU height (anterior) (cm) | −0.08 ± 0.18 | −0.28 ± 0.22 | 3.044 | 0.004 |
| △FSU height (middle) (cm) | −0.005 ± 0.15 | −0.16 ± 0.15 | 2.965 | 0.005 |
| △FSU height (posterior) (cm) | 0.02 ± 0.15 | −0.14 ± 0.10 | 3.164 | 0.003 |
- Note: △: The improvement between post-operative and 3 months follow-up or 6 months follow-up or 1-year follow-up.
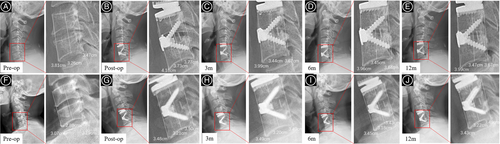
Considering the significant subsidence (Table 4), the rate of significant subsidence did differ significantly between the four screw group and two screw group among anterior, middle, and posterior at the 3-month follow-up. However, at the 1-year follow-up, there were no significant differences between the two groups.
| Characteristic | Four screws | Two screws | t/x2/z | p value |
|---|---|---|---|---|
| 3 months follow-up | ||||
| Number of patients (anterior) | 13 (13.83%) | 15 (37.5%) | 9.511 | 0.002 |
| Number of patients (middle) | 9 (9.57%) | 14 (35%) | 12.758 | 0.000 |
| Number of patients (posterior) | 9 (9.57%) | 9 (22.5%) | 4.031 | 0.045 |
| 6 months follow-up | ||||
| Number of patients (anterior) | 8 (19.51%) | 12 (54.55%) | 8.110 | 0.004 |
| Number of patients (middle) | 3 (7.32%) | 7 (31.82%) | 6.436 | 0.011 |
| Number of patients (posterior) | 3 (7.32%) | 10 (45.45%) | 12.716 | 0.001 |
| 1 year follow-up | ||||
| Number of patients (anterior) | 11 (26.83%) | 5 (50.00%) | 2.0055 | 0.253 |
| Number of patients (middle) | 4 (9.76%) | 3 (30.00%) | 2.782 | 0.126 |
| Number of patients (posterior) | 3 (7.32%) | 2 (20.00%) | 1.462 | 0.250 |
- Note: △: The improvement between post-operative and 3 months follow-up or 6 months follow-up or 1-year follow-up. [Correction added on 22 July 2024, after first online publication: Table 4 has been corrected in this version.]
Fusion Rate of Two Implants
To evaluate the influence of four screws and two screws on the fusion, we observed the presence of continuous bone bridges behind the surgical segments in fusion on the CT scan (Table 5). It was revealed that there was no significant difference in fusion rate between the two groups at 3 months' follow-up (p = 0.189), 6 months' follow-up (p = 0.229), and 1-year follow-up (p = 0.818). The percentage of the bone bridge behind the operative segment was also compared, and no significant difference was observed between the four screw and two screw groups at 3 months follow-up (p = 0.450), 6 months follow-up (p = 0.793), and 1-year follow-up (p = 0.871).
| Characteristic | Four screws | Two screws | t/x2/z | p value |
|---|---|---|---|---|
| Percentage of bone bridge (3 month) (%) | 75.17 ± 33.93 | 58.56 ± 27.90 | 1.341 | 0.189 |
| Percentage of bone bridge (6 month) (%) | 78.67 ± 37.13 | 63.64 ± 29.24 | 1.224 | 0.229 |
| Percentage of bone bridge (1 year) (%) | 95.00 ± 22.07 | 93.52 ± 23.67 | 0.231 | 0.818 |
| Fusion rate (3 month) (Yes/No) | 28/84 | 10/41 | 0.570 | 0.450 |
| Fusion rate (6 month) (Yes/No) | 66/36 | 30/18 | 0.069 | 0.793 |
| Fusion rate (1 year) (Yes/No) | 74/4 | 32/2 | 0.027 | 0.871 |
- Note: If a patient achieves fusion at the 3-month follow-up, they are presumed to have achieved fusion at the 6-month and 12-month follow-up, and similarly if they achieve fusion at the 6-month follow up, they are presumed to have achieved fusion at the 12-month follow-up. [Correction added on 22 July 2024, after first online publication: Table 5 has been corrected in this version.].
Clinical Outcomes
There were no significant differences in JOA recovery rate (p = 0.355), △VAS arm-pain (left) (p = 0.912), △VAS arm-pain (right) (p = 0.783) scores, and △VAS neck-pain (p = 0.192) between the final follow-up and preoperative in the four screw and two screw groups (Table 6). There was no significant difference in the incidence of complications between the two groups excepting the prosthesis subsidence (18.85% vs 17.64%, p > 0.05), including the incidence of the upper limb, neck, dysphagia, hematoma, delayed wound healing and new foraminal stenosis (supplements).
| Characteristic | Four screws | Two screws | t/x2 | P value |
|---|---|---|---|---|
| JOA recovery rate (%) | 86.67 ± 21.94 | 75.56 ± 25.30 | 0.990 | 0.355 |
| △VAS arm-pain (left) | −1.55 ± 0.59 | −1.42 ± 0.54 | 0.112 | 0.912 |
| △VAS arm-pain (Right) | −1.54 ± 0.45 | −1.37 ± 0.41 | 0.278 | 0.783 |
| △VAS neck-pain | −3.09 ± 2.30 | −1.72 ± 2.26 | 1.339 | 0.192 |
Discussion
The current study suggests that both two-screws and four screws groups offer similar stability and effects in promoting fusion and improving neural function. However, the two-screws implant exhibited more subsidence than the four-screws implant. For clinical work, our findings suggest that the two-screw implant is non-inferior to the four-screw implant in most patients. However, in patients with a high risk of subsidence such as multilevel surgery, the elderly, lower BMD, bad cervical alignment, a four-screw implant is a better choice.
Stability of Two Implants
In the fusion segments of hybrid surgery, obtaining stability immediately to promote fusion and maintain normal cervical spine biomechanics is crucial. Unlike the common belief that more screws have better stability, between the two-screw implant and four-screw implant, there were no significant differences in immediate, medium-term, and long-term follow-up stability. Both implants can provide sufficient stability that were able to maintain a postoperative range of motion including FSU ROM and disc ROM of about 3°. In immediate stability, although two fewer screws are used in the fixation of the zero-profile in the two screw group, the screws' length is also longer than the four-screw implant. Lee et al. showed that shorter screw lengths increased the pseudarthrosis risk and lowered stability after fusion.16 Considering medium-term and long-term stability, it is mainly provided by bone fusion. This was consistent with the fusion results, including fusion rate and percentage of the bone bridge of the two groups in 3-month, 6-month, and 1-year follow-ups. We also performed a subgroup analysis based on the preoperative ROM of the fusion segment to investigate the application scenarios of two-screws and four-screws implants. It showed that among the > 11° group (means instability in this segment), 3–11° group (means normal position), and <3° group (means severe degeneration and there was almost no motion),3, 17 the immediate, middle- and long-term stability had no significant improvements across all follow-up periods (supplements).
Subsidence of Two Implants
Regarding the subsidence of the two implants, the two-screw group had more serious subsidence and higher significant subsidence rate than the four screw group. Many studies have reported that multilevel surgery, the elderly, lower BMD, bad cervical alignment, excessive vertebral endplate resection, and lower screw tip to vertebral body height ratio easily lead to subsidence.12, 18 In our study, there were no significant differences in age, BMD, and FSU Cobb angle between the two screw group and the four screw group. The finite element studies of Jin et al. and Shen et al.13, 19 showed higher Von Mises stress on the surface of the interbody implant's and anterior endplate's surface than titanium plate and PEEK cage. Moreover, the higher stress was more concentrated on the screws and anterior endplate in the two screw zero-profile implant than in a four-screw implant. The higher stress on the anterior endplate also causes a higher subsidence rate in two screw implants.18, 20 Furthermore, in the two screws implant, the screw and the fixed plate are designed to have a small angle to micro-motion rather than being completely locked, as in the four-screws implant. Although Ledet et al. demonstrated that micro-motion stimulates bone formation in the ACDF segment,21 the micro-motion also causes implant subsidence before fusion.22 Furthermore, in the subgroup analysis based on the preoperative ROM of the fusion segment, the fusion segment subsidence is consistent with the prior research; the two-screw implant had more severe subsidence than the four-screw implant(supplements).
Clinical Outcomes and Fusion Rate
There was no significant difference in the clinical outcomes and fusion rate measures between the two groups. The improvement of clinical outcomes mainly determined by the thoroughness of decompression, degree of preoperative compression, and severity or duration of symptoms. Although there was higher subsidence rate in two-screw implants, both the two-screw implant group and four-screw implant group underwent complete neurological decompression and both implants can provide sufficient stability until bone fusion.
Strengths and Limitations
The study had some limitations: first, this is a retrospective, single-center comparison of two implants with a potentially small sample size. Second, the two implants were applied at different times and were not used simultaneously at the clinic despite being performed by the same surgeon. Consequently, a larger sample size and longer follow-up, prospective, and multicenter studies are necessary. Despite having certain restrictions, this study is the first to focus on the outcomes of applying two-screw and four-screw implants in hybrid surgery. The results also provide possible directions for implant choosing in clinical works.
Prospects of Clinical Application
For anterior cervical fusion discectomy implant selection, the two-screw implant is non-inferior to the four-screw implant in most patients and is ease of operation, it can be used as the priority choice in the fusion segment. However, in patients with a high risk of subsidence such as multilevel surgery, the elderly, lower BMD, bad cervical alignment, a four-screw implant is a better choice.
Conclusion
In conclusion, our research indicates that the two-screw and four screw groups offer similar stability and effects in promoting fusion and improving neural function. However, the two-screw implant exhibited more subsidence height than the four-screw implant. For clinical works, the two-screw implant is non-inferior to the four-screw implant in most patients. And because of the two-screw implant's ease of operation, it can be used as the priority choice in the fusion segment. However, in patients with a high risk of subsidence such as multilevel surgery, the elderly, lower BMD, bad cervical alignment, a four-screw implant is a better choice.
Authors Contributions
YM and HL contributed to the study design and supervision. ZP, YD, YH, CD, BW, XP, and YM contributed to study design, data extraction and statistical, and manuscript draft, XS, YL contributed to data extraction and response to reviewers. All authors contributed to the review and revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
This study was supported by West China Hospital, Sichuan University(ZYJC21070), Sichuan Province Science and Technology Support Program of China (2022YFS0101, 22ZDYF1077 to Y Meng), 1·3·5 project for disciplines of excellence, Provincial Science and Technology Plan Project Special Fund Transfer Payment Project(2021-YF08-00113-GX). Department of Science and Technology of Sichuan Province (2019YFQ0002) and West China Nursing Discipline Development Special Fund Project, Sichuan University (HXHL20050).
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Ethics Statement
This study was granted the approval by Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (Date: 9/20/2023/Agenda 1690).
Open Research
Data Availability Statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.