Deceased donor kidneys are discarded at higher rates when labeled as high kidney donor profile index
Abstract
The kidney donor risk index (KDRI) and percentile conversion, kidney donor profile index (KDPI), provide a continuous measure of donor quality. Kidneys with a KDPI >85% (KDPI85) are referred to as “high KDPI.” The KDPI85 cutoff changes every year, impacting which kidneys are labeled as KDPIHIGH. We examine kidney utilization around the KDPI85 cutoff and explore the “high KDPI” labeling effect. KDRI to KDPI Mapping Tables from 2012 to 2020 were used to determine the yearly KDRI85 value. Organ Procurement and Transplantation Network data was used to calculate discard rates and model organ use. KDRI85 varied between 1.768 and 1.888. In a multivariable analysis, kidney utilization was lower for KDPI 86% compared with KDPI 85% kidneys (p = .046). Kidneys with a KDRI between 1.785–1.849 were classified as KDPIHIGH in the years 2015–2017 and KDPILOW in the years 2018–2020. The discard rate was 44.9% when labeled as KDPIHIGH and 39.1% when labeled as KDPILOW (p < .01). For kidneys with the same KDRI, the high KDPI label is associated with increased discard. We should reconsider the appropriateness of the “high KDPI” label.
Abbreviations
-
- DCD
-
- donation after cardiac death
-
- HCV
-
- hepatitis C virus
-
- KAS
-
- kidney allocation system
-
- KDPI
-
- kidney donor profile index
-
- KDPI85
-
- 85th percentile kidney donor profile index
-
- KDPIHIGH
-
- kidney donor profile index >85%
-
- KDPILOW
-
- kidney donor profile index <85%
-
- KDRI
-
- kidney donor risk index
-
- KDRI85
-
- 85th percentile kidney donor risk index
-
- KDRIRAO
-
- kidney donor risk index (defined by Rao)
-
- OPTN
-
- Organ Procurement and Transplantation Network
-
- SRTR
-
- Scientific Registry of Transplant Recipients
1 INTRODUCTION
In 2014, the Organ Procurement and Transplantation Network (OPTN) introduced the new kidney allocation system (KAS) that allocates kidneys based on a quantification of kidney donor quality and longevity matching.1 The kidney donor risk index (KDRI) and its percentile conversion, the kidney donor profile index (KDPI) were introduced with the KAS to provide a continuous measure of kidney donor quality.2 With KDPI, kidneys are scored from 0 to 100%, with low percentile scores reflecting better donor kidney quality. Under KAS, the best quintile of kidneys (≤20% KDPI) are allocated to recipients with the best-predicted survival benefit, that is, patients with the best estimated post-transplant survival scores.3 In contrast, kidneys with a KDPI >85% (KDPI85) require additional informed consent from the recipient due to decreased kidney longevity,4 and are colloquially referred to as “high KDPI kidneys.”
In order to calculate a deceased donor's KDPI, several steps are taken. First, 10 donor factors are used to calculate the KDRIRAO,2 which is the raw score. Next, the KDRIRAO is divided by the median KDRI value of the previous year's kidneys procured for transplant. This median KDRI is also termed the “scaling factor” and allows one to use the scaled KDRI as a measure of the relative graft failure rate compared with the median donor. The scaled KDRI value is then mapped to its corresponding KDPI percentile using the KDRI-to-KDPI mapping table that is updated annually. As the distribution of procured kidneys changes every year, the median KDRI scaling factor and all the percentile cutoffs also change. The 85th percentile KDRI (KDRI85) and the KDPI85 refer to the upper limit of what would be considered a “standard” kidney, and above which kidneys are classified “high KDPI.”
This study aims to examine changes in the KDRI85 for procured kidneys over time, determine kidney utilization around the KDPI85 cutoff and explore if there is a “high KDPI” labeling effect. We hypothesize that kidneys with the same KDRI would have different utilization when their KDRI places them above or below the KDPI85 cutoff.
2 MATERIALS AND METHODS
We conducted a retrospective analysis of all United States kidney donors with kidneys recovered for the purpose of transplantation in the OPTN database from January 1, 2012 to December 31, 2020. The time frame for the study was chosen based on initial reporting of the KDPI in organ offers in 2012, and subsequent implementation of the KAS and utilization of KDPI for organ allocation on December 4, 2014. KDRI to KDPI mapping tables from 2012 to 2020 were used to identify KDPI cutoffs and scaling factors.5 The data for this analysis is OPTN data released on April 01, 2021 and UNOS as the contractor for the OPTN supplied the data. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation by the OPTN or the US Government. The University of Washington Human Subjects Division deems the OPTN database to be de-identified and publicly available and thus, not human subjects' data. Therefore, this study was exempt from human subject review.
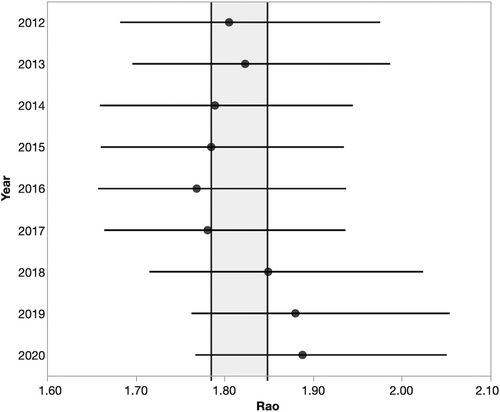
The KDRI to KDPI mapping tables were used to identify the highest scaled KDRI value for a KDPI 85% kidney for 2012–2020. The scaling factor for each year was then used to calculate the raw KDRI85 (KDPI x scaling factor = KDRI).5 Evaluation of change in the KDRI85 over time was performed using the one-way Anova test. In order to examine how KDPI classification changed over time, we took the maximum scaled KDRI85 kidney from each year, calculated the raw KDRI85 using the corresponding year's scaling factor, and then recalculated the KDPI85 for all other years using the relevant scaling factors and mapping tables.
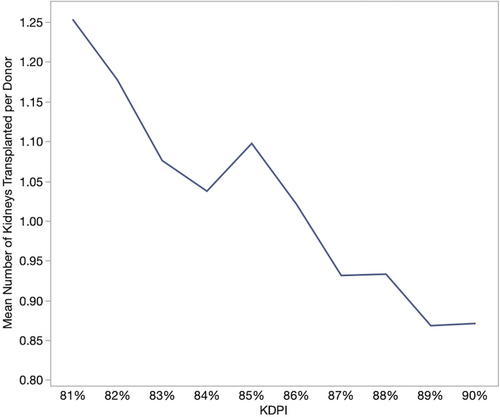
To examine the impact of KDPI on kidney utilization around the 85th percentile, we performed a multivariable linear regression of the number of kidneys transplanted for all potential kidney donors with a KDRI between 81% and 90% in the years 2015 through 2020 (i.e., after KAS implementation). Donors could have 0, 1, or 2 kidneys transplanted. Variables in the model include each of the 10 factors including the KDPI calculation, a time variable (“year from 2015”) to look for a temporal effect on acceptance practices, and variables for each KDPI (with KDPI 85% as the reference).
To determine if there was a high KDPI labeling effect, we examined a narrow KDRIRAO range that fell between the highest KDRI85 of 2015–2017, and the lowest KDRI85 of 2018–2020. These kidneys were above the KDRI85 cutoff in 2015–2017, and such were designated KDPIHIGH, but were below the KDRI85 cutoff in 2018–2020 and so were designated KDPILOW. The number of kidneys procured, discard rate, number of kidney transplants per donor, and biopsy status were examined from this narrow KDRI range by KDPIHIGH versus KDPILOW status. For this population, we then examined differences in the 10 variables included in KDPI, by KDPI status (KDPIHIGH vs KDPILOW).
3 RESULTS
Between 2012 and 2020, the KDRI85 ranged from 1.768 to 1.888 but was not statistically different (p = .49, Table 1). To examine how KDPI classification changed over time, we compared the highest KDPI85 kidney from each year and mapped it to all other years (Table 2). There is substantial variation in the assigned KDPI to a kidney based on the mapping table for each year, between 80% and 89%. For example, a kidney recovered in 2016 with a KDPI of 85% would have been reported as a KDPI 80% kidney in 2019. Likewise, a KDPI 85% kidney recovered in 2020 would have been reported as a KDPI 89% kidney in 2014.
| Year | Scaled KDPI_85 | Scaling factor | KDRI_85 |
|---|---|---|---|
| 2012 | 1.476586686 | 1.222192123 | 1.804672618 |
| 2013 | 1.491034239 | 1.223395269 | 1.824124234 |
| 2014 | 1.463399275 | 1.221769234 | 1.787936211 |
| 2015 | 1.466165369 | 1.217500516 | 1.785057094 |
| 2016 | 1.465406965 | 1.206598211 | 1.768157422 |
| 2017 | 1.470735771 | 1.210831362 | 1.780812997 |
| 2018 | 1.478310675 | 1.250695754 | 1.848916885 |
| 2019 | 1.457436689 | 1.289910453 | 1.87996282 |
| 2020 | 1.467536634 | 1.286540715 | 1.888045631 |
| A 85% KDPI kidney recovered in | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | ||
| Mapped onto the table from | 2012 | 86% | 85% | 85% | 84% | 85% | 87% | 88% | 88% | |
| 2013 | 85% | 84% | 84% | 83% | 84% | 86% | 88% | 88% | ||
| 2014 | 86% | 87% | 85% | 85% | 85% | 88% | 89% | 89% | ||
| 2015 | 86% | 87% | 86% | 85% | 85% | 88% | 89% | 89% | ||
| 2016 | 87% | 87% | 86% | 86% | 86% | 88% | 89% | 89% | ||
| 2017 | 86% | 87% | 86% | 86% | 85% | 88% | 89% | 89% | ||
| 2018 | 84% | 85% | 83% | 83% | 83% | 83% | 87% | 87% | ||
| 2019 | 82% | 83% | 81% | 81% | 80% | 81% | 84% | 85% | ||
| 2020 | 83% | 83% | 82% | 82% | 81% | 82% | 84% | 86% | ||
- Note: Red shading indicates KDPI greater than 85th percentile, and green shading indicates less than 85th percentile. The KDRI_Rao of a KDPI 85% kidney from the year represented in the column was calculated and located on the mapping table of the row year to calculate the KDPI for that year.
The mean number of kidneys transplanted per donor by KDPI is shown in Figure 1 and demonstrates a decreased utilization with increasing KDPI. In the multivariable linear regression model, we found significantly lower utilization of KDPI 86% kidneys compared with KDPI 85% (p = .046, Table 3), while there was no difference found between KDPI 83% or 84% kidneys versus KDPI 85% (p = .74 and 0.25, respectively). Other factors associated with decreased kidney use include higher creatinine, donor height, and anoxia as a cause of death. Donor age and Asian, Black, or Hispanic race were associated with increased kidney usage. Notably, there were no differences for year, donor hepatitis C virus (HCV) status, or donation after cardiac death (DCD) status.
| Donor factors | Estimate | Standard error | p |
|---|---|---|---|
| Age | 0.164592 | 0.002083 | <.001 |
| Height | −0.008998 | 0.00126 | <.001 |
| Weight | −0.000161 | 0.000518 | .75 |
| Ethnicity | |||
| White | ref | ||
| Asian | 0.2508076 | 0.061024 | <.001 |
| Black | 0.4207478 | 0.033267 | <.001 |
| Hispanic | 0.0864561 | 0.033515 | .001 |
| Other | 0.093974 | 0.083095 | .258 |
| History of hypertension | 0.0162243 | 0.013319 | .22 |
| History of diabetes | −0.024951 | 0.014078 | .07 |
| Cause of death | |||
| Trauma | ref | ||
| Anoxia | −0.085017 | 0.034143 | .01 |
| Stroke | 0.0429364 | 0.033657 | .20 |
| Other | −0.131504 | 0.071961 | .07 |
| Serum creatinine | −0.133606 | 0.006005 | <.001 |
| HCV positivity | −0.015216 | 0.02244 | .5 |
| DCD | 0.001086 | 0.013669 | .18 |
| Year from 2015 | 0.001086 | 0.006258 | .86 |
| KDPI | |||
| 81% | 0.1661722 | 0.046714 | <.001 |
| 82% | 0.0971008 | 0.046248 | .036 |
| 83% | −0.01513 | 0.046151 | .74 |
| 84% | −0.052451 | 0.045889 | .25 |
| 85% | ref | ||
| 86% | −0.091598 | 0.045888 | .046 |
| 87% | −0.188052 | 0.045783 | <.001 |
| 88% | −0.192616 | 0.045547 | <.001 |
| 89% | −0.253665 | 0.045889 | <.001 |
| 90% | −0.247002 | 0.046192 | <.001 |
To determine if there was a labeling effect of KDPI85, we examined kidneys with a KDRI between 1.785 and 1.849 that were classified as KDPIHIGH in years 2015–2017 and KDPILOW in years 2018–2020 (Figure 2 shaded area). For this narrow KDRI range, there were 694 donors in the KDPIHIGH era, 918 donors in the KDPILOW era, and the mean KDRI was the same (p = .1, Table 4). The discard rate was significantly higher when kidneys were labeled as KDPIHIGH compared to when kidneys were labeled as KDPILOW (44.9% vs. 39.1%, p < .01). The number of kidneys transplanted per donor likewise decreased with the KDPIHIGH designation, from 1.11 for KDPILOW to 0.94 for KDPIHIGH (p < .01). The biopsy rate was the same for KDPIHIGH versus KDPILOW kidneys (86.5% vs. 86%, p = .74), however, the discard rate was lower for KDPILOW kidneys compared with KDPIHIGH kidneys when a biopsy was done (40.1% vs. 47%, p < .001).
| 2015–2017 (KDPIHIGH) | 2018–2020 (KDPILOW) | p | |
|---|---|---|---|
| Donor factors | |||
| Donors, n | 694 | 918 | .01 |
| Mean KDRI ± SD | 1.816 ± 0.019 | 1.817 ± 0.019 | .1 |
| Age (y), median ± SD | 52.2 ± 16.07 | 53.58 ± 14.11 | .09 |
| Height (cm), median ± SD | 161.59 ± 27.59 | 164.33 ± 24.52 | .045 |
| Weight (kg), median ± SD | 79.01 ± 29.42 | 83.27 ± 28.65 | .005 |
| Race, n (%) | |||
| Asian | 23 (3.3%) | 28 (3.1%) | .74 |
| Black | 157 (22.6%) | 167 (18.2%) | .03 |
| Hispanic | 91 (13.1%) | 103 (11.2%) | .27 |
| Other | 19 (2.7%) | 15 (1.6%) | .14 |
| White | 404 (58.2%) | 605 (65.9%) | .002 |
| History of hypertension, n (%) | 468 (67.4%) | 593 (64.6%) | .49 |
| History of diabetes, n (%) | 148 (21.3%) | 207 (22.6%) | .58 |
| Cause of death, n (%) | |||
| Anoxia | 213 (30.7%) | 369 (40.2%) | .001 |
| CVA/stroke | 378 (54.5%) | 409 (44.6%) | .001 |
| Other | 13 (1.9%) | 34 (3.7%) | .048 |
| Trauma | 90 (13.0%) | 106 (11.5%) | .43 |
| Serum creatinine, median ± SD | 1.41 ± 1.09 | 1.56 ± 1.43 | .03 |
| HCV positivity, n (%) | 29 (4.2%) | 87 (9.5%) | <.001 |
| DCD, n (%) | 153 (22.0%) | 308 (33.6%) | <.001 |
| Procurement outcomes | |||
| Kidneys procured, n | 1186 | 1666 | |
| Kidneys transplanted, n (%) | 654 (55.1%) | 1015 (60.9%) | .002 |
| Kidneys discarded, n (%) | 532 (44.9%) | 651 (39.1%) | |
| Kidney transplanted per donor (n) | 0.94 | 1.11 | <.001 |
| Kidneys biopsied, n (%) | 1026 (86.5%) | 1433 (86.0%) | .74 |
| Discard rate by biopsy status, n (%) | |||
| Biopsy done | 482 (47.0%) | 575 (40.1%) | <.001 |
| Biopsy not done | 54 (33.8%) | 79 (34.1%) | .99 |
4 DISCUSSION
In this study, we have shown that the KDRI85 and the KDPI85 cutoffs change yearly to account for the procured kidneys from the year prior, but with consequences in how kidneys are labeled. We found that utilization rates drop at the KDPI85 cutoff and, by examining kidneys with the same raw KDRIRAO score but variable high KDPI designation, we have also shown that there is decreased organ utilization when kidneys are labeled as “high KDPI.” Our results demonstrate a labeling effect due to the “high KDPI” stigma.
Our findings are consistent with those of Stewart et al6 that showed when the yearly KDRI was erroneously calculated and falsely elevated the KDPI displayed in DonorNet, there was a significantly higher discard rate for kidneys that crossed the KDPI 85% threshold when they would have otherwise been below. They also found there was no change in organ acceptance when the KDPI increased so long as the KDPI remained less than 85%. Prior to December 2014, kidneys were dichotomously labeled as “expanded criteria donor” (ECD) or “standard criteria donors.”7 To move away from the dichotomy, KDPI was implemented to provide a continuous scale of kidney donor quality to make more nuanced clinical decisions. However, despite the increased granularity of the KDPI scale, the discard rate in the KAS era is the same as that of the ECD era.8 Our findings support the idea that the “high KDPI” label contributes to this elevated discard rate, analogous to the labeling of ECD kidneys.
KDPI is used as a continuous measure of kidney donor quality but comes with several limitations. The c-statistic in the original paper by Rao2 was calculated at 0.62, which is reasonably low. Furthermore, when comparing kidneys in the 25–50 quartile with kidneys in the 51–75 quartile, the c-statistic is only 0.58. That is, in just over half the attempts, the model would correctly place kidneys in the correct order of their failure times. This indicates the weak discriminatory ability for kidneys in adjacent quartiles, and if extrapolated, suggests that a small difference on the KDPI scale of 5%–10% is negligible. Yet, in this study, we have shown that not only is there decreased utilization of kidneys when crossing the KDPI85 threshold but kidneys with the same KDRIRAO are discarded at a higher rate due to the “high KDPI” label. We are basing decision making on perceived differences in kidneys rather than real ones.
Our findings have obvious implications for patients. Older patients, who are often the recipients of higher KDPI kidneys, benefit from a kidney transplant. Prior studies have shown that there is no survival benefit associated with declining a high KDPI kidney and remaining on the waitlist.9 With fewer kidneys procured and transplanted from KDPIHIGH donors, the organ pool is also effectively decreased. The KDPI85 value does not represent a point at which the kidney quality and predicted graft failure suddenly worsens, but merely a point along the continuum of a spectrum of graft outcomes that is gradually declining. Currently, patients are required to consent to receive a high KDPI graft, but from structured interviews, patients are often confused about what KDPI means, if they have actually consented to receive a high KDPI kidney, and they are unable to articulate the survival benefit of receiving a kidney transplant.10 This additional consent process not only stigmatizes the kidneys and decreases transplant rates, but patients are not truly informed.
Outside the United States, other countries are utilizing high KDPI kidneys more consistently. In a comparison of United States versus the United Kingdom transplant trends from 2006 to 2017, the median KDRI of transplanted kidneys in the United Kingdom was 1.37 compared to 1.13 in the United States.11 The United Kingdom also utilized older donors and kidneys from donors after circulatory deaths more commonly. Yet, despite the United Kingdom using more marginal kidneys, there was no difference in 1-year graft survival. In France, from 2004 to 2014, the deceased donor kidney discard rate was only 9.1%, compared to 17.9% in the United States.12 Over the study period, France utilized more marginal grafts from older donors, with an increase in KDRI from 1.37 to 1.74, compared to no significant change in the KDRI in the United States (1.30–1.32).
The 85th percentile was chosen as the marker for high KDPI kidneys as ECD kidneys previously comprised 15% of the donor pool. However, this is not a point at which the risk of graft failure or patient survival decreases. In fact, the Scientific Registry of Transplant Recipients (SRTR) uses KDRI (not KDPI) for risk adjustment, and the current cutoffs at which the Hazard Ratio becomes greater than 1 (i.e., higher risk for graft failure or patient death) are KDRI 1.58 for 1-year graft survival and 1.59 for 1-year patient survival.13 These values correspond to a KDPI of 90% based on the 2020 mapping table. Hence, it may be worth considering aligning the “high KDPI” label with the increased hazard identified by the SRTR to truly identify kidneys at higher risk for patient death or graft failure. Alternatively, we could consider using the raw KDRI for organ offers, which better represents the calculated quality of the kidney and would not vary from year to year. There would likely be an adjustment needed for such an approach, as the transplant community likely has low familiarity with the meaning and interpretation of KDRI.
Our study has limitations inherent to utilizing the OPTN database and the retrospective epidemiological approach. As such, we could not adjust for other measures of kidney quality that are not in the KDPI calculation that may influence organ acceptance, such as biopsy results and renal anatomy. Decision making around organ utilization is highly complex and cannot be accounted for in a retrospective study of this nature. Furthermore, there is the possibility that as the transplant community becomes more comfortable with accepting high KDPI kidneys, behavior around organ utilization is changing. As such, our observations reported here may not be a labeling effect, but rather a time effect (2015–2017 vs 2018–2020). We attempted to account for this in our multivariable analysis, which showed no time effect, however, because the time frame is short (only 6 years) there is the possibility of Type II error.
The results of the multivariable analysis suggest that kidneys from certain populations with high KDPI may be utilized at higher rates (older donors, Black, Asian, and Hispanic donors), and these findings should be further explored. Whether the long-term outcomes differ for similar KDPI kidneys is difficult to study, given the recipient selection bias for high KDPI kidneys versus standard kidneys. Outcomes will likely depend on the donor, recipient, and transplant variables, and is beyond the scope of this paper but deserve further inquiry. Lastly, geographic differences in high KDPI kidney utilization should be analyzed, as well as the impact of cold ischemia time, biopsy data, and pump information.
We have demonstrated that due to annual changes in procured kidneys, the KDPI85 cutoff shifts yearly with subsequent changes in which kidneys are labeled as “high KDPI.” This label directly impacts kidney utilization and the “high KDPI” label is associated with increased discard rates. Consideration should be given to the appropriateness of the “high KDPI” label.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.