The roadmap for allergology in Europe: The subspecialty of allergology as “stop-over” on the way to a full specialty. An EAACI position statement
Abstract
The vision of European Academy of Allergy and Clinical Immunology (EAACI) and the Union of European Medical Specialists Section and Board on allergology is to promote and to establish a full specialty of allergology in all European countries. In many European countries, a full specialty does not exist. In those countries, organ-based (sub)specialists or paediatricians and internists with an expertise in allergology may deliver allergy care. There are no generally accepted requirements for the training of subspecialists available. To fill the gap between the need and availability of experienced and accredited physicians who can deliver optimal care to the allergic patients, the EAACI Specialty Committee proposes the minimal requirements for training and certification of subspecialists in allergology. This paper describes the required theoretical knowledge, skills, competences and training facilities (staff and institution). The subspecialist as described in this paper should ideally show the necessary competence in providing good quality care to patients in an environment lacking those full specialists in allergology or tertiary care paediatric subspecialists in allergy.
Abstract

1 INTRODUCTION
The prevalence of allergic diseases is high with allergic rhinitis ranging from 17% to 29% in Europe,1 and asthma fluctuating from 1.3% to 11% in European surveys among children and adults.2 Increasing trends are also recorded in childhood and allergic rhinoconjunctivitis and asthma affects up to 20% of children worldwide.3, 4 In the UK, from 1990 to 2004, hospital admissions for anaphylaxis have increased by 700%, for food allergy by 500%, for urticaria by 100%, and for angio-oedema by 40%.5
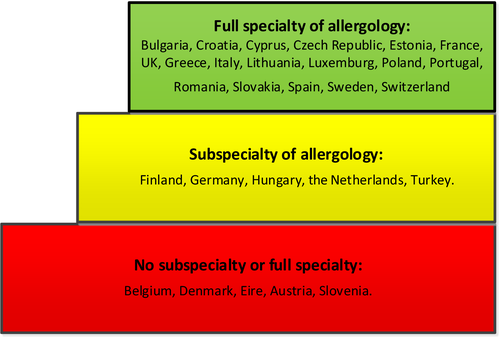
The high burden of allergic diseases imposes substantial demand on health care services. The vision of the European Academy of Allergy and Clinical Immunology (EAACI) and the Union of European Medical Specialists (UEMS) Section and Board (S&B) on allergology is to promote and to establish full specialties of allergology in all European countries. However, allergology is recognized as a full specialty in only 12 (data from 20136) and as subspecialty in six European countries. Some countries do not recognize at all specialists with expertise in allergy. There is an obvious gap between the need and availability of experienced and accredited physicians who can deliver optimal care to the allergic patients. In those countries, where no full specialty in allergology exists, organ-based (sub)specialists or paediatricians and internists with an expertise in allergology may cover allergy care. The different medical systems across Europe do not always stipulate for well-delineated care and training curricula in allergology, and consequently, physicians with different backgrounds, internists, paediatricians or organ-based specialists with an interest in the field should receive specific training in allergy and/or immunology to fill up the gap. Although the minimal requirements for the training of a full specialist have been described in the Logbook and Core curriculum of allergology,7 there are no generally accepted requirements for subspecialists available. Consequently, there is a need to harmonize the education and training for such subspecialists across Europe. This subspecialist is not meant to replace the full specialist, but to provide adequate services. Moreover, the institution of subspecialists should pave the way towards the full specialty, recognized in all European countries. One example is France, which started with allergology as a competence for general practitioners, subsequently instituted a subspecialty and finally established apart from the subspecialty the full specialty in allergology in 2017.
This paper aimed to propose the minimal requirements for training and certification of subspecialists in allergology.
2 METHODS
This consensus document was prepared by the EAACI Specialty Committee. Contributors were Roy Gerth van Wijk (chair) and Norbert Muelleneisen (secretary), both representatives of the UEMS S&B, Jacques Gayraud and Ted Popov representing the European Committee of Continuous Education for Allergologist Practitioners (CEFCAP), Ibon Equiluz-Gracia, Jan Gutermuth, Eckhard Hamelmann, Enrico Heffler, Peter Schmidt-Grendelmeier, Peter Valentin Tomazic, Olympia Tsilochistrou representing EAACI. In January 2016, the EAACI Specialty Committee and a representative of the EAACI National Societies Council met in Zurich to discuss and draft the paper setting minimal requirements for a subspecialist in allergology. The committee convened on 8 January 2016, 10 June 2016 and 3 February 2017 to prepare and finalize the paper.
3 GENERAL ASPECTS OF THE SUBSPECIALTY OF ALLERGOLOGY
Allergology, unlike other medical specialties, does not deal with single-organ/system diseases, but it applies by definition to systemic diseases. Therefore, a systemic approach to allergic diseases has to be the major component of education and training of residents in allergology subspecialty. Allergology either full or subspecialty deals with allergic diseases and involves the diagnosis and comprehensive management of disease while it is strongly related to basic and/or clinical research. This subspecialty programme of EAACI aimed to guide fellows towards the training programme to become medical experts and professionals in the allergy field.8 This programme may offer national authorities a framework to ensure a standard of qualifications of the allergy subspecialists as well as their unrestricted move for training across Europe. We believe that organ specialists involving systems where allergic mechanisms originate and/or take place (eg dermatologists, ENT or respiratory physicians), and those with a systemic approach and management of diseases such as internal medicine doctors and paediatricians should be given the opportunity to obtain dedicated training in order to receive accreditation as subspecialists in allergology. The training in the subspecialty should be focused on competences and skills applicable for all allergy fellows, but these competences and skills can be tailored to the different full specialties. The theoretical background knowledge should be identical for all fellows. EAACI organizes annually the EAACI/UEMS Knowledge Exam in allergology and it is highly desired that this accreditation becomes accepted by national authorities across Europe to certify skills in allergology.
The duration of training must be commensurate with the complexity and variety of topics which will be dealt with both in their theoretical background and in practical settings. Therefore, we believe that a minimum duration of 18 months is required to capture the basic aspects of the subspecialty. This training may not provide the broad spectrum of knowledge and skills as described in the core curriculum of the full specialist in allergology.
The requirements for the proposed paediatric subspecialty are not comparable with the already existing demands for paediatricians trained as tertiary care specialists with the capacity for independent practice (2-3 years of training after common trunk). This training has been described in the European Syllabus in Paediatric Allergology as approved by the European Board of Paediatrics and UEMS9 and published on the EAACI website.10 The subspecialist as described in this paper should be competent to provide good care to patients in an environment lacking those full specialists or tertiary care paediatric subspecialists. We also did not touch clinical immunology. Clinical immunology in Europe is predominantly covered by internists, rheumatologists and allergologists with a combined specialty of allergology and clinical immunology.
3.1 Theoretical knowledge
Fellows successfully taking the EAACI/UEMS Knowledge Exam have the theoretical knowledge of allergy/immunology topics as described in the related catalogue which is proposed to the participants of the Exams (sixth version, 2/2013).11 The topics are listed in Table 1. However, passing the EAACI/UEMS Exam is not yet a prerequisite for registration as either a subspecialist or full specialist in allergology, with the exception of a few countries that have allergology as a full specialty (Switzerland, Sweden and Lithuania). This examination must be considered as an excellent tool to test one's theoretical knowledge in the field of allergology and clinical immunology. EAACI is currently in the progress of organizing a dedicated module of the examination which will address the paediatric allergy field, and as such, it is expected to represent a highly esteemed certification for paediatric allergists.
| 1. Basics/epidemiology allergology/immunology |
| 1.1. Basic principles of immune response |
| 1.2 Epidemiology/genetics |
| 1.3 Allergens |
| 2. Clinic, diagnosis and therapy of allergic diseases |
| 2.1 Allergic diseases: allergic respiratory diseases, allergic skin diseases, food hypersensitivity, drug hypersensitivity, insect venom allergies, anaphylaxis as a consequence of these diseases, mastocytosis or mast cell-related diseases, diseases with hypereosinophilia, controversial symptoms |
| 2.2 Diagnosis of allergic diseases |
| 2.3 Therapy |
| 3. Clinical immunology |
| Basic knowledge of: |
| 3.1 Immune deficiencies (primary and secondary) |
| 3.2. Autoimmunity |
| 4. Appendix |
| Characterization and occurrence of individual allergens |
| Seasonal inhalation allergens |
| Perennial inhalation allergens |
| Occupational inhalation allergens |
| Food allergens (for children and adults) |
| Contact allergens |
| Lipid transfer protein, profilin, bet v1 families, etc., and other cross-reactivity clusters |
| Agents inducing drug hypersensitivity |
| Pseudo-allergy |
| Research principles |
3.2 Skills
Allergic disorders are systemic in nature and have a broad spectrum of organ manifestations. Taking this into account, an acceptable level of competence is required for all physicians who take care of allergic patients but who are not allergy specialists.12 This competence should encompass theoretical knowledge and practical skills.
Table 2 gives an overview of skills for all subspecialists and skills tailored to the different backgrounds of specialists.
3.3 Competences
The essential competences of physicians for optimal care are thoroughly defined in the CanMEDS framework8 (ie medical expert, communicator, collaborator, leader, health advocate, scholar and professional) and should apply for all physicians at all disciplines and hence to allergy specialists and subspecialists. Professional competence is developmental, impermanent and context-dependent.13
- A cognitive function: acquiring and using knowledge to solve real-life problems.
- A relational function: communicating effectively with patients and colleagues.
- An affective function: willingness, patience and awareness to use knowledge and skills to serve the patient.
Upon completion of training, fellows are expected to be competent subspecialists in allergology capable of assuming a consultant's role. For this reason, they must have developed efficient communication skills, fundamental knowledge, technical skills, clinical reasoning and appropriate attitude for professional patient-centred service and care.
Allergology is a multidimensional and interdisciplinary specialty. Training should thus always include treatment of children and adults with a focus on children in paediatric and adults in adult allergology programmes, and of the specific medical aspects of allergic diseases. Still, the allergy subspecialist may have a focus on the management of allergic diseases that are related to his/her primary specialty. Therefore, besides general competences in allergy, specific competences are required for the different subspecialists in allergology. The list of competences represents minimal requirements and is therefore not extensive; moreover, the list partly overlaps with the general competences for organ-based specialists.
All these aspects are detailed as follows:
3.3.1 General competences
The competent subspecialist in allergology is able to:
-
Acquire and apply knowledge:
- Understand the pathology and mechanisms of allergic disease.
- Apply this knowledge to real patient situations.
- Recognize weaknesses in his/her own knowledge and skills.
- Use various systems and tools to acquire new knowledge by asking, learning, communicating, searching.
- Solve daily and general problems in patient care and management.
- Communicate with patients and colleagues.
-
Acquire and apply technical skills (see Table
1
)
- Physical examination skills.
- Procedural skills.
-
Integrate knowledge and skills (see Table
1
)
- Use clinical reasoning strategies.
- Integrate knowledge of external (allergic) causes with history taking and assessment of sensitization.
- Link basic and clinical knowledge across the disciplines of allergology (paediatrics/ENT/pneumology, dermatology).
-
Take care of the patients
- Respect the patient's needs and worries.
- Tolerate different gender, religion and ethical and social backgrounds.
- Apply emotional intelligence.
- Provide the best clinical result for the individual patient regardless of treatment duration.
3.3.2 Specific competences
-
The competent paediatrician subspecialized in allergology is able to:
- Understand the development and mechanisms of allergic diseases in childhood and adolescence.
- Understand the concept and limitation of the “united airway, allergic march” or the currently debated term “one organ, one disease.”
- Communicate with young allergic patients and their parents/caretakers.
- Examine infants, toddlers and school-age children.
- Educate children and caretakers on the risk and management of anaphylactic reactions/shock.
- Educate children and caretakers on the basics and management of atopic eczema/dermatitis.
- Educate children and caretakers on the basics and application of inhalation (including nebulizer, MDI, DPI and spacer).
- Diagnose and treat patients with food allergy.
- Understand the concept and apply the means of primary and secondary prevention of allergy and asthma.
- Understand and translate the risk and benefit of anti-allergic therapies (allergen avoidance, pharmacotherapy, allergen immunotherapy).
-
The competent dermatologist subspecialized in allergology is able to:
- Understand the development and mechanisms of allergic diseases in the skin.
- Understand the concept of impaired skin barrier function as a risk for allergies.
- Educate patients on the basics and management of atopic eczema/dermatitis.
- Educate patients on the basics and management of contact allergies.
- Educate patients on the basics and management of urticaria and angioedema of various origin.
- Educate patients on the risk and management of anaphylactic reactions/shock.
- Understand and translate the risk and benefit of anti-allergic therapies (allergen avoidance, pharmacotherapy, allergen immunotherapy).
- Manage cutaneous manifestations of drug hypersensitivity.
- Diagnose and treat patients with food allergy.
- Educate patients on the risk and management of anaphylactic reactions/shock.
-
The competent ENT doctor subspecialized in allergology is able to:
- Understand the development and mechanisms of allergic diseases of the upper airways.
- Understand the concept and limitation of the “united airways, allergic march” or the currently debated term “one organ, one disease.”
- Educate patients on the risk and management of anaphylactic reactions/shock.
- Educate patients on the basics and application of inhalation (including spacer, MDI, nebulizer).
- Understand the concept and apply the means of secondary prevention of asthma in rhinitis patients.
- Understand and translate the risk and benefit of anti-allergic therapies (allergen avoidance, pharmacotherapy, allergen immunotherapy).
- Educate patients on the risk and management of anaphylactic reactions/shock.
-
The competent respiratory physician subspecialized in allergology is able to:
- Understand the development and mechanisms of allergic diseases of the lower airways.
- Understand the concept and limitation of the “united airways, allergic march” or the currently debated term “one organ, one disease.”
- Educate patients on the risk and management of anaphylactic reactions/shock.
- Educate patients on the basics and application of inhalation (including spacer, MDI, nebulizer).
- Understand the concept and apply the means of secondary prevention of asthma in rhinitis patients.
- Understand and translate the risk and benefit of anti-allergic therapies (allergen avoidance, pharmacotherapy, allergen immunotherapy).
- Educate patients on the risk and management of anaphylactic reactions/shock.
-
The competent internist subspecialized in allergology is able to:
- Understand allergies as a systemic disease.
- Apply this knowledge to real patient situations.
- Understand the concept and apply the means of secondary prevention of asthma in rhinitis patients.
- Understand and translate the risk and benefit of anti-allergic therapies (allergen avoidance, pharmacotherapy, allergen immunotherapy).
- Diagnose and treat patients with food allergy.
- Diagnose and treat patients with insect allergy.
- Diagnose and treat patients with drug allergy.
- Educate patients on the risk and management of anaphylactic reactions/shock.
3.3.3 Training requirements
In countries where allergology has not attained recognition as a full specialty, training programmes should be instituted to address a wide range of skills, knowledge and competencies to allow adequate care for patients with allergic diseases. The aim was to achieve at least the minimal standards which should be periodically updated in line with the most current medical literature, practice-changing innovations and the needs of the population served. At a national level, these training programmes need to be accredited. International/European guidelines and position papers should provide basis for harmonization across the countries. The duration of the training should ideally involve at least 18 months of allergy training apart from the training within the context of the main (organ) specialty.
- The guiding factor in the development of a programme should be that it will benefit both patients and physicians.
- The programme should contain a didactic element; the process to implement it needs to be a learning experience ending with an examination, which demonstrates increased medical knowledge.
- Multiple sources of information are necessary in line with the diversity of allergology as a specific medical discipline.
- Multiple assessment tools are necessary including logbooks, testing of knowledge, practice assessment, analysis of patient care outcomes and quality improvement.
- The training needs to be flexible and adaptable to changes in medicine, science and the practice of allergy and clinical immunology, and it should recognize local needs, availability of medications and diagnostic tests, and service capabilities.
- Outcomes should be identified from the beginning and be monitored and quantified to verify that the process is beneficial.
3.3.4 Staff and institution
Trainers for allergology need to be either fully licensed allergists or need to be board-certified in one of the basic specialties (internal medicine, paediatrics, ENT, dermatology, pneumology) and need to have a subspecialty certification, depending on the national legislative situation. Two years of professional experience is necessary to serve as a supervisor for a trainee in allergology. The director of training program in allergology in particular institution is required to have 5 years of relevant experience in training of residents.
Every 2 years, all staff members providing patient care should be trained and certified in basic life support. Nurses, dieticians and other health allies working in the facility need to be specifically trained to deal with allergic patients.
- Access to a library:
- ○ With relevant textbooks for specialty students.
- ○ Minimum online access to relevant medical and scientific journals covering allergology, the organ specialties and general medicine.
- ○ A quiet space for retreat to check the literature.
- Clinical unit to perform
- ○ Skin prick testing, intradermal testing.
- ○ Patch testing and advanced experimental methods (atopy patch).
- ○ Nasal provocation.
- ○ Conjunctival provocation.
- ○ Spirometry, bronchial challenge.
- ○ Oral food challenge, drug challenge.
- ○ Allergen immunotherapy.
- ○ Monitoring, access to emergency care (incl. life support)/acute treatment of anaphylaxis.
- ○ Dietary counselling/intervention.
- A laboratory to perform basic and advanced testing relevant to allergology:
- ○ Haematology, clinical chemistry.
- ○ Total and specific IgE testing, component-resolved diagnosis.
- ○ Additional experimental testing as basophil activation tests (flow cytometry) and lymphocyte transformation test.
- Facilities for multidisciplinary case discussions
- The spatial prerequisites for registering an allergy training centre:
- ○ Presence of consultation rooms, material and devices to perform the necessary clinical investigation, technical, serological and cellular tests as outlined above (training centres can be registered for selected competencies, for example, dermatology-related competencies of the subspecialty).
- ○ Defined number of patient contacts in the training centre depending on the number of staff and fellows in training (3000-6000/year based on consensus between committee members).
- ○ In training centres, a programme director with 5 years of relevant experience, teach-the-teacher trained.
- ○ At least 2 supervisors should be available to guarantee the continuity of the training.
- ○ Per two residents, one full-time supervisor with at least 2 years of experience should be part of the team.
3.3.5 Registration & revalidation
-
Registration (licensing) of an allergist/subspecialist
- ○ Passing relevant national board examinations (primary specialty, followed by allergology examination after at least 18 months of allergology training).
- ○ National board examinations need to be aligned with the UEMS/EAACI learning objectives, as the European citizens are moving across the continent.
- Revalidation/accreditation of the subspecialty holder needs to be kept active by regular monitoring of the educational status and clinical activity (1- to 5-year cycles):
- ○ Subspecialists aiming for accreditation should gain a predefined number of 120 CME points per 3 years, 84 from the field of allergology and at least 36 from fields of personal choice, thus on average 40 points annually.
- ○ A clinical activity of at least two clinical working days (16 hours) for 40 weeks within 1 year.
- ○ Any other requirements depend on national regulations. For instance, in the Netherlands a visitation of clinical practices by the national allergy society is a prerequisite for reregistration.
4 PERSPECTIVES: THE ROAD TO THE FULL SPECIALTY
In terms of allergy services and allergy care, Europe is characterized by substantial heterogeneity (Figure 1). As stated in the blue print,6 quality criteria in allergy health care comprise the availability of physicians trained in allergy who are able to perform a comprehensive medical allergy history and physical examination. Patients expect safe and adequate allergy testing, optimal preventive advice and treatment and a doctor who is a good communicator in counselling and education. The key person in allergy health care should be the full specialist interacting with general practitioners, occupational health physicians, general and organ-based specialists. Ideally such care should be delivered by an allergy centre, staffed by allergists and supported by appropriately trained allied health professionals. EAACI takes the position that this level of allergy care should be achieved in every European country.
However, also in countries lacking the full specialty of allergology, patients are entitled to have access to the best possible allergy service. Subspecialists can meet the needs of these patients provided that they are competent in diagnosing and treatment of these patients. In the absence of well-defined and well-accepted criteria for the training of such subspecialists, this paper aimed to give guidance regarding the (1) minimal requirements for the disciplines and countries that would like to establish subspecialties in allergology and (2) common criteria for existing subspecialties as well. Without a leading or coordinating allergist, such subspecialists with different backgrounds need to cooperate, share competences and speak a common language. Harmonization in training is the only way to achieve that.
For several European countries like Switzerland and France, subspecialties were the starting point for establishing full specialties. Some other countries are far away from the full specialty. Development of recognizable subspecialties in allergology may be the first step in these countries.
The subspecialties proposed in this document do not have a formal status at the UEMS level which is reserved for the full specialty of allergology as all subspecialists are already part of a recognized specialty. Developing competing specialties is not the aim and the ultimate goal is to set general standards for all specialists dealing with allergic patients.
DISCLAIMER
We unconditionally support allergology as a full speciality in every country of the world. This position paper is however outlining the optimal circumstances related to the organization of training of subspecialists in allergology. It is meant to help countries, where allergology is not recognized as a full specialty, to set up surrogate health care in the field. It is not intended as a legal/mandatory document.
FUNDING
This work was funded by the European Academy of Allergy and Clinical Immunology (EAACI).
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.