Three-dimensional printed navigational template for localizing small pulmonary nodules: A case-controlled study
Abstract
Background
Localization of small pulmonary nodules is an inevitable challenge for the thoracic surgeon. This study aimed to investigate the accuracy of three-dimensional (3D) printing technology for localizing small pulmonary nodules, especially ground-glass nodules (GGNs).
Methods
This study enrolled patients with peripheral small pulmonary nodules (≤ 2 cm) who required preoperative localization. In the comparison period, patients underwent both computed tomography-guided (CT-G) and 3D-printing template guided (3D-G) localization to compare the accuracies of the two methods. In the testing period, the 3D-printing technique was implemented alone. The 3D-printing physical navigational template was designed based on data from perioperative CT images. Clinical data, imaging data, surgical data, and evaluation index were collected for further analysis. The learning curve of the 3D-printing localization technique was assessed using cumulative sum (CUSUM) analysis and multiple linear regression analysis.
Results
In the comparison period (n = 14), the success rates of CT-G and 3D-G were 100% and 92.9% (P = 0.31), respectively; in the testing period (n = 23), the success rate of 3D-G was 95.6%. The localization times of CT-G, 3D-G (comparison), and 3D-G (testing) were 23.6 ± 5.3, 19.3 ± 6.8, and 9.8 ± 4.6 minutes, respectively. The CUSUM learning curve was modeled using the equation: Y = 0.48X2 − 0.013X − 0.454 (R2 = 0.89). The learning curve was composed of two phases, phase 1 (the initial 20 patients) and phase 2 (the remaining 17 patients).
Conclusions
3D printing localization has adequate accuracy and is a feasible and accessible strategy for use in localizing small pulmonary nodules, especially in right upper lobe. The use of this technique could facilitate lung nodule localization prior to surgery.
Introduction
Implementation of lung cancer screening using low-dose computed tomography (CT)1 has increased the rate of detection of small peripheral pulmonary nodules. The diagnosis and treatment of small pulmonary nodules is a major challenge for thoracic surgeons. In recent years, sublobar resection (segmentectomy and wedge resection) has become the mainstream therapeutic method for these nodules as a result of prospective studies (CLGB140503/JCOG0802).2
However, it is hard to localize these nodules by palpation because of their small volume and long distance to the nearest pleural surface.3 Multiple preoperative localization methods have been used to localize the small lung nodule, such as CT-guided percutaneous puncture or hookwire, CT-guided (CT-G) injection of lipiodol or methylene blue dye, electromagnetic navigation bronchoscopic-guided dye marking, and virtual assisted lung mapping.3-6 CT-G percutaneous needle puncture localization is currently the most commonly used approach for localization. Although this technique has a success rate of over 95%, the limitations are well documented too.7 With CT-G methylene blue dye marking, the dye can spread easily, while with the hook-wire, dislodgement occurs in approximately 5% of patients. Another drawback of these methods is that the patient is apprehensive about the procedure, since they are invasive. Finally, it exposes the patients to increased radiation.7
In recent years, the three-dimensional (3D) printing technique has been gradually applied to clinical therapy. Zhang et al.8, 9 developed a localization method for small pulmonary nodules, using a 3D-printed navigational template to mark the puncture site and angle. The 3D-printed template-guided (3D-G) localization they performed was printed with nylon (PA3200), assisted by hookwire, and required pre-evaluation by CT scanning. However, the template we used was printed with photosensitive resin, and the localization assisted by methylene blue dye and performed in an operating room without CT pre-evaluation. Both methods were regarded as a failure if deviation of more than 2 cm was found on the CT scan.
To further clarify the confounding factors, we developed our own 3D printing localization procedure. In contrast to traditional CT-G percutaneous puncture localization, our procedure was performed in the operating room without CT scan evaluation.
Methods
Study population
This study was approved by the Institutional Review Board of Guangdong Provincial People's Hospital (No. GDREC2017261H) and registered with ClinicalTrials.gov, number NCT04056923. Patients who met the inclusion criteria were informed about the risks and benefits of the procedure, and written informed consent was obtained.
This was a prospective study and conducted between 4 January 2018, and 7 June 2018. The surgeon assessed the eligibility of patients with peripheral lung nodule for pulmonary sublobar resection by video-assisted thoracoscopic surgery (VATS). Inclusion criteria were as follows:
(i) a maximum target lung nodule diameter ≤ 20 mm; (ii) a target nodule consolidation/tumor ratio (CTR) <0.25, or a minimum distance from the outer edge of the nodule to the nearest pleural surface >10 mm if the target nodule CTR was >0.25.
Study design
The study was divided into two periods. In the early period (comparison period), localization was performed by both CT-G indocyanine green marking in the radiology department and by intraoperative 3D-G methylene blue dye marking in the operating room. In the later period (testing period), the 3D-G technique was implemented alone. Clinical data, imaging data, surgical data, and evaluation index were collected for further analysis.
Template design and printing
In the first step, routine CT scan was performed on patients with small pulmonary nodules with a slice thickness of 1 mm. We downloaded the patient's CT images from the picture archiving and communication system and performed a 3D reconstruction of the thoracic cavity using Mimics software (Materialize NV, Leuven, Belgium). After 3D reconstruction, the location of the small nodule in the lung can be clearly judged.
Subsequently, we designed a navigational template on the patient's 3D reconstruction model using Mimics software. The positional relationship between the navigational template and anatomical landmarks on the thoracic wall was measured and calculated by the software, and the orientation, position, angle, and depth of the puncture point were determined.
After the design of this 3D navigational template model was completed, the model was then printed using the J501Pro printer (Zhuhai Seine Technology Co., Ltd., Zhuhai city, China) with photosensitive resin (RGD100T, RGD100C, RGD100M, RGD100Y, RGD100W). The template design and the printing procedure took approximately three to five hours to complete (Fig 1).
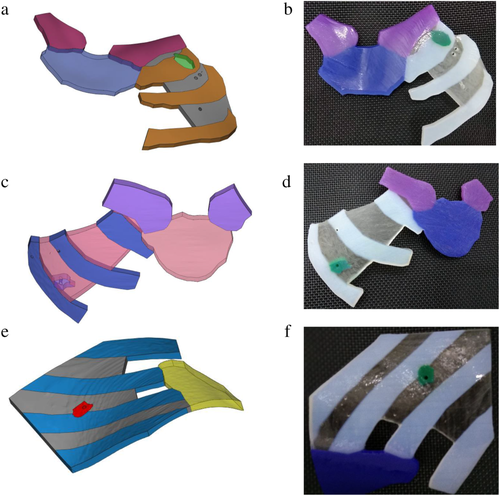
Localization procedure
In the comparison period, the surgeon performed preoperative CT-G percutaneous indocyanine green localization in the CT room on the day of the surgery. After CT-G localization was completed, the patient was transferred to the operating room.
The 3D printing localization was performed in the operating room. After induction of general anesthesia, patients were placed in the standard lateral position before or after the 3D printing localization based on the site of the puncture point on the thoracic wall. If the puncture point was located in the anterior thoracic wall, the patient was placed in the supine position to perform the localization; for puncture points in locations other than the anterior thoracic wall, the patient was placed in the lateral position. The 3D printing navigational template was placed on the patient's thoracic wall based on anatomical landmarks. The puncture angle was guided by the template and the puncture depth was decided according to the prior design of the 3D reconstruction model (Fig 2). We injected methylene blue during inflation of the lung by the ventilator.
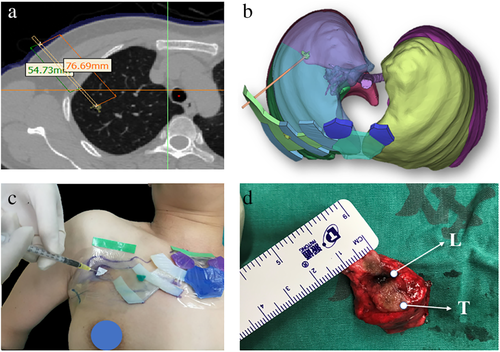
Deviation measurement
After lung resection, we directly measured the distance between location site and the target nodule in the specimen. Based on our previous experience with CT-G localization, a deviation of less than 2 cm was considered a successful localization.
Statistical analysis
Continuous data were expressed as median with interquartile ranges. Categorical variables were analyzed using the chi square test. P < 0.05 was considered statistically significant. The learning curve of the 3D-printing localization technique was assessed using a cumulative sum (CUSUM) analysis and multiple linear regression analysis. CUSUM was the running total of the differences between the individual data points and the mean of all data points, and it could be performed recursively.10 CUSUM analysis was performed to assess the change in trends of localization operation time and the distance error (vertical axis). The cases were ordered chronologically from the earliest to the latest date of the location procedure (horizontal axis). We performed the curve of best fit for the plot for detecting a change in slope of CUSUM learning curve. All statistical analyses were performed using IBM SPSS Statistics version 22.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 47 patients were approached, and 43 patients provided consent to participate. Six patients dropped out of the study due to being unfit for surgery (n = 2), missing template (n = 1), or unplanned change in the surgical schedule (n = 3). In this study, 14 patients were enrolled in the comparison period and 23 patients were enrolled in the testing period. The baseline patient characteristics and nodule characteristics are summarized in Table 1.
| Comparison period (n = 14) | Testing period (n = 23) | P-value | |
|---|---|---|---|
| Age, in years (IQR) | 49.5 (48–56.5) | 58 (45–65) | 0.546 |
| Sex, n (%) | 1.000 | ||
| Male | 6 (42.9%) | 10 (43.5%) | |
| Female | 8 (57.1%) | 13 (56.5%) | |
| Smoking history, n (%) | 1.000 | ||
| Never | 10 (71.4%) | 17 (73.9%) | |
| Former/current | 4 (28.6%) | 6 (26.1%) | |
| Nodule size (mm) | 7.2 ± 3.1 | 8.9 ± 4.0 | 0.423 |
| CTR (mean, range) | 0.19 (0–1) | 0.23 (0–1) | 0.733 |
| Localization, n | |||
| RUL | 12 | 12 | |
| RML | 1 | 1 | |
| RLL | 1 | 3 | |
| LUL | 0 | 4 | |
| LLL | 0 | 3 | |
| Depth (mm) | 12.5 ± 6.3 | 10.0 ± 7.4 | 0.292 |
| Percutaneous puncture approach, n | |||
| Anterior | 10 | 9 | |
| Posterior | 3 | 6 | |
| Lateral | 1 | 8 |
- CTR, consolidation/tumor ratio; LLL, left lower lobe; LUL, left upper lobe; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe.
In the comparison period (n = 14), the sex distribution was almost equal, with 43% male patients. The median age was 49 years (range 40–79 years). The median nodule diameter was 6.5 mm (range 3–14 mm) and the median nodule depth was 12.4 mm (range 2.2–26 mm). The nodules were mainly located in the right upper lobe (12/14) and the most common percutaneous puncture location was the anterior thoracic wall (10/14). All approaches were via VATS wedge resection. The margin was confirmed by frozen section analysis and all margin distances were greater than the lesion diameter or 20 mm. Postoperative pathological analysis of the 14 lung nodules revealed two nodules with benign tumor, one with atypical adenomatous hyperplasia, five with adenocarcinoma in situ, one with minimally invasive adenocarcinoma, and five with invasive adenocarcinoma.
In the testing period (n = 23), the sex distribution was nearly equal, with 43% male patients. The median age was 58 years (range 32–70 years). The median nodule diameter was 8.0 mm (range 4–16 mm) and the median nodule depth was 5.9 mm (range 2.0–23.5 mm). The nodules were also mainly located in the right upper lobe (12/23) and the most common percutaneous location approach was also through the anterior thoracic wall (9/23). All approaches were VATS wedge resection. The margin was confirmed by frozen section analysis and all margin distances were greater than the lesion diameter or 20 mm. Postoperative pathological analysis of the 23 lung nodules revealed two nodules with benign tumor, eight with adenocarcinoma in situ, five with minimally invasive adenocarcinoma, six with invasive adenocarcinoma, and two with metastatic adenocarcinoma.
Based on our previous experience, we considered a distance error of less than 2 cm as a successful localization. In the comparison period (n = 14), the success rates of CT-G and 3D-G were 100% and 92.9%, respectively (P = 0.31); in the testing period, the success rate of 3D-G was 95.6% (n = 23). The localization times for CT-G, 3D-G (comparison), and 3D-G (testing) were 23.6 ± 5.3, 19.3 ± 6.8, and 9.8 ± 4.6 minutes, respectively. The distance errors of localization with CT-G, 3D-G (comparison), and 3D-G (testing) were 1.6 mm (range 0–10 mm), 3.9 mm (0–12 mm), and 9.0 mm (0–30 mm), respectively (Table 2). There was one failure in the comparison period and one failure in the testing period. The reasons for localization failure are summarized in Table 3.
| Variables | Comparison period (n = 14) | P-value | Testing period (n = 23) | |
|---|---|---|---|---|
| CT-G | 3D-G | |||
| Localization time (minutes) | 23.6 ± 5.3 | 19.3 ± 6.8 | 0.07 | 9.8 ± 4.6 |
| Success rate (%) | 14/14 (100%) | 13/14 (92.9%) | 0.31 | 22/23 (95.6%) |
| Distance error (cm, range) | 1.6 (0–10) | 3.9 (0–12) | 0.12 | 9.0 (0–30) |
| Operative time (minutes) | 36.8 ± 9.1 | - | 36.1 ± 7.2 | |
| Postoperative hospitalization (days) | 1.7 ± 0.6 | - | 1.8 ± 0.6 | |
| Case number | Reason |
|---|---|
| 9 | No location site found, needle was too shallow |
| 18 | Nodule was located in the left lower lobe, large range of respiratory movement (30 mm) |
The CUSUM learning curve was best modeled by the equation: Y = 0.48X2 − 0.013X − 0.454 (R2 = 0.89) (Fig 3). The learning curve was composed of two phases (Table 4), phase 1 (the initial 20 patients) and phase 2 (the remaining 17 patients).
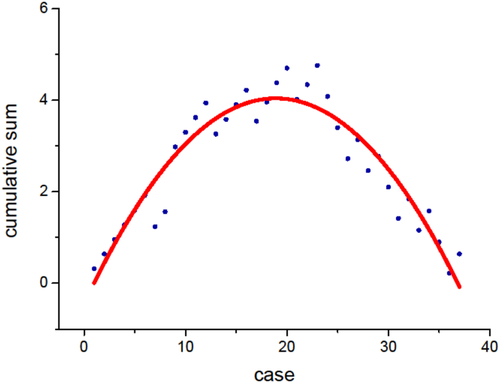
 ) Cumulative sum, (
) Cumulative sum, ( ) Polynomial fit of cumulative sum.
) Polynomial fit of cumulative sum.| Phase 1 (n = 20) | Phase 2 (n = 17) | P-value | |
|---|---|---|---|
| Age, in years (IQR) | 52 (47.5–58.5) | 58 (44–63) | 0.832 |
| Sex, n (%) | 0.815 | ||
| Male | 9 (45.0%) | 7 (41.2%) | |
| Female | 11 (55.0%) | 10 (58.8%) | |
| Smoking history, n (%) | 0.659 | ||
| Never | 14 (70.0%) | 13 (76.47%) | |
| Former/current | 6 (30.0%) | 4 (23.53%) | |
| Nodule size (mm) | 8.1 ± 3.8 | 8.5 ± 3.7 | 0.702 |
| CTR (mean, range) | 0.25 (0–1) | 0.18 (0–1) | 0.571 |
| Localization, n | |||
| RUL | 16 | 8 | |
| RML | 1 | 1 | |
| RLL | 1 | 3 | |
| LUL | 1 | 3 | |
| LLL | 1 | 2 | |
| Depth (mm) | 11.4 ± 6.5 | 10.4 ± 7.8 | 0.682 |
| Percutaneous puncture approach, n | |||
| Anterior | 13 | 6 | |
| Posterior | 6 | 3 | |
| Lateral | 1 | 8 | |
| Localization time (minutes) | 17.8 ± 6.6 | 8.2 ± 3.5 | 0.000 |
| Success rate (%) | 17/20 (85.0%) | 16/17 (94.1%) | 0.609 |
| Distance error (cm, range) | 5.4 (0–40) | 11.8 (0–70) | 0.138 |
| Operative time (minutes) | 36.5 ± 8.8 | 36.2 ± 7.0 | 0.903 |
| Postoperative hospitalization (days) | 1.7 ± 0.6 | 1.7 ± 0.6 | 0.538 |
- CTR, consolidation/tumor ratio; LLL, left lower lobe; LUL, left upper lobe; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe.
Discussion
Localization of small pulmonary nodules prior to surgery is still a clinical challenge. Localization of the target lung nodule by palpating the lung parenchyma is time consuming. Failure to localize nodules can result in an unplanned anatomic segmentectomy or lobectomy. Suzuki et al. reported that if the target nodule is smaller than 10 mm in diameter and the distance to the pleura more than 10 mm, blind localization would be a high-risk approach.11 In our study, although there was one failure in the comparison period and one failure in the testing period, the new approach (3D-G localization) obtained results similar to traditional methods; frozen section analysis revealed that all nodules were resected with safe margins. This new approach is highly dependent on the surgeon. The surgeon must carefully identify the patient's anatomical landmarks to ensure precise placement of the navigational template. According to our CUSUM learning curve, the actual 3D-G localization procedure is not very difficult for surgeons with minimal experience in this procedure. We observed that the success rates and localization time become stable after performing 3D localization in 20 cases. Compared to CT-G localization, we consider 3D-G localization to be easy to use, simple to operate, and will save resources and time. In contrast to traditional localization methods, 3D printing localization is performed in the operating room while the patient is under general anesthesia. The transit time from radiology to the operating room is eliminated and patients do not experience fear and pain. CT-G percutaneous hookwire has easy procedures and safe material, although it may cause complications12 such as pain, pneumothorax, bleeding, hooks shift, and even air embolism.13 CT-G injection of methylene blue dye is simple to perform, and the material is both safe and inexpensive. However, carbon deposition and pigmentation on the surface of lung tissue interfere with the determination of the staining range. Unfortunately, methylene blue dye diffuses easily after percutaneous injection and surgery should be performed within a few hours, or as soon as possible. Lipiodol has been reported to have favorable factors include less diffusion and long presentation (even greater than three months) but there is a risk of causing allergies and embolism if this contrast agent accidentally reached the systemic circulation.14 In addition, the CT-G localization methods have common deficiencies,15-17 such as physical discomfort, psychological stress, ionizing radiation exposure, occupying radiology resources and increasing the burden of logistics department. Virtual-assisted lung mapping (VAL-MAP) is a preoperative bronchoscopic multispot dye-marking technique using virtual images.18 Its safety, efficacy and reproducibility had been previously demonstrated in a multicenter study.19 The learning curve of this method was higher, and the localization time was longer than conventional CT-G localization. However, unexpected hypertension or hypoxemia could occur during the procedure and cause serious medical problems.19 Electromagnetic navigation bronchoscopy (ENB) has been proven to be useful for biopsy of peripheral lung lesions,20 and as a novel technique for the diagnosis and localization of small peripheral lesions.21 Electromagnetic board and sensor probe have been reported to allow the position of the probe to be detected and displayed in real time on a 3D virtual image, and the dye has been injected through the natural lumen to achieve the purpose of locating small nodules.20, 22 Because of general anesthesia, the patient would not feel any discomfort associated with the localization procedure. In localization, the high success rate and safety of ENB have been confirmed in several studies.23-25 This technique also requires training and practice, and its success rate is closely related to the operator's proficiency.26
Localization failed in two cases; in the first case (case No. 9), the localization site could not be found during surgery, as the needle was too shallow; in the second case (case No. 18), localization failed due to respiratory movement, as the tumor was located in the lower lobe. Some issues were difficult to completely avoid; for example, there was a negative effect of the respiratory cycle, especially for localizations in the lower lobe. Moreover, we presumed that the percutaneous puncture approach through the anterior thoracic wall would be technically easier and more accurate than the lateral or posterior approach, due to the adjusted patient position. If the puncture site is located in the anterior thoracic wall, the patient is in the supine position during the localization, which is identical to the CT scan position. Furthermore, the depth of the percutaneous puncture would change under different positions because of changes at the site of the puncture, especially when the posterior thoracic wall is chosen as the percutaneous puncture point. With the change in position, the skin will collapse and accumulate, which would change the depth of the percutaneous puncture significantly, which can lead to a failure to localize the nodule.
As this is a preliminary feasibility study, we acknowledge that there are several limitations, including its small sample size and subjective bias. Moreover, this technique remains an immature procedure, and a backup operation plan needs to be in place if localization fails.
In conclusion, we demonstrated that the 3D printing localization technique has high accuracy for localization of small pulmonary nodules, especially in the right upper lobe. The technology is a feasible and accessible strategy to localize nonpalpable pulmonary nodules.
Acknowledgments
We would like to thank the patients and their families for making this study possible. This work was supported by the National Natural Science Foundation of China (Grant No. 81673031&No. 81872510), Research Fund from Guangzhou Science and Technology Bureau (Grant No. 201704020161), High-level Hospital Construction Project (DFJH201801), Guangdong Provincial People's Hospital Young Talent Project (No. GDPPHYTP201902), Guangdong Provincial Key Laboratory of Lung Cancer Translational Medicine (No. 2017B030314120) and the Natural Science Foundation of Guangdong Province (10451008002006285). The funding sources had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Disclosure
The authors declare that there are no conflicts of interest.