Precise resection of multiple pulmonary nodules using a three-dimensional reconstruction model: A case report
Funding information: Project of National Natural Science Foundation, Grant/Award Numbers: 81673031, 81872510; Guangdong Provincial People's Hospital Young Talent Project, Grant/Award Number: GDPPHYTP201902; High-Level Hospital Construction Project, Grant/Award Number: DFJH201801; Key Lab System Project of Guangdong Science and Technology Department-Guangdong Provincial Key Lab of Translational Medicine in Lung Cancer, Grant/Award Number: 2017B030314120; Research Fund from Guangzhou Science and Technology Bureau, Grant/Award Number: 201704020161
Abstract
A 48-year-old woman presented to our department and chest computed tomography (CT) revealed five pulmonary nodules, two of which were in the left upper lobe of the lung and three in the superior segment of the left lower lobe., All the lesions were resected for comprehensive histological assessment in order to distinguish synchronous multiple primary lung cancers (SMPLCs) from intrapulmonary metastases. The nodules were all successfully removed by minimally invasive surgery under the guidance of three dimensional (3D) reconstruction, in order to preserve as much lung function for the patient as possible. Postoperative histopathological examination demonstrated the presence of SMPLC. The patient was discharged from hospital on postoperative day 4 without any complications.
INTRODUCTION
Recently, due to the widespread use of high-resolution imaging systems, if a large number of multiple tumor nodules are found to be present they are diagnosed as synchronous multiple primary lung cancers (sMPLCs). However, it can be difficult to distinguish sMPLCs from intrapulmonary metastases. To address this problem, we'd better resect all lesions for comparison of histological examination and EGFR mutation status in different pulmonary nodules.1 However, removing multiple nodules often means removing more lung tissue, and patients with poor lung function are subsequently placed at risk. The application of minimally invasive lung surgery enables the total resection of multiple nodules.
CASE REPORT
A 48-year-old woman presented at our clinic and chest routine computed tomography (CT) revealed five pulmonary nodules in the left lobe of the lung. A 9.2-mm diameter dominant pulmonary nodule in the lateral subsegment of the superior segment of the left lower lobe (LS6b) with a partially serrated border was visible on imaging and was determined to be a mixed ground-glass nodule (mGGO). This had increased in size over several months (Figure 1(a)). We also found a further two pure ground-glass nodules (pGGOs) in the superior and medial subsegments of the superior segment of the left lower lobe (4.7 mm, LS6a and 3.2 mm, LS6c, respectively)(Figure 1(b),(c)), and two pGGOs located in the medial subsegment of the ventral segment and lateral subsegment of the superior lingular segment of the left upper lobe (4.7 mm, LS3b and 4.4 mm, LS4a, respectively) (Figure 1(d),(e)). The previous medical history of the patient included hypertension treated with oral medication. No other significant history was identified. Pulmonary function tests were normal.

The data of CT scans containing 1.0-mm slices were used to generate virtual 3D model using 3D reconstruction software (Intelligent surgery planing platform, Perception Vision Medical Technologies Co.,Ltd), which was in turn used to evaluate the location of lesions and anatomical structures. Colors were used to highlight the bronchus and blood vessels of the lung (Figure 1(f). After examination of the anatomical characteristics on a 3D reconstruction model, interestingly we found that the small nodule in LS3b was between the root of pulmonary veins of V3c and V3b + a (V3c: the vein between S3bi and S3bii, V3b: the vein below S3b, V3a: the vein between S3a and S3b).
Under general anesthesia with single lung ventilation, video-assisted thoracoscopic surgery (VATS) was performed with the patient placed in the right decubitus position.
On thoracoscopy, the small nodule in LS3b was invisible on the pleural surface. However, preoperatively using a 3D reconstruction model, we were able to pinpoint the exact location of the nodule which was between the root of pulmonary veins of V3c and V3b +. A minimally invasive procedure was subsequently performed to remove the nodule using blunt and sharp dissection using electrocautery along the veins of V3c and V3b + a (Figure 2(a1)–(a3)). The pulmonary nodule in LS4a was visible on the pleural surface, and a wedge resection was performed to resect the p-GGO using an endoscopic stapler (Figure 2(b1)–(b3)).
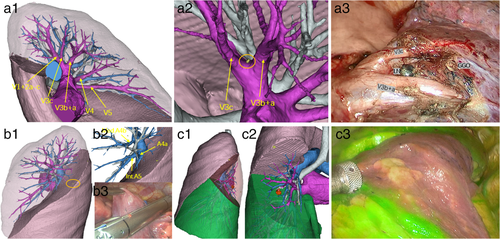
The three nodules in the superior segment of the lower lobe were completely removed by standard segmentectomy of S6 using ICG combined with near-infrared fluorescence (Figure 2(c1)–(c3)). The hilar and subcarinal lymph nodes were removed and then sent to the pathology department for examination.
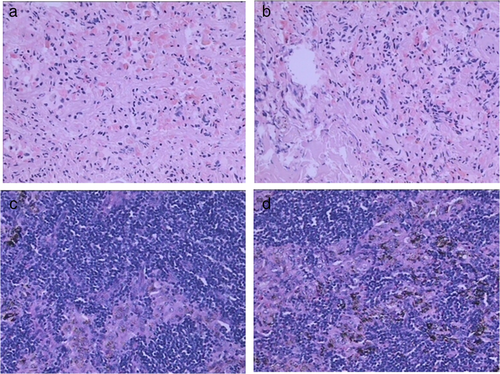
Postoperative histopathological examination revealed that the dominant nodule in LS6b was T1aN0M0 invasive adenocarcinoma (IA) (acinar (90%), lepidic (10%) growth), and the nodule in LS6a was microinvasive adenocarcinoma (MIA) and another nodule in LS6c was benign. The small nodule in LS3b was in situ adenocarcinoma (AIS) (Figure 3(a),(b)), and another nodule in LS4a was microinvasive adenocarcinoma (MIA). All the lymph nodes examined were negative (Figure 3(c),(d)). According to the clinical diagnostic criteria,2 the patient was finally diagnosed with sMPLC.
The amount of blood loss was 20 ml, and the duration of surgery was 255 min. The chest drainage tube was removed on the second day after the operation. The patient was discharged from hospital on postoperative day 4 without any complications.
DISCUSSION
The overall prognosis of simultaneous multiple primary lung cancer is better than intrapulmonary metastatic tumor.3, 4 The stage of the dominant lesion affects the patient's long-term prognosis and requires priority management and surgical intervention, but we can’t ignore or disorderly deal with the non-dominant lesions because they provide important information for differentiating SMPLCs and intrapulmonary metastatic tumor.5, 6
In the present case, using 3D images for presurgical evaluation, we were able to accurately localize and remove all the five nodules to distinguish SMPLC from intrapulmonary metastases.
Therefore, with the assistance of preoperative 3D simulation of the complicated vessels and the bronchi, as well as the space between the lesion and adjacent tissues, surgeons are able to remove multiple pulmonary nodules safely and accurately.
ACKNOWLEDGMENTS
This work was supported by Key Laboratory System Project of Guangdong Science and Technology Department–Guangdong Provincial Key Laboratory of Translational Medicine in Lung Cancer (Grant No. 2017B030314120), Project of National Natural Science Foundation (Grant Nos. 81673031, 81872510), Research Fund from Guangzhou Science and Technology Bureau (Grant No. 201704020161), High-Level Hospital Construction Project (Grant No. DFJH201801), and Guangdong Provincial People's Hospital Young Talent Project (Grant No. GDPPHYTP201902).
CONFLICT OF INTEREST
Dr W. Z. Zhong has received honoraria from AstraZeneca and Roche outside the submitted work; Dr Y. L. Wu has received honoraria from AstraZeneca, Eli Lilly, Roche, Pierre Fabre, Pfizer, and Sanofi; consulting or advisory tole with AstraZeneca, Roche, Merck, and Boehringer Ingelheim and Roche outside the submitted work. The remaining authors declare no conflict of interest.