Global Temporal Trends and Projections of Stroke Among Women of Childbearing Age: An Age–Period–Cohort Analysis Based on the Global Burden of Disease Study 2021
Funding: The authors received no specific funding for this work.
ABSTRACT
Background
Stroke is a major global health concern, particularly for women of childbearing age (WCBA), who face unique biological and sociodemographic risks. This study analyzes temporal trends in stroke incidence, prevalence, disability-adjusted life-year (DALY), and deaths among WCBA at global, regional, and national levels over the past three decades, using age–period–cohort (APC) modeling.
Methods
Stroke burden data for WCBA from 1992 to 2021 across 204 countries were extracted from the Global Burden of Disease (GBD) 2021 study. An APC model assessed annual percentage changes in stroke burden (net drift), age group-specific trends (local drift), and relative risks associated with age, period, and cohort factors. Future stroke burden was projected using Bayesian APC models through 2030.
Results
From 1992 to 2021, global stroke incidence cases among WCBA increased from 638,478 to 779,371, but ASIR and AS-DALYs declined. High-SDI regions consistently had the lowest stroke rates, while middle- and low-SDI regions, particularly China and India, accounted for a significant portion of global cases. Despite declines in some regions, countries like the Philippines and Pakistan exhibited rising trends. Projections to 2030 indicate a continued increase in stroke incidence cases, with higher rates expected in middle-income countries due to emerging risk factors like obesity and gestational diabetes.
Conclusions
While ASIR and AS-DALYs declined globally, rising incidence case numbers and persistent disparities highlight the need for targeted prevention and policy strategies, particularly in low- and middle-income regions, to reduce the stroke burden among WCBA.
1 Introduction
Stroke is the second leading cause of death and disability worldwide [1]. While often perceived as a critical health issue for middle-aged and elderly populations, stroke's impact on WCBA should not be overlooked. Pregnancy and the postpartum period (up to 6 weeks after delivery) are recognized as times of elevated stroke risk. These risks are attributed to pregnancy-related hemodynamic changes, a hypercoagulable state, and preexisting or concurrent conditions such as intracranial arteriovenous malformations or aneurysms [2]. Such factors may partly explain why women have a higher stroke incidence than men [1].
In 2021, the global number of strokes among women was estimated at 6.44 million cases [5.81–7.17], with a prevalence of 56.40 million [52.0–61.5]. For men, there were 5.79 million cases [5.24–6.45] and a prevalence of 45.0 million [41.1–49.3]. Notably, these numbers have shown a steady increase over time [3]. An important yet often overlooked subset of WCBA is those in the pregnancy and postpartum periods. Addressing maternal mortality is a central focus of the 2030 WHO Sustainable Development Goals, aiming to reduce global maternal deaths to fewer than 70 per 100,000 live births [4]. Alarmingly, approximately 7.7%–15% of maternal deaths are attributed to stroke, with intracranial hemorrhage (ICH) accounting for the highest mortality rate (13.8%), followed by ischemic stroke (3.9%) [5-7]. Furthermore, stroke is a major contributor to neurological disability, with 30%–50% of affected mothers experiencing persistent functional impairments. These deficits hinder daily activities and the ability to care for newborns. A meta-analysis spanning seven countries and 11 studies estimated the incidence of pregnancy-associated stroke at 30.0 per 100,000 pregnancies (95% CI: 18.8–47.9), which is 1–2 times higher than that observed in nonpregnant women of similar age. Moreover, the incidence of different stroke subtypes in pregnancy-associated stroke is comparable [8]. The health of WCBA not only affects them individually but also profoundly influences the well-being of future generations and the sustainability of societies.
Regrettably, there is currently no comprehensive global analysis of stroke incidence, prevalence, DALY, and deaths among WCBA. Moreover, understanding the temporal trends requires multidimensional interpretations. Stroke burden in this population is influenced by physiological aging (age effect) [9], as well as specific societal and environmental factors during certain periods, such as public health policies, advancements in medical technologies, and lifestyle changes (period effect) [4]. Additionally, the cumulative impact of exposure to early-life social, behavioral, and health risk factors may vary across birth cohorts (cohort effect) [3]. Presently, little is known about the trends in stroke burden among WCBA across low-, middle-, and high-income countries, or how these trends are associated with age, period, and cohort effects.
In this study, we leveraged GBD 2021 data alongside an age–period–cohort (APC) model to examine trends in stroke burden from 1992 to 2021 across 204 countries and territories. We further applied the Bayesian age–period–cohort (BAPC) model to forecast future epidemiological trends, aiming to fill critical knowledge gaps and provide evidence for targeted interventions.
2 Methods
2.1 Data Sources and Disease Definition
The stroke data for WCBA analyzed in this study were derived from the Global Burden of Disease (GBD) 2021 database, developed by the Institute for Health Metrics and Evaluation (IHME). All data are freely accessible through the GBD 2021 platform (https://ghdx.healthdata.org/gbd-2021/sources) [10]. Detailed information regarding data sources, methodology, and statistical modeling is available in previous reports [11].
Stroke is clinically defined by the World Health Organization (WHO) as a sudden onset of neurological dysfunction—typically focal—that persists for more than 24 h or results in death [12]. Within the GBD framework, diseases are categorized into four levels of classification, ranging from the broadest (Level 1, e.g., noncommunicable diseases) to the most specific (Level 4, e.g., intracerebral hemorrhage). Stroke is categorized as a Level 3 cause of death, within the Level 2 category of cardiovascular diseases.
2.2 Study Population
WCBA with Stroke were the subjects of the study. The number of stroke incidence, prevalence, DALY, and deaths among WCBA from 1992 to 2021 were obtained from GBD 2021. DALYs is a measure used to quantify the overall burden of disease, expressed as the number of years lost due to ill-health, disability, or early death. WCBA, defined by the WHO as females aged 15–49, represents the target population for this analysis [13]. WCBA refers to the developmental stage of females with reproductive capacity and cyclic hormonal changes.
2.3 Sociodemographic Index (SDI)
To stratify countries based on their developmental status, GBD 2021 employs the Sociodemographic Index (SDI), a composite measure incorporating income per capita, educational attainment, and fertility rates. Countries are grouped into five SDI quintiles: low, low-middle, middle, high-middle, and high SDI regions.
2.4 ASR Estimation
The ASR for stroke burden among WCBA was calculated using the direct age-standardization method. This method assumes that rates follow a weighted sum distribution of independent Poisson random variables [14]. Seven age groups were evaluated: 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, and 45–49 years.
2.5 Age–Period–Cohort (APC) Model Analysis
The APC model identifies overall temporal trends (net drifts) and specific trends within age groups (local drifts), allowing for a multidimensional analysis of age, period, and birth cohort effects [15, 16]. This study used data from the GBD 2021 database, covering stroke burden and population demographics for WCBA (ages 15–49) from 1992 to 2021. WCBA were divided into seven 5-year age groups (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49 years) and the study period into six 5-year intervals (1992–1996, 1997–2001, 2002–2006, 2007–2011, 2012–2016, 2017–2021). Birth cohorts, spanning 10-year intervals, were partially overlapping, from 1942–1951 to 1997–2006. The periods 2002–2006 and birth cohort 1967–1976 were used as reference points for assessing period and cohort effects. The rate ratio (RR) compares specific periods or cohorts to the reference; an RR > 1 indicates a higher risk compared with the reference group. The APC model estimated both the overall temporal trend (net drift), reflecting annual percentage changes in incidence due to calendar time and successive cohorts, and the age-specific trends (local drift), reflecting changes in incidence within each age group. Wald χ2 tests were conducted to assess the statistical significance of these trends.
2.6 Bayesian Age–Period–Cohort Model Forecasting
Using the results of the GBD study for stroke from 1992 to 2021, the BAPC package in R software was applied to forecast the global stroke burden from 2022 to 2030. The GBD data for 1992–2021 served as a testing dataset to evaluate the accuracy of the BAPC prediction model. A higher degree of model fit accuracy indicates superior predictive performance [16].
2.7 Statistical Analysis
All statistical analyses and visualizations were performed using R Studio (version 4.3.1) and APC Web Tool (https://analysistools.cancer.gov/apc/) [17]. Key R packages included BAPC (version 0.0.36), INLA (version 23.6.29), and ggplot2 (version 3.5.1). A p value < 0.05 was considered statistically significant in all analyses.
3 Result
3.1 Global and SDI-Specific Trends in Stroke Burden
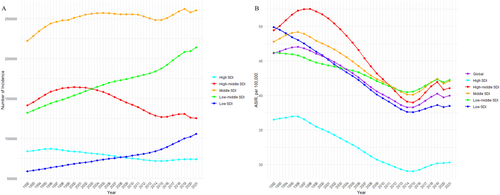
From 1992 to 2021, stroke incidence among WCBA increased from 638,478 to 779,371 cases, though the ASIR declined from 46.12 to 39.99 per 100,000. Stroke incidence cases rose in low, low-middle, and middle SDI regions, while declines occurred in high-middle and high SDI regions. The ASIR trends generally declined across all SDI regions, with a significant rebound around 2015–2016. High SDI regions consistently had the lowest ASIR values (Table 1, Figure 1). In 2021, both DALYs and AS-DALYs for WCBA were lower globally compared to 1992, with similar trends in high SDI and high-middle SDI regions. However, while AS-DALYs rates in middle, low-middle, and low SDI regions were lower in 2021 than in 1992, the total number of DALYs has increased over the past 30 years (Figure S1). APC analysis showed a consistent global decline in stroke incidence (−1.141%/year), prevalence (−0.661%/year), DALY (−1.741%/year) and deaths (−1.968%/year). High-middle SDI regions saw the steepest declines (Figures S7, S13; Tables S2, S3, S4).
| 1992 | 2021 | 1992–2021 APC | |||
|---|---|---|---|---|---|
| Location | Incidence number | Incidence ASR, per 100,000 | Incidence number | Incidence ASR, per 100,000 | Net drift (%/year) |
| Global |
638,478 (554,239, 741,177) |
46.12 (40.03, 53.53) |
779,371 (671,265, 907,034) |
39.99 (34.44, 46.54) |
−1.141 (−1.189, 1.094) |
| Low SDI |
58,649 (51,379, 67,506) |
49.88 (43.7, 57.41) |
105,555 (91,263, 122,704) |
38.48 (33.27, 44.73) |
−1.108 (−1.148, −1.068) |
| Low-middle SDI |
132,130 (115,185, 153,297) |
46.22 (40.29, 53.62) |
213,937 (185,829, 246,462) |
42.26 (36.71, 48.68) |
−0.802 (−0.842, −0.762) |
| Middle SDI |
222,080 (193,055, 259,789) |
47.79 (41.55, 55.91) |
260,246 (223,241, 304,588) |
42.08 (36.1, 49.25) |
−1.39 (−1.455, −1.326) |
| High-middle SDI |
141,159 (122,712, 164,384) |
49.44 (42.98, 57.58) |
125,307 (106,119, 149,321) |
41.07 (34.78, 48.94) |
−1.563 (−1.622, −1.503) |
| High SDI |
83,817 (71,302, 100,138) |
36.51 (31.06, 43.62) |
73,664 (61,577, 88,955) |
30.29 (25.32, 36.58) |
−1.01 (−1.052, −0.969) |
3.2 National Trends in Stroke Burden
In 2021, two nations—China and India—reported over 100,000 incidence cases, jointly accounting for 40.33% of the global burden. These countries are predominantly located in high-middle and low-middle SDI regions. Countries with ASIR values exceeding the global average were identified, with the top five being the Solomon Islands, Nauru, Kiribati, Palau, and Marshall Islands (Figure 2A, Table S1). These nations span various SDI regions: 8 in high, 9 in high-middle, 17 in middle, 16 in low-middle, and 14 in low SDI regions. The countries with the top five AS-DALY values globally are: Nauru, Marshall Islands, Micronesia, Tokelau, and Tuvalu. Among them, the High, High-middle, Middle, Low-middle, and Low SDI regions have 5, 9, 15, 14, and 16 countries (Figure S2A), respectively, reflecting the diverse nature of stroke incidence across countries.
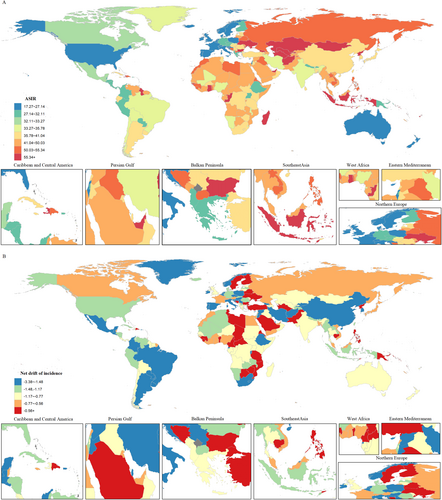
APC model-derived net drift estimates showed rising stroke incidence rates in 15 countries, with one country exceeding an annual net drift of 1% (Figure 2B). These countries were predominantly in low and low-middle SDI regions. The Philippines (middle SDI) exhibited the fastest annual net drift (1.68%; 95% CI: 1.53, 1.83), followed by Palau (high-middle SDI), San Marino (high SDI), and Bhutan (low-middle SDI). Conversely, China led the decline with an annual net drift of −1.831% (95% CI: −1.941, −1.72). Similarly, stroke DALYs increased in 15 countries, including six countries in low-middle SDI regions and four countries in low SDI regions. The net drift values for prevalence, ranked from highest to lowest, were observed in Turkmenistan (middle SDI), the Philippines (middle SDI), and Guam (high-middle SDI). In contrast, the highest net drift values for mortality were recorded in Zimbabwe (low SDI), Lesotho (low SDI), and Sierra Leone (low SDI) (Figures S2B, S8B, S14B).
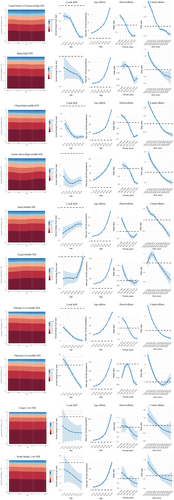
3.3 Age-Specific Temporal Trends in Stroke Burden
We have described the temporal trends in stroke incidence cases across different age groups among WCBA and estimated the annual percentage change (local drift) derived from the APC model (Figure 3). Globally, stroke incidence and DALYs showed a general downward trend, with the steepest declines observed in the 45–49 age group. In all SDI regions, stroke incidence and DALYs have declined across different age groups, showing similar trends. Notably, in low-middle SDI regions, the decline slows down with increasing age, whereas in other regions, the decline accelerates with age (Figures S3, S9, S15).
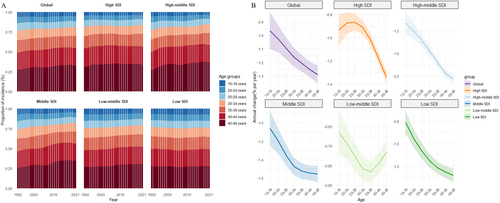
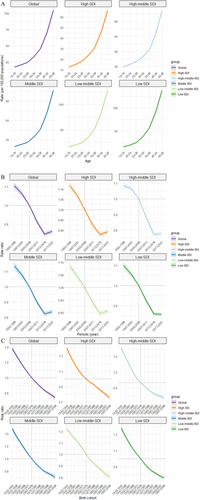
3.4 Age, Period, and Cohort Effects on Stroke Burden
Across different SDI regions, variations in stroke burden rates between age groups were relatively small, with an overall increasing trend (Figure 4A and Figures S4A, S10A, S16A). Overall, the period effect shows a general decline in stroke risk, followed by an increase, with the turning point typically occurring between 2012 and 2016, except in low SDI regions. Compared with the reference period of 2002–2006, the highest relative period risk for incidence in 2017–2021 was 0.907 (95% CI: 0.898, 0.917) in low SDI regions, while the highest relative period risk for DALYs was 0.779 (95% CI: 0.769, 0.791) in low SDI regions (Figure 4B and Figure S4B). Regarding birth cohort effects, stroke risk has decreased across successive birth cohorts globally. This trend is consistent across all SDI regions. Compared with the birth cohort of 1967–1976, the highest relative risk for incidence in the 1997–2006 cohort was 0.807 (95% CI: 0.780, 0.835) in low-middle SDI regions, while the highest relative risk for DALYs in the cohort was 0.638 (95% CI: 0.613, 0.664) in low SDI regions (Figure 4C and Figure S4C).
To illustrate global trends, Figure 5 highlights countries from different SDI regions with distinct age, period, and birth cohort effects. The United States and Japan showed favorable trends, with local drift values across all age groups consistently below 0%. However, the United States had a higher stroke incidence in younger WCBA populations compared with other nations. In densely populated countries like China, the period effect shows an increase in stroke incidence after 2017, a pattern also observed in India. In India, the decline in DALYs slows with age. In South Africa, incidence differences across age groups are small, with an unfavorable period risk during 2002–2006. In Egypt, the local drift for the 45–49 age group is near 0%, with the highest cohort risk in those born between 1952 to 1961. Surprisingly, Ethiopia showed consistently favorable trends, with annual local drift values below −2%. The DALYs age effect is lowest in the 25–29 age group. Notably, in Pakistan, stroke incidence and DALYs in the 19–24 age group have risen each year, with cohort risk increasing for those born after 1987. In Sudan, the number of stroke incidence cases and DALYs was primarily concentrated in younger age groups (Figures S5, S11, S17).
3.5 Projections of Global Stroke Burden to 2030
Using the BAPC model, future trends in stroke incidence cases and ASIR were projected for 2022–2030. Global stroke incidence is expected to rise, reaching 831,161 cases (95% CI: 752,082–910,240) by 2030, with a moderate increase in ASIR to 39.58 per 100,000 (95% CI: 35.81–43.35) (Figure 6A). By 2030, Global stroke DALY cases are projected to decrease to 7,869,751 disability-adjusted life years (DALYs) (95% CI: 7,218,230–8,521,272), while prevalent cases are expected to rise to 11,350,982 (95% CI: 10,664,613–12,037,351), and mortality is estimated to decline to 121,466 deaths (95% CI: 110,533–132,399) (Figures S6A, S12A, S18A).
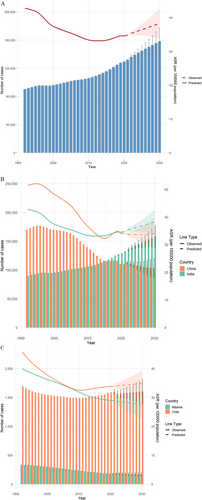
In China, stroke incidence is projected to decrease from 109,035 cases in 2021 (95% CI: 108,582–109,487) to 103,181 cases in 2030 (95% CI: 85,839–120,524), with ASIR stabilizing. In India, stroke incidence is expected to rise from 131,772 cases in 2021 (95% CI: 131,258–132,287) to 158,121 cases in 2030 (95% CI: 139,520–176,722), accompanied by a continuous increase in ASIR. Both countries are expected to see a decrease in stroke DALY cases and AS-DALYs by 2030 (Figure 6B, Figure S6B). The model also predicts sustained increases in stroke burden in Chile (high SDI) and Albania (low-middle SDI). Chile's ASIR is projected to rise to 34.85 (95% CI: 30.28–39.42), while Albania's ASIR will decrease slightly to 27.53 (95% CI: 22.6–32.46) (Figure 6C, Figure S6C). Both countries are expected to see a decrease in DALY cases and AS-DALYs. Detailed forecasts for other countries are provided in Tables S1–S4
4 Discussion
This comprehensive analysis delineates the evolving global burden of stroke among WCBA from 1992 to 2021, with projections extending to 2030. Our findings reveal paradoxical trends: Although the absolute number of stroke incidence cases has increased globally, the age-standardized rates (ASIR and AS-DALYs) have declined, reflecting changes in population structure and heterogeneous progress in different sociodemographic contexts. These trends underscore the dual challenge of population growth and aging against advancements in stroke prevention and management [18], particularly in regions with varying healthcare infrastructure and socioeconomic development.
The net drift rates of incidence, prevalence, DALY, and deaths worldwide highlight progress in mitigating age-specific stroke risks, likely attributable to improved hypertension control, reduced smoking prevalence, and enhanced prenatal care in many regions. However, the persistent rise in absolute case numbers—driven by population growth and aging—emphasizes the urgent need for scalable preventive strategies, particularly in low- and middle-SDI countries. Notably, the divergent trajectories between SDI regions reveal stark inequities: High SDI regions consistently exhibit the lowest ASIR values, while middle SDI regions, which account for 40.33% of global cases, are concentrated in populous countries such as China and India. Additionally, several underdeveloped regions maintain relatively high AS-DALYs and ASMR for stroke. These disparities align with prior studies linking underdeveloped healthcare systems, limited access to acute stroke care, and socioeconomic vulnerabilities to elevated stroke burden in low- and middle-income countries [19, 20].
Highly developed regions benefit from well-established healthcare systems that allow for early detection and effective management of stroke risk factors like hypertension, diabetes, and hypercholesterolemia, contributing to lower stroke incidence and mortality [21]. Widespread health education and accessible prenatal care further support chronic disease management. In contrast, underdeveloped regions often face underdiagnosis, leading to an underestimation of the stroke burden. The lack of medical resources, along with insufficient rehabilitation services, results in high levels of AS-DALYs and ASMR. In these regions, WCBA face compounded health risks from chronic diseases like hypertension and diabetes, as well as infectious diseases, including pregnancy-related infections, further increasing stroke risk [1]. Middle-SDI regions, with rapid urbanization, experience unhealthy dietary patterns, such as increased salt and fat intake, reduced physical activity, and rising smoking and alcohol consumption, all of which elevate stroke risk [22]. Sociocultural factors in some developing countries, like limited access to healthcare and health education for women, can delay interventions for stroke risk factors [23]. Our study projects a continued rise in stroke cases in India, which will pose challenges for stroke management. The rebound in ASIR trends post-2015–2016, particularly in high-middle SDI regions, warrants attention. This inflection point may reflect emerging risk factors, such as the surge in metabolic risks [24, 25] (e.g., the accumulation of obesity, gestational diabetes, and hypertension amid rapid urbanization) and the peak of air pollution [26], as well as the stagnation of public health investments. Conversely, the steepest declines in high-middle SDI regions (−1.563% annual net drift) suggest successful implementation of national stroke prevention programs, as observed in China's aggressive hypertension screening initiatives [27].
Predictive models forecast an ongoing increase in both the absolute case numbers and age-standardized incidence rates of stroke among WCBA by 2030, presenting challenges to the WHO's 2030 health targets. Among WCBA, stroke in pregnant and postpartum women has particularly severe consequences, with pregnancy-related hypertensive disorders (e.g., preeclampsia) being a significant risk factor, especially in younger women and primiparas. This is especially problematic in developing countries, where poor hypertension management exacerbates the issue [28]. Stroke leads to maternal mortality, preterm birth, and low birth weight [29], while impairments severely affect WCBA's quality of life, including motor and cognitive dysfunctions that impact family and professional responsibilities [30]. Additionally, women poststroke often face anxiety and depression, hindering recovery and affecting their families [31]. The economic burden of stroke on WCBA is considerable, with costly treatments and long-term rehabilitation placing a financial strain on families, especially in low- and middle-income countries [32]. Stroke survivors may also experience reduced labor force participation, further impacting societal productivity [33].
Addressing stroke prevention in WCBA is essential to reduce health and economic burdens while promoting gender equality and societal development. Improved maternal health management, including better control of risk factors like hypertensive disorders during pregnancy, diabetes, and smoking cessation, can reduce maternal and perinatal mortality [34]. Promoting prevention and early intervention in low- and middle-income countries can reduce health inequities and support global health goals. Reducing stroke incidence and improving recovery would enhance labor participation and alleviate economic pressures, contributing to sustainable development. A thorough understanding of epidemiological trends in this population is vital for accurate disease assessment and achieving health objectives.
The APC analysis elucidates critical temporal and generational influences. Although pregnancy-related stroke plays an undeniable role, age remains the most important risk factor for stroke, driven by cumulative vascular aging, atherosclerosis, and endothelial dysfunction. This trend is also evident in WCBA, especially in those approaching the end of their reproductive years (≥ 40 years) [35]. As age increases, WCBA accumulate cardiovascular risk factors like hypertension, diabetes, obesity, and hyperlipidemia [36]. Period effects show an overall decline, likely attributable to advancements in global stroke diagnosis and treatment (e.g., thrombolysis, early rehabilitation), especially in high- and middle-SDI regions, where stroke incidence and mortality have decreased [37]. Simultaneously, strengthened preventive measures targeting stroke risk factors such as hypertension and diabetes, alongside public health campaigns promoting smoking cessation and healthier diets, have shown marked success in high- and middle-income countries [38]. However, cohort risks have slightly increased from 2017 to 2021, potentially linked to the global rise in obesity, diabetes, and unhealthy lifestyles (e.g., sedentary behaviors, high-salt and high-fat diets) [3]. The COVID-19 pandemic further compounded these challenges by delaying acute stroke care, exacerbating unhealthy behaviors (e.g., reduced physical activity), and disrupting chronic disease management [39]. Birth cohort effects reveal that later-born individuals exhibit lower overall risks compared to earlier cohorts. This can be attributed to improved childhood health environments, earlier access to health education, reduced infectious disease burdens, and better early-life nutrition, all of which reduce the risk of stroke-related diseases [40, 41].
Among 204 countries and regions, there is significant heterogeneity in the age, period, and cohort effects of stroke incidence in WCBA. While global trends indicate overall improvement, countries like the Philippines show the fastest growth in incidence. Rising cohort risks in Pakistan and Egypt highlight gaps in addressing metabolic and lifestyle-related risks in younger WCBA. This underscores the need for country-specific strategies. China's success may be due to its National Stroke Screening Project and improved healthcare access, while India's challenges stem from rural–urban disparities and high untreated hypertension rates. The contrasting trends in Chile and Albania reflect the complex influence of lifestyle, healthcare funding, and political prioritization of noncommunicable diseases.
Despite its strengths, our study has limitations. First, limited healthcare infrastructure in some underdeveloped regions may lead to misdiagnoses or underreporting, underestimating the true incidence. Second, reliance on GBD-modeled data introduces uncertainties, especially in countries with sparse primary data, affecting the accuracy of age, period, and cohort effects. Third, the lack of specific data on stroke during pregnancy in the GBD database limits our ability to assess global trends in pregnancy-associated stroke. Addressing this gap requires future epidemiological research. Lastly, the time lag in GBD data updates may limit the immediacy of our findings.
5 Conclusion
This study highlights the evolving global burden of stroke among WCBA, showing a decline in ASIR and AS-DALYs, despite an increase in absolute case numbers due to population growth and aging. In addition, certain countries are experiencing adverse increases, with the Philippines showing the most pronounced upward trend. Moreover, many nations face worsening period or cohort risks, underscoring the substantial inadequacy of resources allocated to stroke prevention and health care for the WCBA population. These findings emphasize the urgent need for stronger, more nuanced healthcare and public health policies tailored to the specific circumstances of individual countries. For developing nations, integrating stroke prevention into broader economic development plans is essential. To achieve the sustainable development goal of reducing global maternal mortality by 2030, global health initiatives must prioritize WCBA, with special attention to older pregnant women. Strengthening preventive strategies and improving access to healthcare for this population are critical steps to mitigate the increasing burden of stroke and ensure better health outcomes for women and their families.
Author Contributions
Dong Tang: conceptualization, investigation, funding acquisition, writing – original draft, methodology, validation, visualization, writing – review and editing, software, formal analysis, project administration, data curation, supervision, resources. Zheng Huang: investigation, formal analysis. Shifu Li: conceptualization, methodology, software. Qian Zhang: software, methodology, validation. Mengjun Li: supervision, writing – review and editing. Yangzong Zhou: software. Kangtai Su: resources. Fenghua Chen: conceptualization, writing – original draft, writing – review and editing, methodology, supervision.
Acknowledgments
Thank you to all members of the GBD Database Collaboration Group.
Ethics Statement
As this study utilizes publicly available data from the Global Burden of Disease (GBD) database, which is anonymized and does not involve direct patient interaction or collection of primary data, the Institutional Review Board of the Xiangya Hospital of Central South University determined that approval for this research was not necessary. The GBD database adheres to ethical guidelines in data collection and dissemination, ensuring compliance with ethical standards. This study conforms to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) for cross-sectional studies.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data used from the GHDx platform (https://vizhub.healthdata.org/gbd-results/).




