Risk of cardiac-related mortality in stage IIIA-N2 non-small cell lung cancer: Analysis of the Surveillance, Epidemiology, and End Results (SEER) database
Funding information: Beijing Hope Run Special Fund of Cancer Foundation of China, Grant/Award Number: LC2016L03; Founding for Capital Clinical Special Application Research of China, Grant/Award Number: Z171100001017114; National Key Research and Development Program, Grant/Award Numbers: 2017YFC1311000, 1311002
Abstract
Background
In this study, we aimed to investigate the association between postoperative radiotherapy (PORT) and cardiac-related mortality in patients with stage IIIA-N2 non-small cell lung cancer (NSCLC) using the Surveillance, Epidemiology, and End Results (SEER) database.
Methods
The United States (US) population based on the SEER database was searched for cardiac-related mortality among patients with stage IIIA-N2 NSCLC. Cardiac-related mortality was compared between the PORT and Non-PORT groups. Accounting for mortality from other causes, Fine and Gray's test compared cumulative incidences of cardiac-related mortality between both groups. Univariate and multivariate analysis were performed using the competing risk model.
Results
From 1988 to 2016, 7290 patients met the inclusion criteria: 3386 patients were treated with PORT and 3904 patients with Non-PORT. The five-year overall incidence of cardiac-related mortality was 3.01% in the PORT group and 3.26% in the Non-PORT group. Older age, male sex, squamous cell lung cancer, earlier year of diagnosis and earlier T stage were independent adverse factors for cardiac-related mortality. However, PORT use was not associated with an increase in the hazard for cardiac-related mortality (subdistribution hazard ratio [SHR] = 0.99, 95% confidence interval [CI]: 0.78–1.24, p = 0.91). When evaluating cardiac-related mortality in each time period, the overall incidence of cardiac-related mortality was decreased over time. There were no statistically significant differences based on PORT use in all time periods.
Conclusions
With a median follow-up of 25 months, no significant differences were found in cardiac-related mortality between the PORT and Non-PORT groups in stage IIIA-N2 NSCLC patients.
INTRODUCTION
Chest radiotherapy plays an important role in the treatment of breast cancer, Hodgkin's lymphoma, lung cancer and other malignancies, which can also cause cardiovascular events and deaths. Cardiac-related mortality has long been recognized in patients with breast cancer or Hodgkin's lymphoma,1-5 with a typical latency period of more than a decade. The radiation-associated cardiac risk also appears to increase with time after exposure.5 As the life expectancy of patients with non-small cell lung cancer (NSCLC) continues to rise, cardiac-related mortality is apparent in long-term cancer survivors of NSCLC. Several studies report increased cardiac events and deaths after definitive radiotherapy for locally-advanced NSCLC (LA-NSCLC).6-9 Recently, the Radiation Therapy Oncology Group (RTOG) 0617 (A Randomized Phase III trial) reported that heart radiation dose was associated with worse overall survival with a median follow-up of two years, suggesting a contribution of radiation-induced cardiac mortality relatively soon after treatment.10 Postoperative radiotherapy (PORT) has been posited as an important component of the comprehensive treatment of operable stage IIIA-N2 NSCLC.11 However, evidence of cardiac-related mortality after postoperative radiotherapy (PORT) is more limited in recent years. Given the parallels in definitive radiotherapy of LA-NSCLC, cardiac-related mortality of PORT gains importance in stage IIIA-N2 NSCLC, especially with contemporary treatment modalities. In the present study, we assessed the effect of PORT on cardiac-related mortality in stage IIIA-N2 NSCLC patients using a large population-based database, and stratified these patients over time intervals to assess the cardiac-related mortality by treatment era.
METHODS
National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) database
The SEER database is an authoritative source of information on cancer incidence and survival in the United States, funded by the National Cancer Institute, collects data from approximately 28% of the population of the United States (US), which contains patient demographics, clinicopathological features, the first course of treatment, and follow-up for vital status. The SEER database is a worldwide public database, and we had permission to access the SEER database (authorization code 12201-Nov2019).
Case selection (patients, covariates, and treatment information)
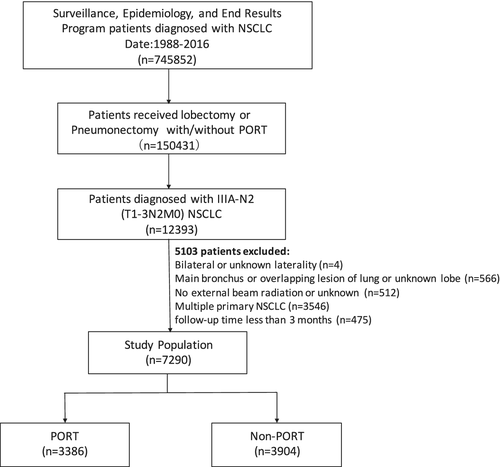
Our study population was chosen from the SEER database (SEER 18 Regs Custom data [with additional treatment field], Nov 2018 Sub [1975–2016 varying]). We used the SEER*Stat software (version 8.3.6.1) for data extraction. We identified our patient population by querying “Site recode ICD-O-3/WHO 2008” with the term “Lung and Bronchus” as the primary site. The following NSCLC histological types were included: adenocarcinoma (International Classification of Diseased for Oncology-3 [ICD-O-3] codes 8140–8141, 8143, 8147, 8480, 8481, 8260, 8550, 8570–8576, 8255), squamous cell (8070–8078), bronchoalveolar adenocarcinoma (8250–8254), adenosquamous (8560, 8562), 8046 (NSCLC, NOS) or large cell (8012–8014). We chose to examine the period from 1988 to 2016 because these years corresponded to the start of TNM staging by SEER and the most recent available patient information, respectively. Patients diagnosed with NSCLC between 1988 and 2016 who met the following criteria were included: (i) Patients underwent either a lobectomy or pneumonectomy, (ii) Patients diagnosed with T1-3N2M0 (stage IIIA-N2, American Joint Committee on Cancer third edition [for patients diagnosed from 1988–2003], American Joint Committee on Cancer sixth edition [for patients diagnosed from 2004–2009] and American Joint Committee on Cancer seventh edition [for patients diagnosed from 2010–2016]). The exclusion criteria were bilateral tumors or unknown laterality, main bronchus tumors or overlapping lesion or unknown lobe, without postoperative external-beam irradiation or unknown, multiple primary, and having survived for less than three months. Two cohorts were then created: (i) patients who received postoperative radiotherapy (PORT) as part of their initial therapy, and (iii) those who did not receive postoperative radiotherapy (Non-PORT) as part of their initial therapy. The workflow is shown in Figure 1.
For each case, we requested the following information: age, sex, race, year of diagnosis, histology, tumor laterality (right vs. left), subsite location (upper lobe, middle lobe, lower lobe), T stage, surgical procedure (lobectomy vs. pneumonectomy), use of radiotherapy, presumed survival in months, vital status, and cause of death. Cardiac-related mortality information was obtained from the cause of death data extracted from the SEER database.
Statistical analysis
We compared the differences in demographics, clinicopathology, and treatment characteristics among patients who did and did not receive PORT by chi-square test. The cardiac-related mortality rate during the study period was graphed by the initial year of diagnosis. We divided patients by the year of diagnosis of 1988–1997, 1998–2007, 2008–2016. Cumulative incidence curves of cardiac-related mortality (from the date of diagnosis) were constructed for PORT versus non-PORT, accounting for mortality from other causes. The underlying hazards were statistically compared using Fine and Gray's test. Univariate and multivariate analysis were performed using the competing risks regression (Fine and Gray method)12 to analyze the risk factors for cardiac-related mortality including age, sex, race, histology, tumor laterality, subsite location, T stage, surgical procedure, use of radiotherapy by assessment of the subdistribution hazard ratios (SHRs) and their corresponding 95% confidence interval (95% CI). A p-value of less than 0.05 was set as the threshold for significance. All analyses were performed with R Version 3.6.2 software.
RESULTS
We identified 7290 patients who met the criteria described above, including 3386 (46.4%) patients who received PORT and 3905 (53.6%) Non-PORT patients. The median age of the entire cohort was 66 years (range: 18–95 years). A comparison of demographic, clinicopathological and treatment factors is shown in Table 1. The distribution of age (p < 0.001), year of diagnosis (p < 0.001), histological type (p = 0.039), subsite location (p = 0.002) by comparing patients who received PORT with Non-PORT reached statistical significance. The median follow-up was 25 months (range: 3–320 months). A total of 308 patients died of cardiac-related diseases. A total of 145 and 163 patients died of cardiac-related diseases in the PORT and Non-PORT groups, respectively.
| N = 7290 | PORT N = 3386(%) | Non-PORT N = 3904(%) | p-value | |
|---|---|---|---|---|
| Age (years) | <0.001 | |||
| <65 | 3276 | 1716 (50.7) | 1560 (40.0) | |
| >=65 | 4014 | 1670 (49.3) | 2344 (60.0) | |
| Sex | 0.337 | |||
| Male | 3658 | 1720 (50.8) | 1938 (49.6) | |
| Female | 3632 | 1666 (49.2) | 1966 (50.4) | |
| Race | 0.806 | |||
| White | 5952 | 2760 (81.5) | 3192 (81.8) | |
| African American | 705 | 326 (9.6) | 379 (9.7) | |
| Other | 624 | 297 (8.8) | 327 (8.4) | |
| Not recorded | 9 | 3 (0.1) | 6 (0.2) | |
| Year of diagnosis | <0.001 | |||
| 1988–1997 | 1178 | 802 (23.7) | 376 (9.6) | |
| 1998–2007 | 2969 | 1249 (36.9) | 1720 (44.1) | |
| 2008–2016 | 3143 | 1335 (39.4) | 1808 (46.3) | |
| Histology | 0.039 | |||
| Adenocarcinoma | 4400 | 2094 (61.8) | 2306 (59.1) | |
| Squamous | 1717 | 757 (22.4) | 960 (24.6) | |
| NSCLC others | 1173 | 535 (15.8) | 638 (16.3) | |
| Tumor Laterality | 0.106 | |||
| Left | 3285 | 1491 (44.0) | 1794 (46.0) | |
| Right | 4005 | 1895 (56.0) | 2110 (54.0) | |
| Subsite location | 0.002 | |||
| Upper lobe | 4453 | 2117 (62.5) | 2336 (59.8) | |
| Middle lobe | 347 | 178 (5.3) | 169 (4.3) | |
| Lower lobe | 2490 | 1091 (32.2) | 1399 (35.8) | |
| T stage | 0.09 | |||
| T1 | 2009 | 924 (27.3) | 1085 (27.8) | |
| T2 | 4391 | 2018 (59.6) | 2373 (60.8) | |
| T3 | 890 | 444 (13.1) | 446 (11.4) | |
| Surgical procedure | 0.247 | |||
| Lobectomy | 6406 | 2992 (88.4) | 3414 (87.4) | |
| Pneumonectomy | 884 | 394 (11.6) | 490 (12.6) |
- Abbreviations: PORT, postoperative radiotherapy; Non-PORT, without postoperative radiotherapy.
Figure 2 shows the cardiac-related mortality curves stratified by PORT use. The five-year overall cardiac-related mortality was 3.01% in the PORT group compared with 3.26% in the Non-PORT group. There were no significant differences (p = 0.49) between PORT and Non-PORT patients (Figure 2(a)). The five-year overall cardiac-related mortality for PORT versus Non-PORT patients in each time interval was as follows: 3.62% vs. 3.99% (1988–1997), 3.37% vs. 3.39% (1998–2007) and 2.21% vs. 2.81% (2008–2016), respectively. When evaluating cardiac-related mortality in each of the time periods (Figure 2(b)-(d)), the overall incidence of cardiac-related mortality was decreased over time. There were no statistically significant differences based on PORT use in all time periods.
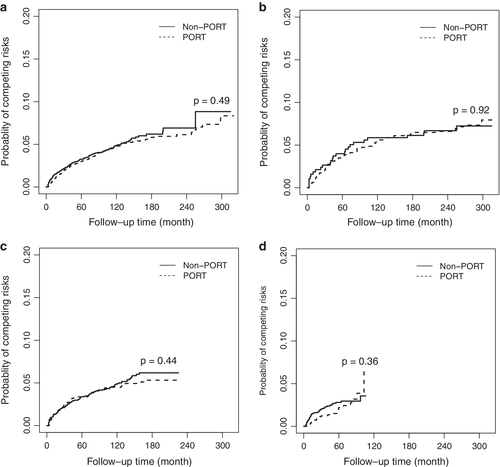
Table 2 shows the results of univariate and multivariate models, accounting for several confounding variables and mortality from other causes. On univariate analysis, cardiac-related mortality events were significantly associated with age>= 65 (p < 0.001), male patients (p < 0.001), year of diagnosis between 1988 and 1997 (p < 0.001), squamous cell carcinoma (p < 0.001), and T1 stage (p < 0.001). On multivariate analysis, age, sex, year of diagnosis, histology, and T stage remained significantly associated with cardiac-related mortality. On univariate and multivariate analysis, PORT was not associated with an increased risk for cardiac-related mortality (univariate: SHR = 1.0, 95% CI: 0.97–1.24, p = 0.97; multivariate: SHR = 0.99, 95% CI: 0.78–1.24, p = 0.91).
| Fine-Gray hazard model of cardiac related death (univariate) | Fine-Gray hazard model of cardiac related death (multivariate) | |||||
|---|---|---|---|---|---|---|
| SHR | 95%ci | p-value | SHR | 95%ci | p-value | |
| Age (years) | ||||||
| <65 | Ref | Ref | ||||
| >=65 | 1.69 | 1.34–2.15 | <0.001 | 1.67 | 1.32–2.12 | <0.001 |
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 0.65 | 0.52–0.82 | <0.001 | 0.71 | 0.57–0.90 | <0.001 |
| Race | ||||||
| White | Ref | Ref | ||||
| African American | 1.31 | 0.93–1.85 | 0.12 | 0.35 | 0.96–1.90 | 0.08 |
| Others | 0.43 | 0.24–0.76 | <0.001 | 0.50 | 0.28–0.89 | 0.02 |
| Year of diagnosis | ||||||
| 1988–1997 | Ref | Ref | ||||
| 1998–2007 | 1.19 | 0.95–1.49 | 0.13 | 0.75 | 0.57–0.98 | 0.03 |
| 2008–2016 | 0.51 | 0.39–0.67 | <0.001 | 0.46 | 0.33–0.64 | <0.001 |
| Histology | ||||||
| Adenocarcinoma | Ref | Ref | ||||
| Squamous | 1.97 | 1.57–2.48 | <0.001 | 1.86 | 1.44–2.42 | <0.001 |
| NSCLC others | 1.00 | 0.75–1.35 | 0.98 | 1.22 | 0.89–1.67 | 0.23 |
| Tumor laterality | ||||||
| Left | Ref | |||||
| Right | 0.88 | 0.70–1.09 | 0.24 | 0.85 | 0.67–1.07 | 0.16 |
| Subsite location | ||||||
| Upper lobe | Ref | Ref | ||||
| Middle lobe | 1.02 | 0.61–1.71 | 0.93 | 1.18 | 0.69–2.02 | 0.55 |
| Lower lobe | 1.16 | 0.92–1.47 | 0.20 | 1.15 | 0.90–1.46 | 0.27 |
| T stage | ||||||
| T1 | Ref | Ref | ||||
| T2 | 1.20 | 0.95–1.51 | 0.13 | 0.85 | 0.65–1.10 | 0.21 |
| T3 | 0.42 | 0.25–0.69 | <0.001 | 0.39 | 0.23–1.66 | <0.001 |
| Surgical procedure | ||||||
| Lobectomy | Ref | Ref | ||||
| Pneumonectomy | 1.24 | 0.91–1.69 | 0.16 | 1.02 | 0.74–1.42 | 0.89 |
| Radiation | ||||||
| Non-PORT | Ref | |||||
| PORT | 1.00 | 0.80–1.24 | 0.97 | 0.99 | 0.78–1.24 | 0.91 |
- Note: An SHR > 1 was associated with increased mortality.
- Abbreviations: 95% CI, 95% confidence interval; Non-PORT, without postoperative radiotherapy; PORT, postoperative radiotherapy; PORT, postoperative radiotherapy; Ref, reference; SHR indicates subdistribution hazards ratio.
DISCUSSION
The effect of PORT on cardiac-related mortality is critical due to cardiac-related mortality risks being inadequately captured in recent years. Our population-based analysis offers a holistic update on the cardiac-related mortality risks in stage IIIA-N2 NSCLC patients who underwent PORT. To our knowledge, this is the first study concentrating on the incidence and trends of competing risk cardiac-related mortality in stage IIIA-N2 NSCLC patients over a long observation period, and the results show that cardiac-related mortality has no association with PORT use between 1988 and 2016. The incidence of cardiac-related modality has also decreased over time.
Previous studies have demonstrated a benefit in local-regional control by using PORT but whether PORT could improve overall survival remains controversial.13-18 The insignificant survival benefits with PORT could partially be explained by the early and late toxicities, including radiation esophagitis, radiation pneumonitis and radiation induced heart diseases. Cardiac-related mortality is also one of the detrimental effects of PORT on survival. Several studies have reported increased cardiac-related mortality with PORT after surgery in patients with stage I to III NSCLC.19-21 Lally et al20 conducted a study on the risk of cardiac-related mortality associated with PORT of resected NSCLC patients. It was demonstrated that PORT was associated with an increase in cardiac-related mortality independent of the expected effects of age, sex, and race between 1983 and 1988 by using the SEER database. However, significant differences exist between Lally et al20 and our study, given the substantial heterogeneity in patient selection, year of diagnosis and method of statistical analysis. First, in the study by Lally et al,20 a mixture of patients with varying stages (stage I to III) of resected NSCLC were included. In contrast, our study concentrated on stage IIIA-N2 NSCLC patients, representing a population most likely to benefit from PORT. Second, the recruitment of patients included in Lally et al20 was from 1983 to 1988 compared with 1988 to 2016 in our study. Finally, comparing the results of the study by Lally et al,20 our study used a competing risk model to avoid overestimating the cumulative survival rate and incorrectly evaluating the effects of covariates on the hazard ratio to the occurrence of the cardiac-related death event. This guaranteed the reliability of the results in our study.
Our study found an approximate 3% cardiac-related mortality rate at five years experienced by all patients with IIIA-N2 NSCLC who received either PORT or Non-PORT. The insignificant difference in cardiac-related mortality observed between the PORT and Non-PORT groups in our study was probably due to the contemporary radiation techniques, limited volumes of radiation, suitable radiation doses and fraction sizes.22, 23 Taken together, these factors probably decreased the volume of the heart exposed to high dose radiation. Trials with contemporary radiation techniques have demonstrated that there was no increase in death from intercurrent disease.24-28 A series of recently published nonrandomized trials could not detect a difference in cardiac-related mortality between patients receiving the 3D-planned PORT group in comparison to the Non-PORT group.14, 29, 30 What is more, the advances in lung cancer treatment could also explain the decrease of cardiac-related mortality over time (1988–2016). The trends are consistent with the analysis of Lally et al20 and Haque et al.9 Lally et al20 demonstrated the decrease of cardiac-related mortality in resected NSCLC patients (1983–1993), while Haque et al9 illustrated that the incidence of cardiac-related mortality has decreased over time in LA-NSCLC (1988–2014). Recently, the multi-institutional randomized phase III trial LungART reported the initial results at the European Society for Medical Oncology (ESMO) congress 2020, which showed a nonstatistically significant improvement in disease-free survival (DFS) (three-year DFS: 47.1% vs. 43.8%, p = 0.16) and overall survival (OS) (three-year OS: 66.5% vs. 68.5%, HR not as yet provided).18 Early and late grade 3–5 cardiopulmonary toxicity was 7% and 20%, respectively in the PORT group compared with 3.2% and 7.7% in the Non-PORT group. The survival benefit may be counterbalanced by the toxicities. However, the influence of cardiac-related toxicity remains controversial until detailed data is published.
On univariate and multivariate analysis, our study confirmed that patients of older age, male patients, squamous cell lung cancer, earlier year of diagnosis and earlier T stage were more likely to have higher rates of cardiac-related mortality. The high cardiac-related mortality may be explained by the baseline risks above rather than being related to the radiotherapy.31, 32 This implies that extra attention to cardiac sparing may be required in patients with greater comorbidities or those with a potential for longer survival.33 Cardiac monitoring with imaging and routine involvement of cardiologists in the pre- and post-treatment care may be necessary for patients with cardiac-related mortality risk factors. Although there is no association between PORT use and cardiac-related mortality, cardiovascular issues such as cardiomyopathy, arterial disease, hypertension, and vascular and metabolic issues could manifest during or after therapy due to PORT-related toxicities. We encourage clinical attentiveness to cardiac-sparing radiotherapy and emphasize overall health through management of early and late cardiac toxicities. With the increasing life expectancy of patients with stage IIIA-N2 NSCLC, further studies are needed in order to provide dosimetric correlates for cardiac toxicities, which is rarely reported in previous studies.34
Several limitations should be acknowledged when interpreting our results. First, just as other studies derived from the SEER database, our study is limited by the lack of important parameters, such as the following: comorbid conditions, smoking history, chemotherapy utilization, radiation therapy dose, technique and target, which are potential confounders for our study. Only cardiac-related mortality is described in our study due to the lack of information on cardiac events. Second, there is an inherent weakness of selection bias in a population-based observational study. Third, the number of events was low, which limits the examination of multiple covariates.
These shortcomings notwithstanding, our study is still the largest retrospective study to address this important clinical question. What is more, the large cohort of population-based patients provides sufficient power to detect relatively small increases in cardiac-related mortality for stage IIIA-N2 NSCLC. We believe that PORT use is safe in stage IIIA-N2 NSCLC patients, without worrying about cardiac-related mortality.
In conclusion, this study characterizes the cardiac-related mortality by PORT use in patients with NSCLC. In all patients over the period studied, no significant differences were found in cardiac-related modality between the PORT and Non-PORT groups in stage IIIA-N2 NSCLC patients. The overall incidence of cardiac-related mortality was decreased over time. Although the association with PORT cannot be proven in our study, we still encourage attentiveness to early and late cardiac toxicities. More studies are required to determine the association between cardiac toxicities and PORT in patients with stage IIIA-N2 NSCLC.
ACKNOWLEDGMENTS
This study was supported by the National Key Research and Development Program (2017YFC1311000, 1311002), the Founding for Capital Clinical Special Application Research of China (Z171100001017114) and Beijing Hope Run Special Fund of Cancer Foundation of China (LC2016L03).
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships.