Unusual lung involvements of invasive mucinous adenocarcinoma with chylothorax
Abstract
A 77-year-old man who had a persistent productive cough for one month was admitted to our hospital. Chest computed tomography (CT) revealed subpleural nodular opacities, irregular pleural thickening with bilateral basal predominance, and a small right pleural effusion. Aspirated fluid was exudative and had the appearance of chylothorax without malignant cells. Surgical lung biopsy specimen showed focal proliferation of neoplastic epithelial cells with lepidic-predominant pattern and abundant mucus in the alveolar spaces, consistent with invasive mucinous adenocarcinoma (IMA). The results of PD-L1 expression and the EGFR, ALK, ROS1, and BRAF mutation status analyzed by next generation sequencer were all negative. IMA should be considered in the differential diagnosis of subpleural micronodular opacities accompanied by pleural effusion (chylothorax) on chest CT.
Key points
Significant findings of the study
This case showed subpleural micronodular opacities and chylothorax as unusual chest computed tomography (CT) patterns for invasive mucinous adenocarcinoma (IMA).
What this study adds
Invasive mucinous adenocarcinoma (IMA) should be considered in the differential diagnosis of subpleural micronodular opacities accompanied by pleural effusion on chest CT.
A 77-year-old man with a history of a persistent productive cough for one month was admitted to our hospital. Chest computed tomography (CT) revealed subpleural nodular opacities, irregular pleural thickening with bilateral basal predominance, and a small right pleural effusion (Fig 1). The differential diagnosis included diffuse pan-bronchiolitis, mycobacterium infection, pulmonary sarcoidosis, and lymphoma; however, there was no increase in blood angiotensin-converting enzyme or carcinoma-specific tumor markers including carcinoembryonic antigen, squamous cell carcinoma antigen, cytokeratin 19 fragment, neuron specific enolase, sialyl lewis X-i antigen, or soluble interleukin-2 receptor; and no evidence of specific pathogens or malignant cells in the sputum. After administration of macrolide and new quinolone antibiotics, the pleural effusion worsened slightly and lung involvement became more apparent. Aspirated fluid was exudative (protein; 2.8 g/dl, lactate dehydrogenase; 331 mg/dL), with a total cell count of 775/μL and lymphocyte predominance. It also had the appearance of chylothorax, with elevated triglyceride levels (160 mg/dL [pleural effusion] vs. 128 mg/dL [blood]) and without malignant cells. Although 18F-fluorodeoxyglucose positron emission tomography-computed tomography (18F-PET-CT) revealed no remarkable FDG uptake, surgical lung biopsy was performed to obtain a definitive diagnosis of lung involvement. The histological specimen showed focal proliferation of neoplastic epithelial cells with lepidic-predominant pattern and abundant mucus in the alveolar spaces (Fig 2). Immunohistochemical results were CK7 (+), TTF-1 (−), CK20 (−), HNF-1α (−), and Ki-67 (≥30%), consistent with invasive mucinous adenocarcinoma (IMA). The results of PD-L1 expression and the EGFR, ALK, ROS1, and BRAF mutation status analyzed by next-generation sequencing (NGS) were all negative.

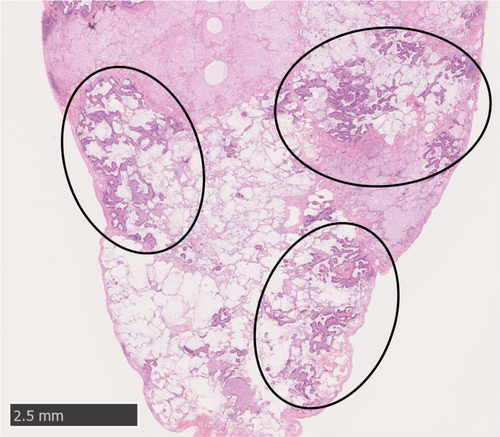
Typical CT findings of IMA of the lung are a mass-like opacity or consolidation mimicking lobar pneumonia.1-3 However, this case showed a very rare CT pattern of subpleural micronodular opacities that was difficult to identify as lung carcinoma. Moreover, this case was accompanied by chylothorax due coincidentally to tumor progression. Therefore, IMA should be considered in the differential diagnosis of subpleural micronodular opacities accompanied by pleural effusion on chest CT.
Disclosure
None of the authors have any real or perceived conflicts of interest to declare in relation to this manuscript.