The Unruptured Intracranial Aneurysm Treatment Score as a predictor of aneurysm growth or rupture
Abstract
Background and purpose
The Unruptured Intracranial Aneurysm Treatment Score (UIATS) was built to harmonize the treatment decision making on unruptured intracranial aneurysms. Therefore, it may also function as a predictor of aneurysm progression. In this study, we aimed to assess the validity of the UIATS model to identify aneurysms at risk of growth or rupture during follow-up.
Methods
We calculated the UIATS for a consecutive series of conservatively treated unruptured intracranial aneurysms, included in our prospectively kept neurovascular database. Computed tomography angiography and/or magnetic resonance angiography imaging at baseline and during follow-up was analyzed to detect aneurysm growth. We defined rupture as a cerebrospinal fluid or computed tomography–proven subarachnoid hemorrhage. We calculated the area under the receiver operator curve, sensitivity, and specificity, to determine the performance of the UIATS model.
Results
We included 214 consecutive patients with 277 unruptured intracranial aneurysms. Aneurysms were followed for a median period of 1.3 years (range 0.3–11.7 years). During follow-up, 17 aneurysms enlarged (6.1%), and two aneurysms ruptured (0.7%). The UIATS model showed a sensitivity of 80% and a specificity of 44%. The area under the receiver operator curve was 0.62 (95% confidence interval 0.46–0.79).
Conclusions
Our observational study involving consecutive patients with an unruptured intracranial aneurysm showed poor performance of the UIATS model to predict aneurysm growth or rupture during follow-up.
INTRODUCTION
Unruptured intracranial aneurysms constitute a relatively frequently encountered neurovascular disease, with a prevalence of around 3% in the general population [1, 2]. Aneurysm rupture leading to a subarachnoid hemorrhage (SAH) is associated with high morbidity and mortality rates [3]. In this respect, proactive treatment via aneurysm clipping or coiling is seen as the cornerstone of rupture prevention. Because elective treatment also bears procedural risks, it should be balanced against the estimated risk of future aneurysm rupture. Therefore, conservative treatment may be the preferred treatment strategy for aneurysms deemed low risk. Typically, short-term follow-up of such aneurysms is indicated, enabling the detection of potential aneurysm growth and facilitating timely reevaluation of elective treatment [4].
Various risk-assessment tools have been introduced to assist in the treatment decision making of unruptured aneurysms. The Unruptured Intracranial Aneurysm Treatment Score (UIATS) is relatively new and represents the most extensive risk-assessment tool [5]. The UIATS is a Delphi consensus-based model, consisting of 29 variables compromising patient-, aneurysm-, as well as treatment-specific variables. Points are given for each variable in the model, either in favor of elective treatment or conservative management. The result is a recommendation to treat or not to treat an aneurysm (Table 1). A point difference smaller than three results in an inconclusive recommendation. Despite its extensiveness, its clinical predictive performance and external validity remain largely unknown.
| Variables | Categories | Points in favor of treatment | Points in favor of conservative management |
|---|---|---|---|
| Age | <40 years | 4 | |
| 40–60 years | 3 | ||
| 61–70 years | 2 | ||
| 71–80 years | 1 | ||
| >80 years | 0 | ||
| Risk factor incidence | Previous SAH from a different aneurysm or SAH | 4 | |
| Familial intracranial aneurysms or SAH | 3 | ||
| Japanese, Finnish, Inuit ethnicity | 2 | ||
| Current cigarette smoking | 3 | ||
| Hypertension | 2 | ||
| Autosomal polycystic kidney disease | 2 | ||
| Current drug abuse | 2 | ||
| Current alcohol abuse | 1 | ||
| Clinical symptoms related to UIA | Cranial nerve deficit | 4 | |
| Clinical or radiological mass effect | 4 | ||
| Thromboembolic events from the aneurysm | 3 | ||
| Epilepsy | 1 | ||
| Other | Reduced quality of life due to fear of rupture | 2 | |
| Aneurysm multiplicity | 1 | ||
| Life expectancy due to chronic and/or malignant diseases | <5 years | 4 | |
| 5–10 years | 3 | ||
| >10 years | 1 | ||
| Comorbid disease | Neurocognitive disorder | 3 | |
| Coagulopathies, thrombophilic diseases | 2 | ||
| Psychiatric disorder | 2 | ||
| Maximum diameter | ≤3.9 mm | 0 | |
| 4.0–6.9 mm | 1 | ||
| 7.0–12.9 mm | 2 | ||
| 13.0–24.0 mm | 3 | ||
| ≥25 mm | 4 | ||
| Morphology | Irregularity or lobulation | 3 | |
| Size ratio >3 or aspect ratio >1.6 | 1 | ||
| Aneurysm location | Basilar bifurcation | 5 | |
| Vertebral/basilar artery | 4 | ||
| ACoA or PCoA | 2 | ||
| Other | Aneurysm growth on serial imaging | 4 | |
| Aneurysm de novo formation on serial imaging | 3 | ||
| Contralateral steno-occlusive vessel disease | 1 | ||
| Age-related risk | <40 years | 0 | |
| 40–60 years | 1 | ||
| 61–70 years | 3 | ||
| 71–80 years | 4 | ||
| >80 years | 5 | ||
| Aneurysm size-related risk | <6.0 mm | 0 | |
| 6.0–10 mm | 1 | ||
| 10.1–20.0 mm | 3 | ||
| >20 mm | 5 | ||
| Aneurysm complexity-related risk | High | 3 | |
| Low | 0 | ||
| Intervention-related risk | Constant | 5 |
Note
- Adapted from Etminan et al. [5]. A point difference ≥3 results in a recommendation favoring the treatment strategy with the highest number of points. If the difference is ≤2, an inconclusive recommendation is given.
- Abbreviations: ACoA, anterior communicating artery; ADPKD, autosomal dominant polycystic kidney disease; PCoA, posterior communicating artery; SAH, subarachnoid hemorrhage; UIA, unruptured intracranial aneurysm.
The primary objective of this study was to determine the ability of the UIATS model to identify unruptured intracranial aneurysms at risk of growth or rupture during follow-up.
METHODS
Study population
All adult patients with a conservatively treated, unruptured intracranial aneurysm, assessed between 1997 and 2017, were consecutively included in our prospectively kept neurovascular database. The decision for conservative management of the aneurysm was made by the multidisciplinary neurovascular group at our tertiary referral center. We excluded extradural aneurysms and patients without follow-up imaging. Patients signed an informed consent as required by our University Medical Center Groningen Research Ethical Board.
Data collection
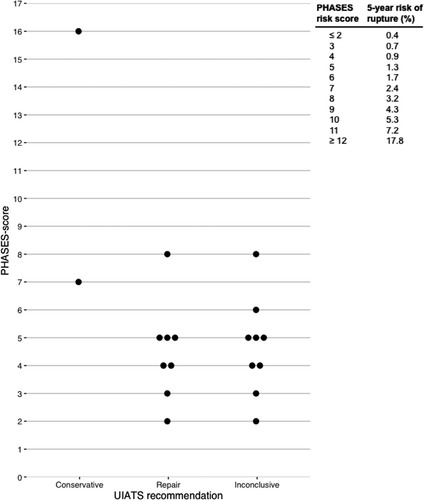
We used questionnaires and chart reviews to acquire data regarding the 29 variables described in the UIATS model (Table 1). The questionnaires were mainly used to ask if patients experienced a reduced quality of life due to fear of rupture, as well as double checking UIATS-related patient-specific risk factors potentially not mentioned in the patients’ referral information. We omitted the variables aneurysm growth and aneurysm de novo formation on serial imaging, because we calculated UIATS recommendations at baseline. Aneurysm measurements were based on three-dimensional (3D) time-of-flight magnetic resonance angiography with 0.6-mm slice thickness or contrast-enhanced computed tomography angiography with 0.75-mm slice thickness. We measured aneurysm height, width, and neck diameter at baseline and during follow-up to detect aneurysm growth. Aneurysm shape was evaluated using 3D reconstructions, with an irregular shape defined as the presence of blebs, wall protrusions, or multiple lobes [6]. Growth was defined as either an increase in size of at least 1 mm in at least one direction, or a change in aneurysm shape [7]. We defined rupture as a computed tomography– and/or cerebrospinal fluid–proven SAH. For all unstable aneurysms (i.e., those with growth or rupture), we also calculated the PHASES score. PHASES stands for the variables population, hypertension, age, size of the aneurysm, earlier SAH from another aneurysm, and site of the aneurysm, which can be used to estimate the 5-year risk of rupture [8]. We used the PHASES score to evaluate the estimated risk distribution of the unstable aneurysms at baseline.
Statistical analysis
UIATS recommendations were determined by calculating the sum of points for each strategy (treatment vs. conservative). Aneurysms with an inconclusive recommendation were excluded from statistical analysis. Aneurysms with a treatment recommendation showing progression during follow-up were considered as true positives, whereas those receiving a conservative recommendation showing progression during follow-up were considered as false negatives. We used the Fisher exact test for group comparisons of categorical data, and the Student t test or Mann-Whitney U test for continuous data. The level of statistical significance was set at 0.05. We calculated the sensitivity, specificity, positive and negative predictive value, and the area under the receiver operator curve (AUC) to assess the performance of the UIATS model to discriminate between aneurysms with and without progression. Statistical analyses were performed using SPSS (version 23.0; IBM Corp.).
RESULTS
A total of 214 patients (277 unruptured aneurysms) with a conservative treatment recommendation were assessed. The majority of patients (74%) were female. Aneurysms were followed for a median period of 1.3 years (range 0.3–11.7 years). During follow-up, 17 (6.1%) aneurysms enlarged, and two (0.7%) aneurysms ruptured. Median duration to the occurrence of growth or rupture was 2.45 years (range 0.8–9.8 years). Based on the UIATS model, a total of 88 (32%) aneurysms received a treatment recommendation, 65 (23%) received a conservative recommendation, and for 124 (45%) the UIATS recommendation was inconclusive (Table 2). The majority of unstable aneurysms had a relatively low estimated 5-year rupture risk based on the PHASES score at baseline, generally favoring conservative treatment. One large aneurysm of the anterior communicating artery with a high PHASES score of 16 was treated conservatively due to the patients’ older age, intra-aneurysmal thrombosis, and significant comorbidities. No clear differences between PHASES scores and UIATS recommendations could be identified (Figure 1).
| UIATS recommendation | Stable, n = 258 | Unstable, n = 19 |
|---|---|---|
| Repair | 80 (31) | 8 (42) |
| Conservative management | 63 (24) | 2 (11) |
| Inconclusive | 115 (45) | 9 (47) |
Note
- Data are displayed as n (%).
- Abbreviation: UIATS, Unruptured Intracranial Aneurysm Treatment Score.
Besides older age, high aneurysm complexity risk (mainly due to small aneurysm size) was the only variable associated with favoring a conservative recommendation (Table 3). Variables associated with favoring a treatment recommendation were: (i) a previous SAH from a different aneurysm, (ii) familial intracranial aneurysms or SAH, (iii) current smoking, (iv) current alcohol abuse, (v) reduced quality of life due to fear of rupture, and (vi) aneurysm multiplicity. Subsequent analysis of the UIATS model showed a sensitivity of 80%, a specificity of 44%, a positive predictive value of 9%, and a negative predictive value of 97% (Table 2). The AUC of the receiver operator curve was 0.62 (95% confidence interval [CI] 0.46–0.79), implicating poor performance of the UIATS model to discriminate between stable and unstable aneurysms.
| Variable | Total group, N = 277 | UIATS treatment recommendation | p value* | ||
|---|---|---|---|---|---|
| Repair, n = 88 | Conservative, n = 65 | Inconclusive, n = 124 | |||
| Mean age ± SD, years | 57 ± 10 | 51 ± 8 | 64 ± 9 | 57 ± 10 | 0.33 |
| Risk factor incidence | |||||
| Previous SAH from a different aneurysm | 109 (39) | 53 (60) | 16 (25) | 40 (32) | <0.01 |
| Familial intracranial aneurysms or SAH | 48 (17) | 24 (27) | 6 (9) | 18 (15) | 0.01 |
| Current cigarette smoking | 122 (44) | 65 (74) | 9 (14) | 48 (39) | <0.01 |
| Hypertension | 133 (48) | 49 (56) | 30 (46) | 54 (44) | 0.26 |
| ADPKD | 10 (4) | 5 (6) | 1 (2) | 4 (3) | 0.24 |
| Current alcohol abuse | 12 (4) | 9 (10) | 1 (2) | 2 (2) | 0.045 |
| Clinical symptoms related to UIA | |||||
| Epilepsy | 1 (0.4) | 1 (1) | 0 | 0 | 1.0 |
| Other | |||||
| Reduced quality of life due to fear of rupture | 68 (25) | 38 (43) | 10 (15) | 20 (16) | <0.01 |
| Aneurysm multiplicity | 180 (65) | 70 (80) | 32 (49) | 78 (63) | <0.01 |
| Reduced life expectancy | 2 (0.7) | 0 | 1 (2) | 1 (1) | 0.43 |
| Comorbid disease | |||||
| Neurocognitive disorder | 2 (0.7) | 0 | 2 (3) | 0 | 0.18 |
| Psychiatric disorder | 4 (1.4) | 0 | 3 (5) | 1 (1) | 0.08 |
| Morphology | |||||
| Mean maximum diameter ± SD, mm | 4.6 ± 2.7 | 4.1 ± 3.4 | 5.3 ± 2.8 | 4.7 ± 2.8 | 0.1 |
| Irregularity or lobulation | 23 (8.3) | 9 (10) | 2 (3) | 12 (10) | 0.12 |
| Size ratio >3 or aspect ratio >1.6 | 60 (22) | 19 (22) | 11 (17) | 30 (24) | 0.54 |
| Location | |||||
| BA bifurcation | 13 (4.7) | 7 (8) | 1 (2) | 5 (4) | 0.14 |
| ACoA or PCoA | 57 (21) | 16 (18) | 12 (18) | 29 (23) | 1.0 |
| Other | |||||
| Contralateral steno-occlusive vessel disease | 1 (0.4) | 0 | 0 | 1 (1) | N/A |
| High aneurysm complexity-related risk | 148 (53) | 33 (38) | 52 (80) | 63 (51) | <0.01 |
Note
- Data are displayed as n (%) unless indicated otherwise. The following variables were omitted from this table because no patients or aneurysms were included in these categories: Japanese, Finnish, or Inuit ethnicity; current drug abuse; cranial nerve deficit; clinical or radiological mass effect; thromboembolic events from the aneurysm; coagulopathies; thrombophilic diseases; and aneurysms located at the vertebral/basilar artery.
- Abbreviations: ACoA, anterior communicating artery; ADPKD, autosomal dominant polycystic kidney disease; BA, basilar artery; N/A, not applicable; PCoA, posterior communicating artery; SAH, subarachnoid hemorrhage; UIA, unruptured intracranial aneurysm; UIATS, Unruptured Intracranial Aneurysm Treatment Score.
- * Statistical significance of the difference between repair and conservative.
DISCUSSION
We evaluated whether the UIATS model is valid to predict growth or rupture of unruptured intracranial aneurysms during follow-up. The results of our study show that aneurysm progression during follow-up could not be reliably predicted by the UIATS model. In addition, almost one-third of aneurysms remaining stable during follow-up received a treatment recommendation. On the other hand, nearly half of the aneurysms in this study received an inconclusive recommendation, whereas the number of aneurysms with growth or rupture was highest in this category.
To our knowledge, two other studies investigated the predictive performance of the UIATS model. The first study performed a retrospective analysis of 212 consecutive SAH patients at their institution [9]. They calculated UIATS recommendations for all aneurysms to determine which aneurysms would have received a treatment recommendation (true positives) or a conservative treatment recommendation (false negatives). Analysis demonstrated a relatively low sensitivity of 44% in detecting aneurysms at risk of rupture. The second study described 142 patients with 182 unruptured intracranial aneurysms diagnosed between 1956 and 1978 [10]. Patients were followed for a median period of 21 years (range 0.8–52.3 years). The UIATS demonstrated poor performance to predict rupture, with an AUC of 0.62 (95% CI 0.50–0.73). It should be noted that these aneurysms were almost all incidental findings after an SAH from a different aneurysm, and UIATS points given due to their Finnish nationality also increased the likelihood of a UIATS recommendation favoring treatment. We therefore believe our study adds to this by providing a more contemporary cohort of patients. In our large group of aneurysms, a significant proportion of aneurysms was discovered incidentally on brain imaging in patients without a previous SAH, and follow-up angiography was performed to identify potential aneurysm growth.
In contrast to other models used in the assessment of unruptured aneurysms (e.g., the PHASES score), the UIATS model is not based on longitudinal collected data regarding risk factors of aneurysm progression [8]. Instead, a Delphi consensus-based approach was used in constructing the model, and the model was not validated. The developers of the UIATS model state that the model enables clinicians to appreciate what highly informed individuals in the cerebrovascular field would advise in a particular patient based on current data and uncertainties. They also state that its applicability and clinical accuracy remains to be investigated. In this respect, multiple cerebrovascular institutions compared the UIATS treatment recommendation with decisions made by their own multidisciplinary teams [11-13]. Despite all studies using different statistical methods of comparing the UIATS recommendation to their own treatment decisions, they all show limited agreement between the two.
Of interest, in accordance with the results presented in this article, most studies investigating the UIATS show only a minor role of aneurysm size in the determination of the UIATS treatment recommendation [11, 12]. This is remarkable, because aneurysm size is a well-studied variable and one of the strongest predictors of rupture [14]. It seems to result from the fact that aneurysm size is both represented as a variable favoring aneurysm treatment as well as favoring conservative management, whereas different size categories are also used for the two. Consequently, the effect of aneurysm size on the UIATS stays between one point in favor of aneurysm repair and two points in favor of conservative management, for the full range of aneurysm sizes [15]. The result is an almost nonexistent effect of aneurysm size on UIATS recommendation.
Our study does have some limitations. First, treatment decisions for individual aneurysms by our multidisciplinary neurovascular working group may be different than other neurovascular centers, potentially limiting the generalizability of our results. Second, our focus on conservatively treated aneurysms might underestimate the performance of the UIATS model to predict progression due to the inclusion of mostly aneurysms deemed low risk by our working group. Hence, included aneurysms are relatively small, and the majority of aneurysms are located in the anterior circulation, because posterior circulation aneurysms are frequently deemed more high risk and therefore more frequently treated. Finally, the mean duration of follow-up was relatively short, preventing assessment of the UIATS performance over a longer period of follow-up.
CONCLUSIONS
This observational study involving patients with unruptured intracranial aneurysms who underwent follow-up imaging at our institution demonstrated poor performance of the UIATS model to predict aneurysm progression during follow-up.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Rob Molenberg: conceptualization (equal); dataCuration (equal); formalAnalysis (equal); investigation (equal); methodology (equal); projectAdministration (equal); writingOriginalDraft (equal). Marlien W. Aalbers: conceptualization (equal); dataCuration (equal); investigation (equal); methodology (equal); writingReviewEditing (equal). Aryan Mazuri: dataCuration (equal); writingReviewEditing (equal). Gert Jan Luijckx: dataCuration (equal); writingReviewEditing (equal). Jan D. M. Metzemaekers: dataCuration (equal); writingReviewEditing (equal). Rob J. M. Groen: dataCuration (equal); writingReviewEditing (equal). Maarten Uyttenboogaart: conceptualization (equal); dataCuration (equal); methodology (equal); writingReviewEditing (equal). J. Marc C. van Dijk: conceptualization (equal); dataCuration (equal); methodology (equal); supervision (equal); writingReviewEditing (equal).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




