Immunosenescence: the importance of considering age in health and disease
OTHER ARTICLES PUBLISHED IN THIS REVIEW SERIES
The convergence of senescence and nutrient sensing during lymphocyte ageing. Clinical and Experimental Immunology 2017, 187: 4–5.
Immune senescence: significance of the stromal microenvironment. Clinical and Experimental Immunology 2017, 187: 6–15.
Innate immune responses in the ageing lung. Clinical and Experimental Immunology 2017, 187: 16–25.
Age-related alterations in immune responses to West Nile virus infection. Clinical and Experimental Immunology 2017, 187: 26–34.
Intracellular signalling pathways: targets to reverse immunosenescence. Clinical and Experimental Immunology 2017, 187: 35–43.
Ageing and inflammation in patients with HIV infection. Clinical and Experimental Immunology 2017, 187: 44–52.
Considerations for successful cancer immunotherapy in aged hosts. Clinical and Experimental Immunology 2017, 187: 53–63.
Ageing and obesity similarly impair antibody responses. Clinical and Experimental Immunology 2017, 187: 64–70.
The life cycle of a T cell after vaccination – where does immune ageing strike? Clinical and Experimental Immunology 2017, 187: 71–81.
Herpes zoster and the search for an effective vaccine. Clinical and Experimental Immunology 2017, 187: 82–92.
Adult vaccination against tetanus and diphtheria: the European perspective. Clinical and Experimental Immunology 2017, 187: 93–99.
This special issue of Clinical and Experimental Immunology is dedicated to immunosenescence. It covers a wide range of topics related to immunosenescence, from basic research and animal models to applied topics such as vaccines for elderly people and interventions to rejuvenate the immune system. The reviews in this issue highlight some of the topics discussed at the Satellite Symposium ‘Immunosenescence: Hot Topics and Interventions’, which took place on 5–6 September 2015 in Vienna, Austria, preceding the 4th European Congress of Immunology. The symposium was organized by Birgit Weinberger, Beatrix Grubeck-Loebenstein (both University of Innsbruck, Innsbruck, Austria), Daniela Frasca, Bonnie Blomberg (both University of Miami, Miami, FL, USA), Arne N. Akbar (University College London, London, UK), Graham Pawelec (University of Tübingen, Tübingen, Germany), Rebecca Fuldner (National Institute on Aging, Bethesda, ND, USA) and Elizabeth J. Kovacs (Loyola University, Chicago, IL, USA).
The world is undergoing a substantial shift in demographics, as the number of individuals aged more than 60 years is increasing dramatically. The immune system undergoes typical age-related changes, which are collectively termed ‘immunosenescence’. The incidence and severity of various infections increases with age; concomitantly, the immunogenicity and efficacy of many vaccines is lower in elderly people, making protection of this vulnerable population a challenge.
With increasing age, the innate immune system exhibits a diminished ability to respond to and clear infections. The incidence of lung infections is high in older adults and severe disease is observed frequently. A more detailed understanding of local and systemic immune responses to pneumonia and the impact of age is essential in order to design age-specific therapies. Alveolar macrophages and neutrophils are the first line of defence against bacterial pneumonia, but alterations in Toll-like receptor signalling, cytokine and chemokine production and defects in effector functions, such as clearance of cell debris and bactericidal activity, limit their effect in elderly people. Dendritic cells and natural killer cells in the lung play an important role in the defence against viral infections such as influenza and respiratory syncytial virus, but migration to lymph nodes and stimulation of T cells by dendritic cells as well as the capacity of natural killer cells to eliminate infected cells are diminished in old age 1.
Cell-intrinsic defects of aged T cells have been investigated extensively. The review by Kim et al. 2 summarizes the details of vaccine-induced T cell responses, including activation, expansion, differentiation into effector cells and generation of T cell memory, and highlights the importance of these findings for vaccine development. Most approaches to improve vaccination responses in old age concentrate on activating the innate immune system by adjuvants in order to improve the induction of an adaptive immune response, but strategies to target T cells directly should also be considered 2. During recent years it has become evident that metabolic regulation in lymphocytes plays an important role in immune responses and immune regulation. A short commentary by Arne Akbar highlights the interplay of nutrient sensing by adenosine 5'-monophosphate activated protein kinase (AMPK), intracellular adenosine triphosphate (ATP) levels and ageing processes in T cells 3. Age-related defects of B cells include alterations in the generation of B cells during haematopoiesis, reduced somatic hypermutation and class-switch recombination in germinal centre B cells and changes in the B cell receptor repertoire 4.
Our understanding of immunosenescence is, to a great extent, based on studies investigating the intrinsic properties and defects of individual immune cells. The importance of cell–cell interactions, for example between antigen-presenting cells and T cells or between T cells and B cells, are well recognized, as is the role of cytokines. There is also an important role for the microenvironment in immunosenescence, particularly within primary (bone marrow, thymus) and secondary (lymph node, spleen) lymphoid organs, where immune cells are generated, mature and reside and where adaptive immune responses are initiated. Aged stromal cells, altered cytokine environment and structural changes contribute to age-related changes in immune cell composition, activation and function 5.
Reversion of immunosenescence and rejuvenation of the immune system are promising strategies to improve health in old age. Fulop et al. 6 summarize age-associated alterations in the signalling pathways of immune cells, and discuss that signalling cascades can be promising targets to modulate immune function in old age. Protein tyrosine phosphatase inhibitors could be used to improve neutrophil function, but most studies focus on interventions targeting T cell signalling. Modulation of inhibitory receptors, such as programmed death 1 (PD-1) and of p38 MAPK pathways are investigated in order to restore T cell function. Inhibition of mammalian target of rapamycin (mTOR) has also been shown to improve immune function 6.
Besides the well-known examples of infections which are more frequent in elderly people, such as influenza, pneumonia, herpes zoster and skin infections, it has been shown that age might also be a risk factor for other infections that are not recognized commonly as age-related. Infection with West Nile virus is frequently asymptomatic, but some individuals develop severe neurological disease and encephalitis. Age is the most well-defined risk factor for severe disease and several age-related immunological defects, such as impairment of neutrophils, macrophages, dendritic cells and natural killer cells and altered Toll-like receptor function, might contribute to the increased susceptibility of older adults. Age-associated changes in the permeability of the blood–brain barrier might also be relevant 7.
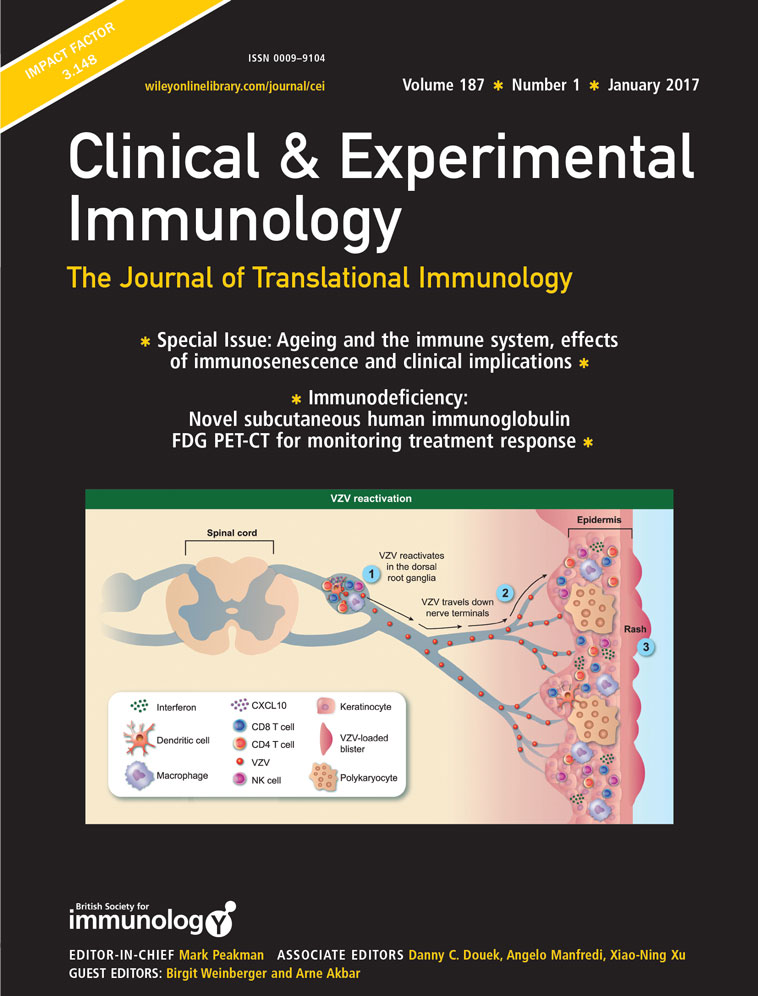
Vaccination is the most successful strategy to prevent infectious disease and several vaccines are recommended specifically for elderly people, including those against influenza, Streptococcus pneumoniae and herpes zoster. Arnold and Messaoudi summarize clinical and epidemiological data on varicella zoster virus infection and reactivation (herpes zoster) as well as immune responses at different stages of the viral life cycle 8. The licensed vaccine against herpes zoster, which is a live-attenuated vaccine, reduces the incidence of disease and the occurrence of post-herpetic neuralgia, a severe complication of herpes zoster. Recently, an adjuvanted subunit vaccine, which comprises the recombinant glycoprotein E in combination with the liposome-based AS01B adjuvant system (MPL and QS21), showed very promising results in a Phase III study 8. It has been demonstrated by a plethora of studies that antibody responses to influenza vaccination are lower in elderly people compared to younger adults. Frasca et al. 9 summarize that – similar to old age – obesity is associated with an increased inflammatory state, which hampers innate and adaptive immune responses. They also describe how intrinsic changes of B cells as well as altered microenvironment and inflammation lead to impaired antibody responses to influenza vaccination in aged and obese individuals 9.
In addition to the vaccines recommended specifically for elderly people, regular booster vaccinations against tetanus and diphtheria, which are recommended for all adults, are also relevant. The review by Birgit Weinberger gives an overview of vaccination recommendations, which differ between European countries, and vaccination coverage in adult populations 10. A substantial proportion of adults do not have protective antibody concentrations against diphtheria and antibody levels are even lower in elderly people. Despite an increase in antibody levels after booster vaccinations, long-term protection is frequently not achieved late in life, highlighting the importance of vaccination programmes throughout life 10.
With the increasing proportion of aged individuals worldwide, awareness is rising that immunological interventions and therapies should also consider the age of the patient. HIV-positive patients under efficient anti-viral therapy have an expected lifespan that is only slightly shorter than that of the general population. HIV infection leads to immunological changes that resemble immunosenescence in several aspects, including chronic inflammation and immune activation. The complex interplay of HIV pathology, adverse effects of long-term anti-viral treatment and the natural ageing process, which includes inflammatory processes, needs to be considered when treating older patients for HIV. Non-AIDS-related complications such as neurocognitive disorders, cardiovascular disease, metabolic syndrome and other typically age-associated diseases also need to be considered in this population 11.
Immunotherapy against cancer is experiencing a renaissance, as our understanding of cancer immunopathogenesis has increased substantially during recent years. Despite the fact that cancer incidence is increasing with age, age-related changes of the immune system are rarely taken into consideration when designing or testing novel cancer immunotherapies. Immune functions do not simply decline with age, but rather change in complex ways. Immune cell populations with undesired properties, such as cells producing proinflammatory cytokines or cells suppressing immune functions (e.g. myeloid-derived suppressor cells) can accumulate with age. Immunomodulatory drugs might affect aged immune cells in a distinct way, and the aged microenvironment is also contributing to altered immunological responses in old age. These factors need to be considered in the context of cancer immunotherapy for an aged population 12.
While this special edition of Clinical and Experimental Immunology covers many aspects of immunosenescence, many more factors need to be considered in the approach to improve health care in older adults with an ageing immune system. A profound and detailed knowledge of age-related changes of individual immune cells and pathways is the basis for the development of novel strategies to reverse or delay immunosenescence, which could prevent many age-related diseases. It is also the basis of vaccines targeting specifically the aged immune system in order to protect this vulnerable population. It is, however, crucial to keep in mind that the immune system is a highly complex network of cells and soluble factors. In addition, there is extensive cross-talk between immune cells and other tissues, and both environmental and behavioural factors, such as nutrition and exercise, also have an impact on the immune system. A strong and intact immune system is an essential part of healthy ageing and has the potential to improve quality of life substantially for elderly people.
Disclosure
None to declare.