Public health policies in dental traumatology: A call for action!
Daniela Atili Brandini and Ana Beatriz Carvalho de Souza Cantão should be considered joint first author.
Abstract
Traumatic dental injuries (TDI) are a prevalent public health concern, requiring preventive measures as well as timely and appropriate interventions to prevent adverse outcomes and optimize patients' prognosis. Although dental trauma injuries require prompt clinical intervention, some challenges persist in effectively managing these injuries. In dental traumatology, the implementation of public health policies assumes critical importance, these policies play an important role in addressing preventive measures and mitigating the repercussions of TDI. This review aims to emphasize the importance of developing comprehensive public health policies in dental traumatology, recognizing the strategic importance of this approach and its benefits. By proactively addressing issues associated with dental injuries, these policies have extensive implications for individual quality of life and public health in general. Furthermore, this review will present a suggested structured framework for the development of public health policies, encompassing key domains including prevention, intervention, and education in dental traumatology. The creation and implementation of these policies will address dental trauma through prevention programs, research, and development, and will provide a significant step toward enhancing the well-being of the population and dental trauma victims' prognosis promoting a more resilient healthcare system.
1 INTRODUCTION
Traumatic dental injuries (TDI) are a common public health concern that affects teeth and surrounding structures in the mouth and oral cavity. These injuries are typically accidental and usually require immediate attention. TDI have been estimated as the second most frequent oral condition and the world's fifth most prevalent disease or injury.1 This underscores the substantial public health implications of traumatic dental injuries, making it a widespread concern affecting a broad demographic, particularly the younger population. The prevalence and incidence of traumatic dental injuries are globally significant, impacting both primary and permanent dentitions.1, 2 Although TDI prevalence and incidence are generally high worldwide, they may vary considerably and are a neglected condition even in developed countries. Issues regarding the availability, organization, and management of emergency services for the management of TDI had been reported.3
The clinical challenges in traumatic dental injuries, encompassing fractures, luxations, avulsions, and soft tissue injuries, necessitate timely intervention to prevent complications. The associated financial burden further extends to healthcare systems and individuals alike, emphasizing the clinical and financial implications of effective management.4, 5 Management of TDI can be expensive and time-consuming. The severity and complexity of injuries correlate with elevated direct and indirect expenses. The direct costs of managing dental injuries encompass emergency care and the ongoing treatment requirements throughout the patient's lifetime. In addition, indirect costs include the time spent away from school or work and transportation expenses.4-7 These costs are incurred not just during the initial trauma management but also during subsequent follow-up visits, the duration of which may vary depending on the extent of the traumatic injury and the development of complications. Quality of life might also be significantly compromised, as pain, altered appearance, and functional limitations stemming from the dental trauma may impact daily activities, social interactions, and emotional well-being.8-12 Adopting a multidisciplinary approach is imperative, as dental trauma often coexists with injuries in other body parts, requiring collaboration among dentists, physicians, and emergency responders for comprehensive care.
The prompt and proper treatment of dental trauma is crucial for ensuring optimal outcomes and mitigating the potential long-term consequences associated with such injuries. The importance of prompt treatment is underscored by its potential to improve the prognosis and overall success of managing dental trauma.13 Timely and effective care reduces immediate complications and prevents secondary issues that may arise with delayed interventions. In conjunction with individual clinical approaches, public health policies in dental trauma might play a vital role in supporting prompt treatment by promoting awareness, education, and preventive measures within communities.14, 15 Policies advocating for oral health education, safety protocols in sports, and access to timely dental care might contribute to the holistic approach in preventing and managing dental trauma at both the individual and population levels.
Public health policies encompass government strategies and guidelines designed to promote and safeguard the health of the population. It is defined as the power and duty of the state to guarantee the conditions for people to be healthy.16 This includes both the strategic public health policy of the state or country in terms of its role and responsibilities in relation to the health of the population, and the functional policies that define the interventions it is prepared to carry out to execute its strategy. The policy is determined by a process of consultation, negotiation, and research, leading to an action plan that sets out a vision of the public health objectives identified. Public health policies, with regards to TDI, may involve awareness strategies about safety measures in sports activities, and public education to discourage harmful habits and establish rapid intervention protocols for cases of dental trauma.17-20 In the context of public health, policy is usually determined by the political or executive arm of the municipality, state, or country, although private or public health agencies can also formulate policies about their public health objectives. Public health policy can be descriptive, in that it sets out an approach to a public health issue, or prescriptive, in that it requires some follow-up action.21
In dental trauma, the importance of public health policies lies in their ability to address preventive measures and mitigate the consequences of traumatic injuries. The effective implementation of these policies will contribute to reducing the incidence of trauma and to ensure equitable access to oral health services and promote a comprehensive approach to managing these situations. Therefore, the integration of public health policies is crucial to improving oral health outcomes and ensuring that the population is better informed and protected against the risks associated with TDI.
Dental trauma guidelines play a crucial role in providing standardized, evidence-based approaches to the diagnosis, treatment, and prevention of dental injuries. Currently, there are established guidelines by the International Association of Dental Traumatology (IADT),8, 22-24 which focus on the management of traumatic dental injuries. These guidelines stress the importance of immediate or urgent care for dental trauma. Additionally, recently, the IADT and the Academy for Sports Dentistry (ASD) published joint guidelines for the prevention of TDI.18, 20, 25-32
The World Health Organization (WHO) guide33 provides guidelines for the prevention and management of oral diseases and promotes global initiatives to improve oral health and prevent oral diseases. These initiatives often focus on preventive measures, early detection, and access to dental care. The WHO recognizes the need for emergency care and rehabilitation services for individuals who experience dental trauma. However, there is still a lack of proper comprehensive inclusion of TDI in the WHO guide.
The International Federation for Dentistry (FDI)34 focuses mainly on developing global policies, standards, and guidelines relating to oral health practices, including dental trauma. The initiatives often involve promoting preventive measures, raising awareness, and supporting policies that enhance dental care globally. The FDI contributes to providing recommendations for dental professionals, including policy statements related to dental trauma. These policy statements aim to ensure standardized and evidence-based approaches to dealing with traumatic dental injuries.
Although dental trauma treatments are patient-specific, these guidelines are essential for dental professionals, including dentists, dental hygienists, and emergency medical personnel, to ensure consistent and optimal care for patients who suffer from dental trauma.
This review aims to emphasize the creation of comprehensive public health policies in dental traumatology, recognizing the strategic relevance of this approach. The importance of these policies is in the proactive addressing of issues associated with dental injuries, impacting the individual quality of life and holding substantial implications for public health at large. Additionally, this review provides a suggested structured framework for creating these policies, covering areas such as prevention, intervention, and education.
2 SUGGESTED FRAMEWORKS FOR PUBLIC HEALTH POLICIES IN DENTAL TRAUMATOLOGY
Public health policies can operate on several different levels, which affects the health of the population.35 In dental traumatology, public health policies should take shape on several levels. These include primary prevention, which aims to educate patients and professionals about the occurrence of dental trauma and how to prevent or reduce its rates, and secondary prevention which aims to prevent the development of a disease at a high stage by diagnosing and treating the disease effectively, contributing to a better diagnosis and proper treatment.20 The interventions involve individual-level behavioral approaches to disease prevention or management, and their success depends on several factors such as the population being more likely to take up or get involved with policies in certain initiatives compared to others.
A framework for public health policies in dental traumatology should be multilayered and include various aspects of public health issues related to the prevention and treatment of TDI. A suggested framework is described below and depicted in Figure 1.
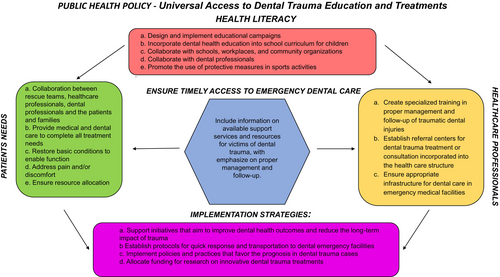
2.1 Health literacy
The design and implementation of educational public health policies to raise awareness about dental trauma involves a strategic approach to convey crucial information effectively. The strategies should define clear objectives, identify the target audience, and develop engaging content that emphasizes the causes of dental trauma and preventive measures. Utilizing diverse communication channels, such as social media, applications, community events, and collaboration with health professionals, is essential to maximize outreach.19, 31 The importance of addressing dental trauma promptly and effectively, lies in its potential to prevent long-term damage to teeth, improve overall well-being, and reduce healthcare costs associated with emergency treatments. By fostering awareness and promoting preventive measures, these policies contribute to a healthier community and underscore the significance of proactive oral health practices.
To ensure the success of educational programs on dental trauma, collaboration with key institutions and professionals is indispensable. By partnering with schools, workplaces, and community organizations, public health policies gain access to diverse audiences and channels for information dissemination.29 Schools provide a direct avenue to reach students and parents, instilling preventive measures from a young age. Workplaces offer the opportunity to engage adults who may overlook the importance of oral health in their busy lives. Community organizations provide a platform to connect with local residents, fostering a sense of shared responsibility for community well-being. Additionally, collaborating with healthcare professionals brings authoritative expertise to the forefront. Community workshops led by these experts will disseminate valuable information on preventive measures and also empower individuals with the knowledge needed to make informed decisions about their oral health.31 This collaborative approach will enhance the strategies' reach and ensure that the information is conveyed with credibility and relevance, contributing to a more informed and proactive community in addressing dental trauma.
The collaborative approach extends into the realm of preventive programs, adding depth to the overall strategy. By developing and implementing preventive dental health programs in schools and communities, the policies not only raise awareness but actively engage in proactive measures. Integrating dental health education into school curricula ensures a sustained and systematic approach to disseminating knowledge about oral health. By incorporating these programs into the educational system, the plan establishes a foundation for long-term behavioral change, empowering individuals to prioritize their dental well-being throughout their lives. These programs can include regular dental check-ups, oral hygiene education, sports dentistry, and protective measures, and the distribution of educational materials, fostering a culture of preventative care from a young age.
In addition to educational initiatives, promoting the use of protective measures during sports activities is a crucial facet of preventive efforts. Encouraging the adoption of mouthguards and other protective gear to reduce the risk of dental injuries and adopting a culture of precautionary measures within sports communities is of utmost importance.18, 26 Collaborating with sports organizations, schools, and community groups, policies can advocate for the widespread implementation of such measures, contributing to a safer environment for participants. Ultimately, these preventive programs reinforce the overarching message of the strategies, emphasizing the importance of proactive oral health practices and significantly reducing the incidence of dental trauma within schools and communities.
2.2 Patients' needs
Collaborating with healthcare providers is a key component of this strategy to meet the needs of patients suffering from dental trauma, as it enhances the immediate treatment options available to trauma victims.15, 36 By fostering partnerships with health and dental professionals as well as with emergency healthcare facilities, the plan should ensure that individuals facing dental trauma receive specialized care tailored to their needs. This collaboration can involve the development of specialized treatment plans, the provision of emergency dental services, and the dissemination of information about available resources. The proactive approach of collaborating with health care providers will address the acute needs of trauma victims and contribute to building a network of support that emphasizes the significance of prompt and specialized dental care in the aftermath of traumatic events. In summary, these measures collectively underscore the policy's commitment to comprehensive oral health and its dedication to minimizing the impact of dental trauma through swift and effective emergency response strategies.
The majority of patients affected by dental trauma suffer aesthetic and functional impairment of the oral cavity, accompanied by the presence of pain and/or physical, psychological, and social discomfort, due to injury of teeth, bone, or soft tissues. The range of dental trauma can be classified from enamel cracks to tooth avulsion.37 In most cases, tooth replantation, soft tissue suturing, tooth repositioning, dental splint, removal of tooth fragments, or pulp tissue protection are needed as first aid to ensure better support for the patient and an improved prognosis.8
Complete dental treatment can be highly complex and often requires an unexpected budget from the patient. For this reason, public health policy for dental trauma must have financial planning to support these patients, considering the importance of oral cavity rehabilitation in the patient's quality of life.
2.3 Healthcare professionals
Effective public health policies addressing dental trauma are imperative for ensuring a comprehensive and coordinated response to such incidents. First, the creation of specialized training programs represents a crucial step in equipping healthcare professionals with the necessary expertise for the proper management and follow-up of dental trauma cases. By incorporating focused education into the training curriculum for emergency responders, dentists, and other health care providers, these policies lay the groundwork for a more informed and skilled response to dental injuries, ultimately improving patient outcomes.
In addition to training, public health policies should advocate for the establishment of referral centers dedicated to dental trauma treatment or consultation. Integrating these centers into the broader healthcare structure facilitates seamless collaboration among various medical disciplines, ensuring a multidisciplinary approach to dental trauma cases. Such referral centers become hubs of specialized knowledge and resources, enhancing the overall quality of care provided to individuals experiencing dental trauma. Furthermore, policies should emphasize the need to ensure appropriate infrastructure for dental care within emergency medical facilities. This entails equipping emergency departments with the necessary tools, facilities, and personnel to address dental trauma promptly and effectively, recognizing the significance of oral health as an integral component of emergency medical care. Overall, these public health policies collectively contribute to a more resilient and responsive healthcare system, better equipped to handle and mitigate the impact of dental trauma on individuals' well-being.
2.4 Ensure timely access to emergency dental care
The importance of ensuring timely access to emergency dental care for trauma victims cannot be underestimated in the context of prevention and reduction of the consequences of dental trauma. Prompt intervention is critical to restoring basic conditions, enabling normal oral function, and reducing pain or discomfort associated with traumatic dental injuries. Public health policies should promote immediate access to emergency dental care, to minimize the physical and emotional toll on individuals but also to properly address the immediate consequences of dental trauma, promoting a faster and more effective recovery and prognosis.38 This involves establishing efficient protocols for quick response and transportation to dental emergency facilities, ensuring that individuals experiencing dental trauma receive prompt attention and appropriate care.22, 24, 39
2.5 Implementation strategies
Public health policies concerning dental trauma should prioritize research and development initiatives aimed at enhancing prognosis and reducing the long-term impact of such injuries.
According to the World Health Organization,33 public health refers to “all organized measures (whether public or private) to prevent disease, promote health, and prolong life among the population as a whole.” The absence of well-defined public health policies can lead to deficiencies in prevention strategies, proper treatment protocols, and the effective dissemination of essential information. This approach aims to mitigate the negative impacts of dental trauma and to lay solid foundations for oral health promotion.
Moreover, public policies should actively support initiatives dedicated to improving dental health outcomes and minimizing the long-term effects of trauma. This involves fostering collaborations between healthcare institutions, research organizations, and industry partners to develop comprehensive programs and interventions. These initiatives can include community outreach, education strategies, and preventive measures to address the root causes of dental trauma. The support, including financial support to the public health policies, plays a vital role in creating a healthcare landscape that is not only responsive to immediate trauma but is also committed to reducing the long-term impact, ultimately advancing overall dental health and well-being.
One key aspect is the allocation of funding for innovative dental trauma treatments. By earmarking resources for research endeavors, policymakers can foster the development of advanced diagnostic tools, treatment modalities, and preventive measures. This proactive investment supports the evolution of dental care, ensuring that practitioners have access to cutting-edge techniques that improve prognosis and mitigate the consequences of trauma.
3 CONCLUSIONS
In conclusion, the development and implementation of public health policies to address dental trauma through prevention programs, research, development, and support initiatives represents a significant step toward enhancing the well-being of the population and dental trauma victims' prognosis. By allocating funding for innovative treatments and technologies, policymakers enable advancements in dental care that improve prognosis and reduce the long-term impact of trauma. Additionally, supporting initiatives focused on improving dental health outcomes promote a proactive approach to preventive care, ultimately reducing the incidence of trauma and its associated consequences. Overall, these policies contribute to a more resilient healthcare system, ensuring that individuals have access to high-quality dental care that not only addresses immediate needs but also promotes long-term oral health and well-being for the entire population.
AUTHOR CONTRIBUTIONS
All the authors made substantial contributions to the manuscript. All the authors have read and approved the final version of the manuscript.
ACKNOWLEDGMENT
The authors would like to thank the Dean of Postgraduate Studies (PROPe-UNESP) for the Capes-Print Institutional Internationalization Program and the National Council for Scientific and Technological Development (CNPq, Brazil) for facilitating the international collaborative effort that led to this work.
FUNDING INFORMATION
No funding was received for the presented work.
CONFLICT OF INTEREST STATEMENT
The authors declare there are no competing interests for the above manuscript.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable as no new data were generated.