Can open cholecystectomy be taught by cadaveric simulation?
Abstract
Background
Laparoscopic cholecystectomy (LC) is the current standard of treatment for surgical gallbladder removal as it has an overall improved post-operative recovery compared to Open Cholecystectomy (OC). This has resulted in the loss of exposure to surgical trainees and the associated technical skills and decision-making required to convert to OC. The aim of this study is to provide construct validity to the proposition that cadaveric simulation can be used successfully to teach and learn open cholecystectomy.
Methods
Participants (n = 25) were surveyed on a 9-point questionnaire using a 5-point Likert scale to determine their opinion on cadaveric simulation as a tool for teaching OC.
Results
Overall respondents deemed the tool as highly translatable. There was no significant correlation in the responses between candidates versus tutors (P = 0.05, r = 0.51).
Conclusions
The outcome of the survey revealed that participants agreed that cadaveric simulation is a positive learning tool to aid in OC.
Introduction
There has been a significant decline in elective and, less so, emergency open surgery due to the introduction of minimally invasive laparoscopic (key-hole) procedures.1, 2 As a result, foundational exposure and learning of open surgical techniques have been lost.1, 3 Traditionally, technical skills in operative surgery have been taught in the operating room under the direct supervision of surgeons, but the advent and popularization of laparoscopic procedures have diminished the exposure of surgical trainees to open operations.4 This is considered a problem for surgeons, particularly in regional centres, as they may be put in a position of having to do surgical procedures for which they are inadequately trained. The concerns arise specifically for cholecystectomy.3
LC for symptomatic cholelithiasis has become the widespread standard of care due to its association with decreased morbidity, shorter recovery time and overall cost reduction.3, 5 In Australia's private and public sectors, based on 2014–2015 data, the number of annual LC operations is given as 216/100000 per annum, whereas OC is 15/100000 people, including conversion rates of 1%–15%.2, 3, 5, 6 Thousands of patients thus have OC either primarily or following conversion, a source of risk for patients and surgeons.
The Halsted model of surgical training, with close apprenticeship, and repeated clinical practice, is ill-suited to the modern surgical context. The requirements of training programs to produce increased numbers of surgeons, given reduced working hours, decreasing numbers of expert trainers, and increasing litigation, puts patients, trainees, surgeons and hospitals at risk.4
Simulation in surgery has been widely used in teaching technical skills with validated simulation models.7 Simulation has been shown to improve technical performance, decrease errors, and shorten the learning curve in the operating theatre.8 The Anatomy of Surgical Exposure (ASE) course in Cairns run by James Cook University is a cadaveric simulation course in teaching whole-body open emergency and elective operations in General Surgery, in a simulated operating theatre environment. The first course was delivered in 2013 and was preceded by a careful assessment of needs of particularly regional surgeons. Sub-speciality emergencies in cardio-thoracic, neuro-surgical and urology procedures, were developed on the cadaveric model, and as well the perennial need for OC. Of the 21 h of the three-day program, 1.5 h are allocated to the OC segment.
Applications are invited on-line from doctors with an interest in surgical training. A minimal standard of Anatomy is required, the GSSE or an Anatomy Diploma. About half the candidates are those in Surgical Training, and occasionally some with FRACS. The tutors are evenly divided between local Cairns surgeons and an invited faculty from around Australia, Sri-Lanka and Singapore. This includes many Upper GI, Colorectal, Head and Neck, and Hepato-Biliary specialists.
Each of the 10 cadaver stations has a Registered Nurse, who in turn is supervised by an OT specialist RN, two candidates, one or two consultants, assisting medical students or paramedics, all fully gowned and gloved. Each table has a full set of instruments and safe handling taught and learned. Lighting and suction are provided. The candidates take it in turn to ‘do’ the operations, actively assisted by tutors. A separate team of trained data gatherers are in attendance to gather OSATS (Objective Structured Assessment of Technical Skills) scores for debriefing in addition to that for research (Document S2). A validation study of the ASE program was published in 2021.1
The specially prepared, flexible cadavers are supplied from mainly the JCU donation program in Townsville. They are expensive to prepare, transport and store. Costs are spread over other courses (Vascular, Arthroscopic, Orthopaedic, and Temporal Bone Dissection) using the same cadaveric material. This requires a great deal of Organization and Collaboration. The Smithfield facility and staff are excellent, as are the enthusiastic teams of volunteers (mainly medical students). Course income is almost entirely from candidates. None of the tutors are paid but have transport and accommodation provided by the ASE program.
Methods
The aim of this study is to provide construct validity to the proposition that cadaveric simulation in the ASE course can be used successfully to teach and learn OC.
This longitudinal study surveyed consenting participants, both candidates and tutors, who had performed and conducted the OC part of the program. The participants received an operational manual and access to pre-recorded videos where they were given instructions on how to perform the operation step-by-step (Document S1, Video S1). This included instructions for the primary operator, how to instruct the first assistant, and what instruments to use. For the purposes of the survey, the operation was broken down into several components after extensive discussions between general, upper gastrointestinal (GI) and hepatopancreatobiliary (HPB) surgeons and tested by the questionnaire (Fig. 1).
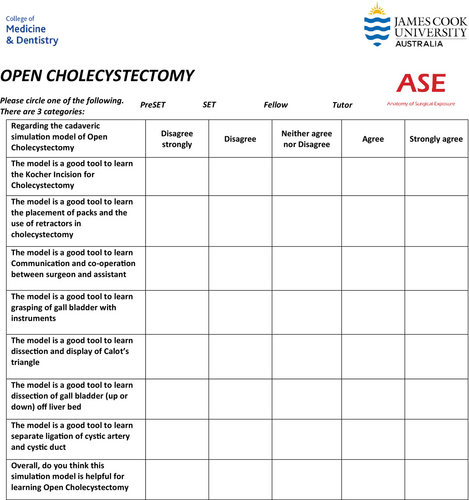
The survey contained 9 items, including 1 question on the level of training, and 8 questions regarding cadaveric simulation as a model for teaching open cholecystectomy using a 5-point Likert scale (Fig. 1). Categorical and Likert items are reported as number and per cent respectively. A Pearson chi-square test and Mann–Whitney U test (non-parametric test) were used to compare responses between candidates and tutors. A two-sided P-value <0.05 was considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics (Version 29).
Data gatherers recorded scores without interrupting work flow. The study was approved by James Cook University ethics committee (Ethics approval number H8855) and candidate consent was obtained.
Results
A total of 25 respondents participated in the survey between 12 October 2022 and 28 August 2023; 6 (24%) were junior doctors in pre-surgical training, 7 (28%) were surgical trainees, 10 (40%) were general surgery consultants, and 2 (8%) did not specify their level of training.
The five-point Likert scale is considered an interval scale. From 1 to 1.8, it means strongly disagree. From 1.81 to 2.60, it means disagree. From 2.61 to 3.40, it means neither agree nor disagree. From 3.41 to 4.20, it means agree; from 4.21 to 5, it means strongly agree. The overall responses are represented in Table 1. In this study, the decision using the perception of the respondents was based on a weighted average value or grand mean. The calculated weighted average value was 4.24. Therefore, anything that was less than 4.24 was deemed low perception and anything equal to or above, was deemed high perception (Table 1).9
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Mean | σ | Decision | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | F | % | F | % | ||||
| The model is a good tool to learn the Kocher incision for cholecystectomy | 14 | 56 | 11 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 4.56 | 0.507 | High perception |
| The model is a good tool to learn the placement of packs and the use of retractors in cholecystectomy | 8 | 32 | 12 | 48 | 4 | 16 | 1 | 4 | 0 | 0 | 4.08 | 0.812 | Low perception |
| The model is a good tool to learn communication and co-operation between surgeon and assistant | 10 | 40 | 11 | 44 | 4 | 16 | 0 | 0 | 0 | 0 | 4.24 | 0.723 | High perception |
| The model is a good tool to learn grasping of the gall bladder with instruments | 12 | 48 | 12 | 48 | 0 | 0 | 1 | 4 | 0 | 0 | 4.40 | 0.707 | High perception |
| The model is a good tool to learn dissection and display of Calot's triangle | 9 | 36 | 12 | 48 | 2 | 8 | 2 | 8 | 0 | 0 | 4.12 | 0.881 | Low perception |
| The model is a good tool to learn dissection of gall bladder (up or down) off liver bed | 9 | 36 | 14 | 56 | 1 | 4 | 1 | 4 | 0 | 0 | 4.24 | 0.723 | High perception |
| The model is a good tool to learn separate ligation of cystic artery and cystic duct | 8 | 32 | 9 | 36 | 6 | 24 | 2 | 8 | 0 | 0 | 3.92 | 0.954 | Low perception |
| Overall, do you think this simulation model is helpful for learning Open Cholecystectomy | 10 | 40 | 15 | 60 | 0 | 0 | 0 | 0 | 0 | 0 | 4.40 | 0.500 | High perception |
- Note: N = 25; F = frequencies; Weighted average (total means of all items/number of items) = 4.24.
The data analysis showed that most of the participants highly perceived that the model for OC was a good tool for learning the Kocher incision; communication and cooperation between surgeon and assistant; grasping of the gallbladder with instruments; dissection of the gallbladder (up or down) off the liver bed; and that overall, the simulation model was helpful for learning OC. On the other hand, the participants had a low perception of the model as a learning tool for placing packs, using retractors, dissection of Calot's triangle and separating ligation of cystic artery and cystic duct in OC.
When comparing the mean responses of candidates and tutors, there was no difference in responses in the two groups (P = 0.51). Therefore, the data suggests that the responses to the survey were not associated with the level of training.
Discussion
The most common reported intra-operative reasons for the conversion from LC to OC are difficult anatomy and dense adhesions, often both.3 Another reason is failure to progress laparoscopically and prolonged surgical time. It has been argued that there is a four times increased cumulative risk of perioperative complications of a LC that lasts over 2 h, than an open operation completed within 60 min.10 Validated Predictive Models for difficulty and conversion of LC to OC are available and should allow for planning of operating lists.2, 11-13
- Another chance to achieve a ‘Critical View’. This could be by manual palpation and retraction of the gall bladder and separation of the gall bladder from adhesions, by finger and blunt dissection. An important component is manual inferior retraction of the duodenum when adhesions are extensive.
- Fundus-first cholecystectomy in a hostile environment. While expert Laparoscopic surgeons may achieve this confidently, many general surgeons would feel more confident doing this open.
- Less-than Cholecystectomy-subtotal cholecystectomy especially in the presence of a stone impacted in Hartmann's Pouch may be much more easily and safely achieved by open operation. In this situation cholecystostomy after removal of an impacted stone may be better facilitated.14
- Where bleeding or injury to other organs has occurred in the context of ongoing difficulty, this is better done at an open procedure.
- Open exploration of the bile duct (though taught in this course), as a means to achieving cholecystectomy, is better deferred in this situation for later ERCP, unless there are other compelling indications.
The operator uses his hands and instruments differently and has a different perspective in OC. This should be taught and learned. When facing difficulty of this order, the advice and assistance of a senior colleague may be invaluable.
Campbell et al. surveyed 135 surgical trainees and new fellows on their exposure and confidence in performing both LC and OC. They found a significant difference in outcome in those respondents who had previously been involved in more than 20 OC, who felt confident to independently perform an OC or convert an LC to an OC. They found exposure to less than or more than 20 LC procedures had no impact on confidence in performing the OC procedure. Overall, it concluded that exposure to OC needs to be an important consideration in surgical training to develop confidence in performing OC.
If operative exposure is low for surgical trainees, and confidence in performing the operations is directly related to exposure, then further steps need to be taken to improve surgical exposure to ensure competent surgeons and patient safety. Surgical simulation models have been used as adjuncts to enhance performance in live operative settings, however, it is most established in areas of laparoscopy and endoscopy.15, 16 Current literature on open surgical simulators includes bench models, live animals, cadavers, and virtual reality surgical simulators with most of the studies focusing on trauma, vascular surgery, and technical skills. There is positive feedback from participants for open simulators, but limited research is available to assess the overall benefit and comparison of and between the models.15 The information on simulation models to teach open cholecystectomy is scarce and even more limited on cadaveric models.3
This observational study explored the opinions of respondents to cadaveric simulation as an opportunity for exposure and practice of OC. All participants of the study reported that overall, the model of cadaveric simulation was a helpful tool for learning OC. As shown in Table 1, 40% strongly agreed and 60% agreed with this statement. Specifically looking at the questionnaire, participants perceived that practice on a cadaver would be of considerable help in where to site their incision (using anatomical landmarks); have the ability to communicate with their first assistant and knowing where to technically place and use specific instruments; and finally, to be able to dissect the gallbladder off the liver bed. Interestingly there was a low perception on displaying and dissecting Calots triangle as well as the separation and ligation of the cystic artery and cystic duct based off the grand mean. For the dissection of Calots triangle responses to this section of the questionnaire reported 36% strongly agree, 48% agree, 8% neither agree or disagree, and 8% disagree. For learning how to separate and ligate cystic artery and duct, responses included 32% strongly agree, 36% agree, 24% neither agree nor disagree and 8% disagree. As this is a preliminary study, we did not explore the reasons prompting these responses.
The study limitations included a small sample size, some cadavers didn't have gallbladders (i.e previous cholecystectomy), and the cadaveric tissue was variable depending on past pathology. Further studies are planned to explore confidence levels pre and post-course, in the practice of OC.
Investigation of educational outcomes of simulation programs continue to develop, and this study may be usefully judged against the template of Kirkpatrick et al.17 and that of Zevin et al.8
The model of Kirkpatrick uses four levels of outcomes that may be investigated. The first level interrogates learners reactions to a curriculum. The second level interrogates whether some form of learning has been acquired; the third level interrogates whether participant behaviour has been changed by the program, and the fourth whether there have been improvement in outcomes. On this template this study may be judged Level 1.
The Delphi consensus methodology work of Zevin et al.,8, 18 while reviewing the subject, has produced a more surgically focussed template. This included pre-development analysis, cognitive psychomotor training, curriculum validation, evaluation and improvement, and maintenance of the model. While the ASE course has included pre-development analysis and has assumed psychomotor skills by selection and preparing of candidates, this is a preliminary step at curriculum validation. We have also been impressed over the years that this program has the potential to be used in a summative way. A preliminary validation study (Killoran et al.) suggests that this may be possible. More needs to be done.
Conclusion
Overall, the questionnaire revealed a positive response to cadaveric simulation model as a tool to teach open cholecystectomy. Currently there is little research, but this study opens the possibility for further investigation into this topic and the development of associated simulation models. This study provides validation to the notion that Open Cholecystectomy can be successfully taught by Cadaveric Simulation.
Author contributions
Callie Breanne Killoran: Data curation; formal analysis; investigation; project administration; writing – original draft; writing – review and editing. Alan de Costa: Methodology; supervision; writing – review and editing.
Acknowledgements
The Anatomy of Surgical Exposure (ASE) Course. James Cook University, Cairns and Townsville. The ASE course acknowledges the help of J&J. Open access publishing facilitated by James Cook University, as part of the Wiley - James Cook University agreement via the Council of Australian University Librarians.
Ethical approval
Ethical approval and consent to participate. The study was approved by James Cook University ethics committee (Ethics approval number H8855) and candidate consent was obtained.
Conflict of interest
None declared.