Hospitalisations With Cryoglobulin-Related Diseases in Spain Over 25 Years
Funding: The authors received no specific funding for this work.
Handling Editor: Luca Valenti
ABSTRACT
Background
The epidemiology of cryoglobulinemia in Spain has likely changed following the widespread adoption of direct-acting antivirals (DAAs) since 2015 for the treatment of hepatitis C virus (HCV) infection, the principal cause of mixed cryoglobulinemia (MC).
Methods
All hospital admissions of patients with cryoglobulinemic disease at the National Registry of Hospital Discharges were retrospectively examined in Spain from 1997 to 2022. The following primary conditions associated with cryoglobulinemia were considered: chronic viral infections, haematological diseases (HD), and autoimmune diseases (AD).
Results
A total of 16 929 admissions for patients with cryoglobulinemic disease were recorded during the study period. Hospitalisation rates for patients with cryoglobulinemia steadily increased from 1997 to 2015 (from 10.8 to 17.9 admissions per 1 million habitants, APC = +2.1), and decreased from 2018 to 2022 (from 15.7 to 11 admissions per 1 million habitants, APC = −7) (p < 0.001 for all). The drastic changes in HCV prevalence rates determined this shift (26.3% in 1997, 52.7% in 2016 and 27.9% in 2022, p < 0.001). The proportion of patients with cryoglobulinemia associated with hepatitis B virus (HBV), paraproteinemias, non-Hodgkin lymphoma, systemic lupus erythematosus, primary Sjögren syndrome and rheumatoid arthritis steadily increased during the study period as cause of hospitalisation in patients with cryoglobulinemia (from 1997 to 2022, p < 0.001), while human immunodeficiency virus infection remained fairly stable since 2005.
Conclusions
The introduction of DAA as treatment for HCV has resulted in a significant reduction in hospitalisations due to cryoglobulinemia in Spain. As a result, cases due to HBV, hematologic and autoimmune diseases have emerged as conditions of growing importance associated with cryoglobulinemia hospitalisations.
Summary
- We analysed 25 years of hospital admissions in Spain related to cryoglobulinemia, a rare condition caused by abnormal proteins in the blood.
- Thanks to new hepatitis C treatments, virus-related cases have decreased, while autoimmune and blood-related diseases have become the main causes.
- Our study shows how the profile of affected patients has changed and highlights the need for ongoing attention to this evolving disease.
Abbreviations
-
- AD
-
- autoimmune diseases
-
- B-NHL
-
- B lineage non-Hodgkin lymphoma
-
- CLL
-
- chronic lymphocytic leukaemia
-
- HCV
-
- hepatitis C virus
-
- HBV
-
- hepatitis B virus
-
- HD
-
- haematological diseases
-
- HIV
-
- human immunodeficiency virus
-
- IMMI
-
- idiopathic inflammatory myopathy
-
- MCTD
-
- mixed connective tissue disease
-
- MGUS/MGCS
-
- monoclonal gammopathy of undetermined significance/monoclonal gammopathy of clinical significance
-
- MM
-
- multiple myeloma
-
- NHL
-
- non-Hodgkin lymphoma
-
- RA
-
- rheumatoid arthritis
-
- SjS
-
- Sjögren's syndrome
-
- SLE
-
- systemic lupus erythematosus
-
- SNHDD
-
- Spanish National Hospital Discharge Database
-
- SSc
-
- systemic sclerosis
-
- WM
-
- Waldenström's macroglobulinaemia
1 Introduction
Cryoglobulinemia is a rare condition in which abnormal immunoglobulins, known as cryoglobulins, are present in the blood and precipitate when exposed to temperatures below 37°C, dissolving again when the temperature rises [1]. According to Brouet's classification, the disease can be divided into three subtypes. Type I is characterised by the presence of monoclonal immunoglobulins. Type II includes a combination of monoclonal IgM with rheumatoid factor activity and polyclonal IgG. Finally, type III consists of both polyclonal IgM with rheumatoid factor activity and polyclonal IgG [2]. Type II and III, referred to as mixed cryoglobulinemia (MC), are associated with hepatitis C virus (HCV) and other viral infections, autoimmune diseases (AD) and lymphoproliferative diseases. In contrast, Type I is exclusively linked to B-cell proliferative disorders [3]. In the absence of an underlying condition, cryoglobulinemia is classified as essential. As research into the essential form of cryoglobulinemia progresses, the number of cases that fall into this category is declining [1].
In mixed cryoglobulinemia, the presence of cryoglobulins can lead to an immunocomplex-mediated systemic small-to-medium vessel vasculitis, known as cryoglobulinemic vasculitis [3, 4]. In contrast, type I cryoglobulinemia mainly causes hyperviscosity syndrome and small vessel thrombosis, leading to Raynaud's phenomenon, purpura and livedo reticularis. Therefore, the potentially life-threatening vasculitic and cryoglobulinemic clinical manifestations may vary depending on the type of cryoglobulins and the baseline condition. Accordingly, different clinical manifestations of damage to the skin, glomerulus, joints and/or the peripheral nervous system can be seen in types I, II and III cryoglobulinemia [5].
Classically, chronic HCV infection was responsible for 70%–90% of MC cases [6]. In the mid-2010s, the advent of direct-acting antivirals (DAA) was a major breakthrough, as more than 95% of chronic hepatitis C patients cleared the virus following a course of 2–3 months of therapy [7]. As a result, the epidemiological landscape of MC was transformed. The widespread use of DAA in Western countries has substantially reduced the rate of HCV-related MC [8]. As a compensation, haematological diseases (HD), including paraproteinemias and lymphoproliferative disorders, as well as AD, mainly Sjögren's syndrome (SjS) and systemic lupus erythematosus (SLE), have emerged as major causes of cryoglobulinemia during the last decade [8, 9]. Alongside this replacement, the demographics, clinical profile, natural history and outcome of MC have experienced important changes [1].
Since 2015, the public Spanish Health System has provided free-of-charge DAA therapy to all patients with hepatitis C with advanced liver fibrosis, extrahepatic manifestations, including cryoglobulinemia and women of childbearing age [10]. This coverage was expanded in 2017 to include all individuals infected with HCV infection [10]. Using the national hospital admission database spanning 25 years, we investigated all hospital admissions with cryoglobulinemia in Spain. Our study focused on epidemiological trends, including hospitalisation rates, prevalence and mortality, with particular attention to changes in underlying etiologies and the impact of DAA on HCV treatment.
2 Methods
We conducted a descriptive analysis to assess the epidemiology and temporal trends of cryoglobulinemia and associated conditions among patients hospitalised in Spain from 1997 to 2022. We used data from the Spanish National Hospital Discharge Database (SNHDD), a publicly accessible registry maintained by the Spanish Government. The SNHDD provides comprehensive demographic and epidemiological data, including up to 20 hospital discharge diagnoses per admission, coded according to the International Classification of Diseases (ICD-9 from 1997 to 2015 and ICD-10 from 2016 onwards). Previous studies have validated the robustness, reliability and high value of the SNHDD in estimating the burden and temporal trends of distinct clinical conditions at the national level [11-14]. For reference, data on the population living in Spain during the same period were obtained from the National Statistics Institute (INE) (www.ine.es).
2.1 Study Population and Definition
We identified all hospital admissions of patients with cryoglobulinemic disease from 1997 to 2022, using ICD-9 code 273.2 and ICD-10 code D89.1. Besides collecting epidemiological data, including sex, age, mortality and length of hospital stay, we used ICD codes to identify primary conditions associated with cryoglobulinemic disease, including chronic viral infections, HD or AD. Chronic viral infections considered were HCV, human immunodeficiency virus (HIV) and hepatitis B virus (HBV). HD comprised paraproteinemias, including monoclonal gammopathy of undetermined significance (MGUS), monoclonal gammopathy of clinical significance (MGCS), multiple myeloma (MM) and Waldenström's macroglobulinaemia (WM), as well as chronic lymphocytic leukaemia (CLL) and non-Hodgkin lymphoma (NHL). For AD, we retrieved the following: SLE, primary SjS, rheumatoid arthritis (RA), systemic sclerosis (SSc), mixed connective tissue disease (MCTD) and idiopathic inflammatory myopathies (IMMI). Essential cryoglobulinemia was defined by the absence of these conditions in the diagnostic record.
2.2 Statistical Analyses
For the descriptive analysis, categorical variables were reported as frequencies and percentages, while numerical variables were presented as means and standard deviations. The significance of differences between groups was determined using Pearson's chi-square or Student's t-tests, as appropriate. A binary logistic regression analysis was conducted to identify factors associated with mortality, adjusting for age, sex, comorbidities associated with cryoglobulinemia and the year of admission. All descriptive and multivariate analyses were performed using SPSS version 26.0.
Annual trend analyses were conducted to assess changes in the number of hospitalisations due to cryoglobulinemia over the study period, including mortality and mean age. Admission rates were calculated per 1 million inhabitants per year based on the whole Spanish population. In a secondary analysis, trends for each condition associated with cryoglobulinemia were analysed. The rate of each condition was reported as a percentage of the total number of patients diagnosed with cryoglobulinemia each year, with trends analysed using the annual per cent change (APC) from baseline. Annual trend analyses were conducted using Joinpoint Regression Program version 5.2.0.
Statistical significance was set at a p-values < 0.05.
2.3 Ethics
The study complies with the Declaration of Helsinki and received approval from the Ethics Committee of Puerta de Hierro University Hospital (PI 241-24). All data from records were provided in an anonymised form, with any potential patient identifiers removed. In accordance with Spanish law, informed consent was not required for this study.
3 Results
3.1 Study Population
Between 1997 and 2022, a total of 16 929 admissions of patients with cryoglobulinemia were recorded. As shown in Table 1, 53.1% were female, and the mean age was 63.6 years. Associated conditions were as follows: chronic viral infections in 42.8%, including HCV in 39.3%, HIV in 8%, and HBV in 1.9%. HC were identified in 6.2% of cryoglobulinemia admissions, as follows: paraproteinemia 5.6%, CLL 0.7%, and NHL 3.9%. The presence of AD was found in 9.7%, SLE in 2.2%, primary SjS in 4.3%, RA in 2%, and SSc in 1%, among others. The remaining 43.6% of admissions were classified as essential cryoglobulinemia.
| Total (n) | 16 929 |
| Female (n, %) | 8992 (53.1) |
| Age (years) (mean, SD) | 63.6 (15.1) |
| Associated conditions | |
| Viral infection (n, %) | 7244 (42.8) |
| HCV | 6655 (39.3) |
| HIV | 1355 (8) |
| HBV | 326 (1.9) |
| Age (years) (mean, SD) | 59.9 (14.5) |
| Haematological condition (n, %) | 1043 (6.2) |
| Paraproteinemia | 942 (5.6) |
| MGUS/MGCS | 584 (3.4) |
| MM | 219 (1.3) |
| WM | 162 (1) |
| CLL | 122 (0.7) |
| NHL | 658 (3.9) |
| Age (years) (mean, SD) | 67.6 (12.6) |
| Autoimmune disease (n, %) | 1641 (9.7) |
| SLE | 371 (2.2) |
| Primary SjS | 727 (4.3) |
| RA | 347 (2) |
| SSc | 162 (1) |
| MCTD | 36 (0.2) |
| IIM | 31 (0.2) |
| Age (years) (mean, SD) | 63.7 (15) |
| Essential cryoglobulinemia (n, %) | 7376 (43.6) |
| Age (years) (mean, SD) | 66.4 (15.2) |
| Outcomes | |
| Admission length stay (days) (mean, SD) | 12.7 (15.4) |
| Mortality (n, %) | 1156 (6.8) |
- Abbreviations: CLL, chronic lymphocytic leukaemia; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IIM, idiopathic inflammatory myopathy; MCTD, mixed connective tissue disease; MGUS/MGCS, monoclonal gammopathy of undetermined significance/monoclonal gammopathy of clinical significance; MM, multiple myeloma; NHL, non-Hodgkin lymphoma; RA, rheumatoid arthritis; SD, standard deviation; SjS, Sjögren's syndrome; SLE, systemic lupus erythematosus; SSc, systemic sclerosis; WM, Waldenström's macroglobulinaemia.
Notably, patients with virus-associated cryoglobulinemia (mean age 59.9 years), including those with HCV infection (mean age 60.8 years), were younger than patients with HD (mean age 67.7 years), AD (mean age 63.7 years) and essential cryoglobulinemia (mean age 66.4 years) (p < 0.001).
Overall, in-hospital mortality in patients admitted with cryoglobulinemia was 6.8%. After adjustment, older age (OR = 1.04, 95% CI: 1.03–1.04), NHL (OR = 1.74, 95% CI: 1.34–2.25) and HIV infection (OR = 1.69, 95% CI: 1.30–2.20) were independently associated with an increased risk of mortality. Conversely, primary SjS (OR = 0.52, 95% CI: 0.34–0.76) and more recent years of admission (OR = 0.98 per year, 95% CI: 0.97–0.99) displayed a protective effect.
3.2 Hospitalisation Trends for Cryoglobulinemia
The number of hospital admissions with cryoglobulinemia steadily increased in Spain from 1997 to 2015, from 10.8 to 17.9 admissions per 1 million habitants (APC = +2.1; p < 0.001). Figure 1 illustrates that, after peaking in 2015–2018, there was a dramatic decline in the rate of admissions with cryoglobulinemia up to 2022 (from 15.7 to 11 admissions per 1 million habitants; APC = −7; p < 0.001). During the whole study period, the mean age of patients with cryoglobulinemia increased from 61.1 to 67.7 years (APC = +0.2; p < 0.001). This trend was more remarkable from 2019 to 2022 (APC = +1.5; p < 0.001). The mortality rate remained fairly stable throughout the whole study period.
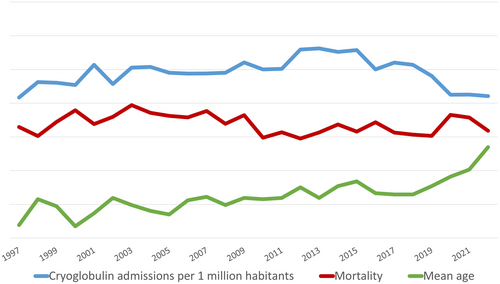
The figure displays the hospital admission rate for cryoglobulinemia, per 1 million habitants, as well as the in-hospital mortality rate and mean age.
3.3 Trends for Cryoglobulinemia Etiologies
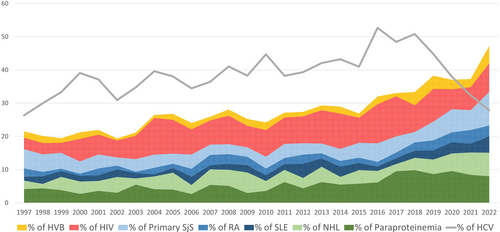
Trends for distinct conditions associated with cryoglobulinemia are recorded in Figure 2, grouped as viral infections, HD, AD and essential cryoglobulinemia. Admissions of patients with essential cryoglobulinemia declined in Spain from 57.3% in 1997 to 37.2% in 2022 (APC = −2; p < 0.001). This trend was more pronounced between 2015 and 2018 (APC = −9.8, p = 0.02). Figure 3 depicts the major conditions related to cryoglobulinemia, including HCV, HBV, HIV, paraproteinemia, NHL, SLE, and primary SjS, over the last 25 years.
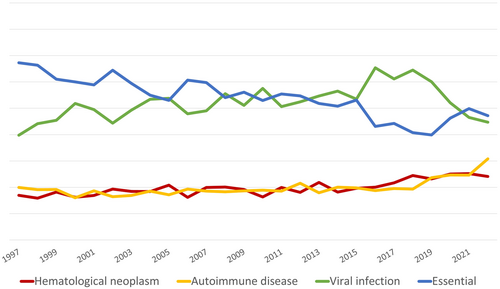
The figure displays the trends in cryoglobulinemia etiologies between 1997 and 2022 in Spain. Data are displayed as percentages with respect to yearly cryoglobulin admissions.
The figure displays the major conditions related to cryoglobulinemia admissions between 1997 and 2022 in Spain. Data are displayed as percentages relative to the total number of yearly cryoglobulinemia admissions with a known aetiology.
3.3.1 Viral Cryoglobulinemic Disease
Admissions with viral-infection associated cryoglobulinemia increased from 29.8% in 1997 to 55.4% in 2016 (APC +2; p < 0.001). Then, it decreased sharply from 54.5% in 2018 to 34.7% in 2022 (APC −9.8; p = 0.001). A drastic drop in admissions with HCV-associated cryoglobulinemia determined this shift, representing 26.3% of all admissions with cryoglobulinemia in 1997, rising to 52.7% in 2016 (APC = +2.3; p < 0.001) and declining again to 27.9% in 2022 (APC = −12.7; p < 0.001) (Figure 4). As a comparison, the rate of HIV infection among admissions with cryoglobulinemia increased from 1997 to 2004 from 3.5% to 11% (APC +15.7; p < 0.001), and since then, it has remained fairly stable. With respect to HBV-associated cryoglobulinemia, it has steadily increased since 2002 up to 2022 from 0.6% to 5.2% (APC +6; p < 0.001).
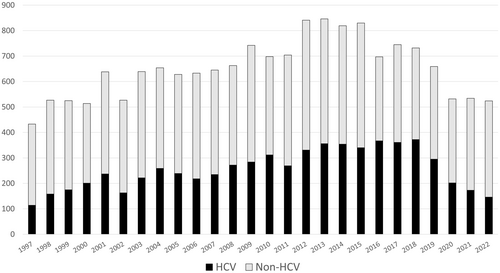
The figure displays the number of yearly admissions of HCV and non-HCV-related cryoglobulinemia between 1997 and 2022 in Spain.
3.3.2 Hematologic and Autoimmune Cryoglobulinemic Disease
Hospitalisations with forms of cryoglobulinemia associated with HC and AD rose during the study period, from 6.9% in 1997 to 14.1% in 2022 (APC +3; p < 0.001) and from 9.9% to 20.8% (APC +2.4; p < 0.001), respectively (Figure 2). Rising rates of paraproteinemia (from 4.2% to 8%, APC +4.2), NHL (from 2.5% to 7.1%, APC +2.3), SLE (from 1.2% to 5%, APC +3), primary SJS (from 5.8% to 10.1%, APC +1.6) and RA (from 2.5% to 3.2%, APC +3.9) were the main contributors to this trend (p < 0.05 for all).
3.4 Current Picture of Patients Hospitalised With Cryoglobulinemia
A total of 524 admissions of patients with cryoglobulinemia were found in Spain in 2022. The mean age was 67.7 years and 56.3% were female. The in-hospital mortality was 5.9% and the mean length of stay 10.7 days. The main etiologies were as follows: HCV (27.9%), primary SjS (10.1%), HIV (8.6%), paraproteinemias (8%), NHL (7.1%), HBV (5.2%), SLE (5%) and RA (3.2%) (Figure 5). Of note, COVID-19 was identified in 11.6% of admissions. In 72.1% of these, no other cryoglobulinemia-associated condition was retrieved. No differences regarding the proportion of females (68.2% vs. 55.2%), age (67.6 vs. 68.9 years old), or mortality rate (11.4% vs. 5.4%) were found in cryoglobulinemia related to COVID-19 with cryoglobulinemia admissions associated with other conditions.
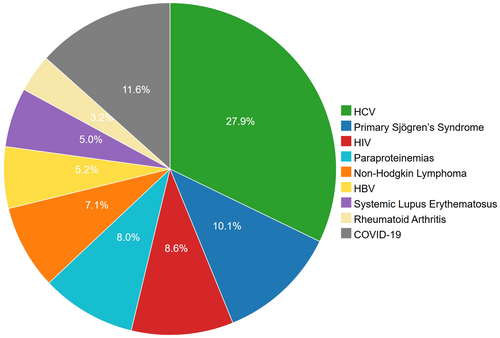
The figure displays the major conditions related to cryoglobulinemia admissions in 2022 in Spain. Data are displayed as percentages relative to the total number of yearly cryoglobulinemia admissions with a known aetiology.
4 Discussion
The introduction and widespread use of DAA as a treatment for hepatitis C have reshaped the etiological framework of cryoglobulinemia over the past decades [9]. This breakthrough therapy has reduced significantly the rate of virus-associated cryoglobulinemia, while other causes, such as hematologic and autoimmune disorders, have gained prominence. Our nationwide study highlights this fact, adding that the patient profile and prognostic factors driving clinical outcomes differ from those in previous decades.
First, our findings show notable changes in the rate of cryoglobulinemia among hospitalised patients in Spain during the last 25 years. Admissions with cryoglobulinemia increased steadily since the late 1990s peaked in 2016 and declined afterwards. This trend, also reported elsewhere, appears driven by the drastic decline in HCV-associated cryoglobulinemia following its 2016 peak, temporally coinciding with the widespread implementation of DAA therapy [8, 15, 16]. These data align with other surveys and support the conclusion, also reached by Boleto et al., that successful HCV control via DAAs is the primary reason for the overall reduction in cryoglobulinemia admissions [8, 15, 17]. However, HCV remains the leading associated condition [8]. This is likely due to persistent cryoglobulin production and vasculitic relapses in around 50% and 12.6% of patients post-sustained virologic response, respectively, in addition to newly identified carriers [18]. All the above underscores the need for continued monitoring for cryoglobulinemic manifestations even after successful HCV clearance [19].
Despite the decline in admissions due to cryoglobulinemia associated with HCV, other viruses such as HBV and HIV remain significant contributors, accounting for approximately 10% and 5% of cases, respectively, in our study. Both are established causes of cryoglobulinemia, likely driven by chronic antigenic stimulation [17, 20-23]. In both infections, antiviral therapy suppresses viral replication but does not eradicate infection [24, 25]. Unlike HBV, whose contribution to cryoglobulinemia-related hospitalisations has gradually increased, HIV-associated cases have remained relatively stable since 2005. This difference might reflect earlier, widespread HIV testing and effective antiretroviral therapy stabilising the immune profile and reducing overt cryoglobulinemic disease risk in HIV patients [13, 17]. In contrast, HBV infection is often underdiagnosed and may go unnoticed until liver- or immune-related complications arise [3, 20]. Persistent antigenic stimulation, potentially driving cryoglobulin production, might still occur in HBV despite viral suppression with nucleos(t)ide analogues.
The number of admissions with cryoglobulinemia associated with hematologic diseases and autoimmune disorders has shown a consistent increase over the 25-year study period, with cases doubling from 1997 to 2022. Therapeutic advances have significantly extended survival in hematologic diseases, often rendering them chronic conditions [26]. While similar progress has been made for many autoimmune disorders, the impact on survival has been probably less pronounced in this field [14, 27]. Indeed, there has been a continuous rise in the rate of admissions with cryoglobulinemia associated with both conditions. Our findings align with literature reporting improved diagnosis and identification of these causes [28-34]. Notably, paraproteinemias and lymphoproliferative disorders for hematologic links [33-36]; and conditions like SLE, primary SjS and RA for autoimmune associations [6, 30, 37, 38]. This evolving understanding has reshaped the epidemiological landscape of cryoglobulinemia, emphasising the need for multidisciplinary approaches to optimise diagnostic and therapeutic strategies.
The growing proportion of autoimmune and hematologic causes of cryoglobulinemia has modified the clinical profile of patients. Building on the observed rise in these conditions, our findings reveal a significant demographic shift. The mean age of patients admitted with cryoglobulinemia rose by 6 years throughout the 25-year study period. This change reflects the decline in cases of virus-associated cryoglobulinemia, particularly those linked to HCV and the stabilisation of HIV-related cases, which are typically seen in younger patients, along with a growing proportion of autoimmune and hematologic-related causes, which predominantly affect older individuals [15, 17, 23]. Therefore, the widespread use of antiviral therapies for HCV and the better management of HIV with antiretroviral therapy have further reduced the impact of viral triggers in younger populations, contributing to the overall increase in the mean age of patients hospitalised with cryoglobulinemia [17, 25].
Altogether, these trends help explain why overall in-hospital mortality remained stable throughout the study period, despite major therapeutic advances such as the introduction of Rituximab and DAAs. While these treatments have significantly improved long-term outcomes—particularly in autoimmune, hematologic and HCV-related cryoglobulinemia—their effect on short-term hospital mortality may be less evident, especially considering their widespread use in outpatient settings [8, 17, 37]. Moreover, changes in the etiological profile of hospitalised patients may have counterbalanced the expected reduction in mortality. While cryoglobulinemia associated with HCV has declined—and primary Sjögren's syndrome, generally associated with milder disease and better outcomes [38], has become more prevalent—there has been a concurrent rise in patients with hematologic malignancies and other severe autoimmune conditions, both of which carry higher baseline mortality [29, 30, 32]. Additionally, the mean age of patients increased significantly over time, further contributing to the overall risk profile. In this context, the stability of in-hospital mortality likely reflects a dynamic equilibrium: on one hand, improvements in diagnosis, early intervention and immunosuppressive therapies (especially Rituximab for Sjögren's syndrome among other AD) may have reduced severe complications in certain subgroups; on the other hand, the increasing age and complexity of hospitalised patients may have offset these gains.
The higher proportion of essential cryoglobulinemia observed in our study compared to previous reports likely reflects inherent methodological differences between specialised single-centre cohorts and our nationwide dataset. Earlier studies reported an approximate 10%–25% prevalence of essential cryoglobulinemia within smaller populations undergoing rigorous serological monitoring [8, 39]. Additionally, the available data on essential cryoglobulinemia prevalence derive mainly from a limited number of such studies, potentially limiting their robustness [1, 3, 40, 41]. In contrast, our broad, nationwide data lacks the intensive surveillance of specialised centres, likely leading to more cases being categorised as ‘essential’. Nonetheless, our findings align with recent trends showing a decrease in essential cryoglobulinemia over time, likely due to improved diagnostics and recognition of underlying causes [1, 3].
Finally, we had the opportunity to examine the impact of COVID-19 on admissions with cryoglobulinemia. SARS-CoV-2 infection can cause immune dysregulation (e.g., hyperinflammation, cytokine release and autoimmunity) [42, 43]; potentially creating an environment conducive to cryoglobulin production. Up to 10% of patients admitted with cryoglobulinemia in 2022 had COVID-19. Additionally, recent reports have described new-onset or relapsing mixed cryoglobulinemia following COVID-19 infection or vaccination [44]. However, our study design does not allow us to assess causality or distinguish between infection- and vaccine-related cases. Further prospective studies are needed to clarify the impact of SARS-CoV-2 infection and vaccination on cryoglobulinemia admissions.
Our study has several limitations. Firstly, reliance on a nationwide hospital discharge database precluded direct diagnosis verification and introduced potential coding inaccuracies. However, since cryoglobulinemia was coded during hospitalisation, likely prompted by compatible symptoms, we believe significant bias from non-systematic testing is unlikely. Secondly, focusing on hospital admissions excludes outpatient cases and may bias towards more severe presentations, limiting generalisability. However, given that cryoglobulinemia often requires hospitalisation due to its severity, this concern might be lower than expected. Furthermore, lack of specific clinical details (serology, viral titers, treatments) limited the analysis scope. Although the coding reflects a clinical diagnosis of cryoglobulinemia, specific clinical presentations (e.g., vasculitis and renal involvement) could not be distinguished, which limits the granularity of phenotype analysis. Due to the nature of the database, we were only able to examine overall cryoglobulinemia-associated hospitalisations; our inability to differentiate between type I and MC may limit the accuracy of mortality analysis. In any case, we analysed the underlying etiologies associated with cryoglobulinemia, providing insight into the evolving causes of disease over time. Despite these limitations, the study's large size, long duration and alignment with trends from smaller studies support the robustness of our findings.
In summary, our nationwide study offers a comprehensive overview of hospital admissions with cryoglobulinemia over a 25-year period. The introduction of antiviral therapies has significantly reduced cases of viral-associated cryoglobulinemia, particularly those associated with HCV, though it remains the predominant aetiology. As a result, there is a noticeable increase in the proportion of cryoglobulinemia associated with hematologic and autoimmune conditions. Finally, the potential role of COVID-19 and/or COVID-19 vaccines warrants closer surveillance.
Author Contributions
Mario Martín-Portugués: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – original draft, writing – review and editing. Jorge Esteban-Sampedro: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – original draft, writing – review and editing. Carmen de Mendoza: conceptualization, investigation, methodology, project administration, supervision, validation, visualization, writing – review and editing. Guillermo Ruiz-Irastorza: conceptualization, investigation, supervision, validation, visualization, writing – review and editing. Ana Royuela: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – review and editing. Alfonso Ortega-de la Puente: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – review and editing. Marina de la Cruz-Echeandía: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – review and editing. Xiomara Patricia Blanco-Valencia: conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, writing – review and editing. Vicente Soriano: conceptualization, data curation, formal analysis, investigation, methodology, software, supervision, validation, visualization, writing – original draft, writing – review and editing. Víctor Moreno-Torres: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, software, validation, visualization, writing – original draft, writing – review and editing.
Ethics Statement
The study complies with the Declaration of Helsinki and received approval from the Ethics Committee of Puerta de Hierro University Hospital (PI 241-24).
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data accessible upon request.