Targeted treatment strategy for patients with severe pulmonary hypertension secondary to connective tissue diseases
Bo Jiang and Chun Wang contributed equally to this study.
Abstract
Background
Pulmonary arterial hypertension (PAH) associated with connective tissue diseases (CTD) (CTD-PAH) remains a difficult challenge in clinical practice. We aimed to evaluate the effects of targeted vasodilators in patients with severe CTD-PAH.
Methods
The data of 53 patients with severe CTD-PAH hospitalized at the Department of Rheumatology and Immunology, The Affiliated Drum Tower Hospital of Nanjing University Medical School, were retrospectively reviewed. Patients were followed up for an average of 2 years to track their outcomes. The efficacy of treatment and the survival rate of patients with severe CTD-PAH were determined.
Results
Among the causes of severe CTD-PAH, systemic lupus erythematosus (SLE) was the most common (39.6%), and the age at onset in patients with SLE-PAH was younger than that of patients with other CTD. Bosentan was more effective than sildenafil in reducing pulmonary artery pressure, improving cardiac function, and increasing survival time. Combination therapy with targeted vasodilators significantly improved the prognosis of patients with severe CTD-PAH compared with monotherapy.
Conclusions
Patients with severe CTD-PAH should be treated early with targeted vasodilators. In this study, bosentan was superior to sildenafil. Combined treatment might be an option for severe CTD-PAH.
Key points
-
This study showed that bosentan is more effective than sildenafil in the treatment of patients with severe pulmonary arterial hypertension associated with connective tissue diseases (CTD-PAH).
-
The findings are important for the clinical choice of targeted vasodilators for CTD-PAH.
1 INTRODUCTION
Pulmonary arterial hypertension (PAH) associated with connective tissue diseases (CTD) (CTD-PAH) remains a difficult challenge in clinical practice. Previous studies by Chinese scholars have shown that approximately 3.7%–8.3% of patients with CTD develop PAH,1, 2 and CTDs are the third leading cause of PAH in China. However, this rate is lower than that in European patients with CTD, as shown in DETECT.3 Without treatment, PAH can lead to severe right-sided heart failure and early death. Evidence suggests that intensive immunosuppressive therapy improves pulmonary hemodynamics and long-term prognosis in patients with CTD-PAH, especially in the early stage.4 However, the prognosis of severe CTD-PAH is still poor; therefore, severe CTD-PAH has a high mortality rate.
Recently, targeted vasodilators have been found to significantly improve patients' outcomes, with the 1-year survival rate for systemic sclerosis (SSc)-PAH increasing from 50% to 90%.5 Several clinical trials have suggested that both bosentan,6, 7 a dual endothelin receptor antagonist (ERA), and sildenafil,8, 9 a phosphodiesterase type-5 (PDE5) inhibitor, improve clinical symptoms, hemodynamics, and pulmonary artery pressure (PAP) in Chinese patients with PAH. The latest Chinese guideline on PAH in 2018 recommends ERAs and PDE5 inhibitors for the treatment of CTD-PAH.10 However, there are no clinical studies on the efficacy of various treatments in Chinese patients with severe CTD-PAH. Therefore, how to choose the best first-line vasodilators in patients with CTD-PAH is still an important clinical question without definitive international recommendations. In this study, we assessed the therapeutic efficacy of targeted vasodilators in patients with severe CTD-PAH.
2 METHODS
2.1 Patients
A total of 53 hospitalized patients with severe CTD-PAH at the Department of Rheumatology and Immunology of Nanjing Drum Tower Hospital from December 2015 to December 2018 were recruited. The diagnosis of CTD fulfilled 1997 American College of Rheumatology (ACR)11 or 2012 Systemic Lupus International Collaborating Clinics criteria for systemic lupus erythematosus (SLE)12; the 2002 International Classification Criteria for Sjögren's syndrome (SS)13; the 1987 Sharp criteria for mixed connective tissue disease (MCTD)14; the 1980 ACR criteria15 or 2013 ACR/European League Against Rheumatism criteria for SSc16; the 1987 ACR criteria for rheumatoid arthritis (RA)17; and the 1975 Bohan/Peter criteria for polymyositis (PM) and dermatomyositis (DM).18 Pulmonary artery systolic pressure (PASP) was measured by transthoracic cardiac ultrasound in the resting state. According to 2015 or 2022 European Society of Cardiology/European Respiratory Society guidelines, PAH was defined as a mean PAP of ≥25 or ≥20 mmHg at rest, in addition to a pulmonary capillary wedge pressure of ≤15 mmHg and a pulmonary vascular resistance of >3 Wood units. Under normal conditions, PAP measured by echocardiography is approximately 10–15 mmHg higher than that measured by right heart catheterization. When PAP is above 36 mmHg, echocardiography has high specificity and sensitivity for detecting PAH.19 In this study, severe PAH was defined as a PASP of ≥70 mmHg (PASP = 4 × (maximal tricuspid regurgitation velocity)2 + right atrial pressure) measured by echocardiography according to the cardiac ultrasound classification of pulmonary hypertension (PH).20 At the same time, echocardiographic, chest computed tomography (CT), anticardiolipin antibody, and pulmonary artery (PA) CT angiography were used to exclude group 2, 3, and 4 PH. Patients with ischemic heart disease, valvular heart disease, viral myocarditis, dilated cardiomyopathy, hypertrophic cardiomyopathy, chronic obstructive pulmonary disease, pulmonary thromboembolism, lung cancer, congenital pulmonary disease, and human immunodeficiency virus were excluded.
Cardiac functional grading was performed by the conventional New York Heart Association (NYHA) functional classification. Interstitial lung disease (ILD) and its severity were judged by radiologists and respiratory specialists according to chest CT and lung function testing in patients with CTD. The serum B-type natriuretic peptide (BNP) concentration was measured using an immunofluorescence assay. The 6-min walk distance (6MWD), right ventricular function, and morphological indices were measured by echocardiography, except in patients with poor cardiac function.
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital (No. 2020-093-01). Written informed consent was obtained from all participants to use their clinical and laboratory data.
2.2 Data collection
The patients' clinical data on admission, including sex, age, disease entity, duration, use of targeted vasodilators and immunosuppressants, PASP, and NYHA class, were collected. Patients were followed up every 3–6 for 12–58 months (bosentan group: 25.38 ± 15.35 months; sildenafil group: 21.25 ± 13.71 months) to track their survival status, PASP, and cardiac function.
All patients were treated with targeted vasodilators. The effect of beraprost monotherapy (20–40 µg, three times per day) is poor for severe PAH in clinical practice, so it is mostly taken as the concomitant drug with bosentan or sildenafil at our center. The choice of bosentan or sildenafil was made according to the financial status and severity of PAH of the patients. The 53 patients were divided into two groups: the bosentan group (n = 18) and the sildenafil group (n = 35). The dose of bosentan was 62.5 mg twice per day for 1 month, which was then upregulated to 125 mg twice per day. The dose of sildenafil was 25 mg three times per day.
In addition to targeted therapy, almost all patients were treated with glucocorticoid (GC) (0.5–1 mg/kg daily with gradual tapering) and immunosuppressants for CTD. The dose of GC and the choice of immunosuppressant depended on the severity and activity of CTD. Cyclophosphamide (CTX) was administered intermittently (0.4 g by an intravenous infusion twice per month) and gradually reduced in most patients with severe disease, but it was not taken in patients with fertility requirements or intolerance to the side effects of CTX, such as digestive tract reactions. Similar to CTX, mycophenolate mofetil (MMF) (1.5–2.0 g/day) was mostly used in more severe and acute aggravated cases. Leflunomide (LEF) (20 mg/day), Tripterygium wilfordii (TW) (30–60 mg/day), hydroxychloroquine sulfate (HCQ) (0.4 g/day), and FK 506 (3–4 mg/day) were also taken by some patients with relatively mild disease. In the bosentan group, 16 patients were treated with CTX, one patient was treated with TW, and one patient was treated with MMF. In the sildenafil group, 17 patients were treated with CTX, seven patients were treated with MMF, two patients were treated with TW, one patient was treated with FK506, two patients were treated with LEF, and three patients were treated with HCQ, while three patients were not treated with any immunosuppressants. The exact therapies of all patients are listed in Table 1.
| Groups | Bosentan group | Sildenafil group |
|---|---|---|
| Total patients (n) | 18 | 35 |
| Age (years), mean ± SD (range) | 38.2 ± 3.0 (24.0–77.0) | 43.9 ± 2.9 (21.0–79.0) |
| Female:male (n) | 18:0 | 34:1 |
| SLE (n) | 8 | 13 |
| SS (n) | 5 | 7 |
| SSc (n) | 1 | 5 |
| Mixed CTD (n) | 3 | 2 |
| RA (n) | 1 | 4 |
| PM/DM (n) | 0 | 4 |
| Average PASP (mmHg), mean ± SD | 91.56 ± 3.61 | 80.44 ± 2.74 |
| CTD duration (years), mean ± SD | 6.33 ± 0.80 | 8.43 ± 1.02 |
| PAH duration (years), mean ± SD | 2.59 ± 0.47 | 1.78 ± 0.26 |
| With obvious ILD (n) | 6 | 18 |
| Basic WHO function class (before targeted drug treatment) (n) | ||
| I | 0 | 1 |
| II | 1 | 9 |
| III | 14 | 17 |
| IV | 3 | 8 |
| Immunosuppressive drug (n) | ||
| CTX | 16 | 17 |
| MMF | 1 | 7 |
| Tripterygium wilfordii | 1 | 2 |
| LEF | 0 | 2 |
| FK506 | 0 | 1 |
| HCQ | 0 | 3 |
| None | 0 | 3 |
| Targeting drug (n) | ||
| Single drug | 2 | 12 |
| Bosentan + sildenafil | 4 | 0 |
| Bosentan/sildenafil + beraprost sodium | 4 | 23 |
| Bosentan + sildenafil + beraprost sodium | 8 | 0 |
| Follow-up duration (months), mean ± SD | 25.38 ± 15.35 | 21.25 ± 13.71 |
| Poor prognosis (n) | ||
| Died of heart failure | 1 | 11 |
| Died of other reason | 1 | 1 |
| Lost contact | 1 | 0 |
- Abbreviations: CTD, connective tissue disease; CTX, cyclophosphamide; DM, dermatomyositis; HCQ, hydroxychloroquine sulfate; LEF, leflunomide; MMF, mycophenolate mofetil; PAH, pulmonary arterial hypertension; PM, polymyositis; RA, rheumatoid arthritis; SD: standard deviation; SLE, systemic lupus erythematosus; SS, Sjogren's syndrome; SSc, systemic sclerosis.
2.3 Statistical analysis
The data are presented as the mean ± standard deviation (parametric data) or as the median (25th, 75th percentiles) (categorical variables). Continuous variables were compared between the two groups using the unpaired t-test (parametric data) or the Mann–Whitney U-test (nonparametric data). The χ2 test was used to compare categorical data. Survival curves were constructed using the log-rank (Mantel–Cox) test and the Gehan–Breslow–Wilcoxon test. A two-tailed p value of <0.05 was considered statistically significant. All statistical calculations were performed using SPSS software (version 20.0; IBM Corp.).
3 RESULTS
3.1 Demographics of the patients with severe CTD-PAH
Among the 53 patients with severe CTD-PAH, SLE was present in 21 patients (39.6%), SS was present in 12 patients (22.6%), SSc was present in six patients (11.3%), MCTD was present in five patients (9.4%), RA was present in five patients (9.4%), and PM/DM was present in four patients (7.5%) (Tables 1 and 2). Overall, 98.1% of the patients were female. There was no difference in the mean age of the patients between the bosentan group and the sildenafil group (p = 0.1344). Although the duration of CTD (p = 0.1807), duration of PAH (p = 0.1097), and NYHA class (median [25th, 75th percentiles] = 3 [2, 3] vs. 3 [3, 3], p = 0.5801) showed no obvious difference between the two groups, the average baseline PASP (91.56 ± 3.61 vs. 80.44 ± 2.74 mmHg, p = 0.0181) was significantly higher in the bosentan group than that in the sildenafil group (Table 1). CTX was the most commonly used immune suppressor (62.2%). In total, 12 patients died of heart failure, two patients died of other causes, and one patient lost contact during follow-up.
3.2 Factors related to the prognosis of severe CTD-PAH
3.2.1 CTD entity
Among the patients with severe CTD-PAH, SLE was the most common cause (39.6%). The average age at onset of SLE-PAH (32.7 ± 8.2 years) was much younger than that of other types of CTD-PAH (38.6–51.0 years) (Table 2). The mortality rate due to PAH was 33.3% in patients with SSc, which was the highest among all CTDs, but the average PASP in patients with SSc was low (80.2 mmHg) (Table 2), suggesting that SSc-PAH had the poorest prognosis.
| Items | SLE | SS | SSc | MCTD | RA | PM/DM |
|---|---|---|---|---|---|---|
| Patients (n) | 21 | 12 | 6 | 5 | 5 | 4 |
| Percentage (%) in total CTD-PAH group | 39.6* | 22.6 | 11.3 | 9.4 | 9.4 | 7.5 |
| Average onset age of PAH (years) | 32.7** | 46.8 | 51.0 | 38.6 | 45.0 | 47.0 |
| Average PAH duration (year) | 2.31 | 1.67 | 2.42 | 2.50 | 2.20 | 0.53 |
| Average onset time of PAH after CTD (years) | 4.48 | 3.79 | 4.75 | 4.70 | 15.80 | 7.63 |
| Average PASP (mmHg) | 82.6 | 84.1 | 80.2 | 86.0 | 79.8 | 82.0 |
| Died of heart failure or lost contact (%) | 23.8 | 25.0 | 33.3 | 20 | 20 | 25 |
- Abbreviations: CTD, connective tissue disease; DM, dermatomyositis; MCTD, mixed connective tissue disease; PAH, pulmonary arterial hypertension; PASP, pulmonary artery systolic pressure; PM, polymyositis; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; SS, Sjogren's syndrome; SSc, systemic sclerosis.
- * p = 0.0157
- ** p = 0.0074.
3.2.2 Baseline PAP and NYHA functional class
The average baseline PASP of the 12 patients who died from heart failure was higher than that of the surviving patients (90.62 ± 4.59 vs. 81.11 ± 2.62 mmHg, p = 0.0376) in all CTD patients, while the NYHA class was not significantly different (3 [3, 3] vs. 3 [3, 3], p = 0.5573]. Therefore, the PASP of patients with severe CTD-PAH before treatment was related to prognosis.
3.2.3 ILD
Of the study population, 24 patients had obvious ILD (six patients in the bosentan group and 18 patients in the sildenafil group); the other patients had no or mild ILD. The PAH duration (1.90 ± 0.33 vs. 2.21 ± 0.36 years, p = 0.5356), baseline PASP (82.08 ± 3.15 vs. 84.71 ± 3.02 mmHg, p = 0.5492), baseline NYHA functional class (3 [3, 3] vs. 3 [2, 4], p = 0.3835], and the percentage of patients who died from PAH (28.5% vs. 22.2%, p = 0.7340) were not significantly different between patients with obvious ILD and patients without obvious ILD. The decrease in PASP in the group with CTD without obvious ILD (6.75 ± 4.19 mmHg) was more evident than that of the group with CTD with ILD (2.80 ± 4.49 mmHg) after targeted therapy. This suggests that the effect of targeted therapy may be weaker in group 3 PH with lung diseases.
3.2.4 Immunosuppressants
Compared with the sildenafil group, CTX was more frequently taken in the bosentan group (88.9% vs. 48.6%, χ2 = 8.224, p = 0.0063), and the rate of mortality due to heart failure was significantly lower (5.5% vs. 31.4%, χ2 = 4.543, p = 0.0331). The proportion of patients treated with CTX who survived was higher than the proportion of patients who died (70.2% vs. 35.7%, χ2 = 5.088, p = 0.012). CTX more obviously decreased PASP (p = 0.0298), NYHA class (p = 0.0113), and mortality due to heart failure (CTX, 12.5% vs. other immunosuppressors, 33.3%) than other immune suppressors, including MMF, TW, LEF, FK506, and HCQ (data not shown).
3.3 Targeted vasodilators for severe CTD-PAH
During follow-up, only one 77-year-old patient with SSc in the bosentan group died of heart failure 3 years later, whose baseline PASP was 98 mmHg. One patient with MCTD died of gastric perforation, and one 26-year-old patient with SLE lost contact 1 year later, whose baseline PASP was 117 mmHg (Table 1). However, in the sildenafil group, 11 patients died of heart failure, including four patients with SLE (average baseline PASP = 85.2 mmHg), four patients with SS (average baseline PASP = 89.5 mmHg), one patient with SSc (whose baseline PASP was 98 mmHg), one patient with PM/DM (whose baseline PASP was 108 mmHg), and one patient with MCTD (whose baseline PASP was 70 mmHg). Among the deceased patients in the sildenafil group, the PASP of two patients was obviously decreased (115–98 and 101–85 mmHg). One patient with RA died due to a tumor with liver cirrhosis (Table 1). Mortality due to PAH (heart failure) in the bosentan group was much lower than that in the sildenafil group (χ2 = 4.543, p = 0.0331), in spite of the significantly higher baseline PASP (91.56 ± 3.61 vs. 80.44 ± 2.74 mmHg, p = 0.0181) before targeted drug treatment.
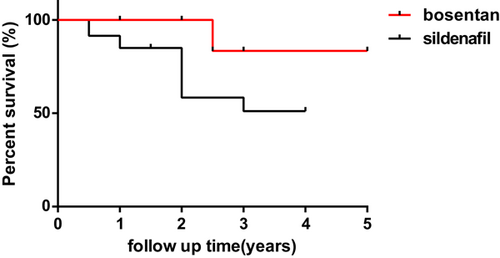
Figure 1 shows the survival curves of patients in the bosentan and sildenafil groups. The 1-, 2-, and 3-year survival rates were 100% versus 84.9%, 100% versus 58.4%, and 83.3% versus 51.1% in the bosentan and sildenafil groups, respectively. The log-rank (Mantel–Cox) test (p = 0.0402) and the Gehan–Breslow–Wilcoxon test (p = 0.0309) indicated better survival in the bosentan group.
The average PASP of patients treated with bosentan was significantly reduced (91.56 ± 3.61 vs. 81.38 ± 3.67 mmHg, p = 0.0292). Despite the lower initial average PASP in the sildenafil group than that in the bosentan group, sildenafil did not effectively decrease PASP (80.44 ± 2.74 vs. 78.32 ± 4.00 mmHg, p = 0.8290). Bosentan evidently decreased NYHA functional class (3 [3, 3] vs. 2 [2, 3], p < 0.0001]. Although the initial cardiac function of patients treated with sildenafil was better than that of patients treated with bosentan at the beginning, NYHA class increased slightly after sildenafil treatment (3 [3, 3] to 3 [3, 4], p = 0.8752). There was a significant difference between the change in NYHA class in the bosentan group and the sildenafil group (−1 [0–0] vs. 0 [−1 to 1], p = 0.0007). The results also show that bosentan had better efficacy than sildenafil in decreasing BNP concentration, increasing 6MWD (Supporting Information: Figure S1), and decreasing PA diameter (data not shown).
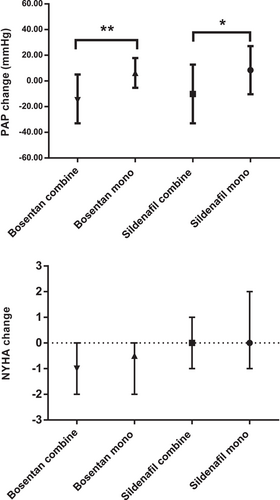
3.4 Combined use of targeted vasodilators improves prognosis
Combination therapy with targeted vasodilators was more effective in decreasing PASP than monotherapy, both in the bosentan (p = 0.0066) and sildenafil (p = 0.0217) groups (Figure 2). Combination therapy was better in reducing NYHA functional class than monotherapy, although the difference was not significant (Figure 2). Compared with the sildenafil group, more patients in the bosentan group were treated with combination therapy (88.9% vs. 65.7%) and demonstrated better survival. In the bosentan group, only one patient who died of heart failure was treated with bosentan alone. In the sildenafil group, mortality due to heart failure among the patients treated with combination therapy (sildenafil + beraprost) was much lower than that of patients with sildenafil alone (4/23 [17.4%] vs. 7/12 [58.3%], p = 0.0133).
4 DISCUSSION
Among the patients with severe CTD-PAH at our center, the prevalence of SLE (39.6%) and SS (22.6%) was the highest. These results differ from the largest international PAH study (REVEAL, Registry to Evaluate Early and Long-term PAH Disease Management), in which the frequency of PAH in patients with SSc (67.7%) was the highest and the frequency of PAH in patients with SLE was the lowest (18.7%).21 However, our results are consistent with a previous study conducted in China.22 This may be due to the higher incidence of SLE and SS in China. We also found that the patients with severe SLE-PAH were the youngest among all patients with CTD-PAH, indicating the early development of PAH in SLE. Similar to other studies,23, 24 the mortality of PAH secondary to SSc was the highest in the present study. Therefore, the primary autoimmune disease is relevant to the occurrence and prognosis of PAH. Noninvasive cardiac ultrasound should be performed frequently to screen for PAH in patients with CTD, especially SLE and SSc, for the purpose of early intervention and to prolong the survival time.
The results of this study indicate that high-risk factors for a poor prognosis in patients with severe CTD-PAH include a high baseline PAP, nonuse of CTX, and noncombination use of targeted vasodilators. CTX has demonstrated efficacy for the treatment of CTD-PAH4 and is recommended as the first choice of immunosuppressant therapy in Chinese PAH guidelines.10 Therefore, patients with severe CTD-PAH with cardiac insufficiency III–IV should be frequently monitored; should take strong immunosuppressive agents, such as CTX; and should be initially treated with targeted drugs. It seems that ILD does not affect the prognosis of CTD-PAH. To confirm the above speculation, studies with a large number of patients with CTD-PAH are required.
At present, regularly used targeted vasodilators for PAH in China include bosentan (ERA), sildenafil (PDE5 inhibitor), and beraprost (prostacyclin analog). High-dose beraprost often causes side effects, such as flushing and headache, and has limited benefit for severe PAH.25 Therefore, beraprost is usually taken as a component of combination therapy with bosentan or sildenafil. Other prostacyclin analogs, such as epoprostenol or treprostinil, are too expensive for most Chinese patients. In the present study, we evaluated the efficacy of bosentan and sildenafil in reducing PASP, improving cardiac function, and increasing survival in patients with severe CTD-PAH. No significant improvement was observed in the sildenafil group, which might be ascribed to more severe illness in the enrolled patients than in other studies. In contrast, bosentan more significantly relieved the illness of patients with more severe CTD-PAH than sildenafil. The results demonstrate that bosentan greatly reduced PASP, NYHA class, and mortality in patients with severe CTD-PAH. Bosentan also showed better efficacy in reducing the BNP concentration, increasing 6MWD, and decreasing the PA diameter, though the difference was not very significant. Compared with the sildenafil group, the survival rate in the bosentan group was significantly higher, especially at 2–4 years of follow-up. In summary, the curative benefit of bosentan was considered superior to sildenafil for severe CTD-PAH. A previous meta-analysis of 24 studies on patients with group 1 PH showed that bosentan was more effective than sildenafil in decreasing clinical worsening (odds ratio 0.21 vs. 0.31).26 The present study is a retrospective analysis of real-world data; therefore, the distribution of CTD types, the proportion of patients treated with CTX, and the proportion of patients taking combination therapy in the sildenafil and bosentan groups were different, which may have led to some bias. In future research, we will attempt to balance the different study groups to prevent such bias in the statistical results. No obvious side effects occurred in this study, with the exception of one case of mild epistaxis in a patient treated with sildenafil. In addition to the Chinese economic condition, considering the efficacy, we recommend the use of PDE5 inhibitors or prostacyclin analogs for mild-to-moderate PAH. However, we recommend ERAs as the first-line treatment for severe CTD-PAH (i.e., NYHA class III–IV) rather than PDE5 inhibitors.
Combination therapy with targeted vasodilators has theoretical basis because they target various pathogenic pathways in PAH. A previous study conducted in China showed that the combination of beraprost with sildenafil was more effective in improving 6MWD and event-free survival than sildenafil alone.27 Although bosentan reduced the plasma concentration of sildenafil, the efficacy of sildenafil in reducing PASP and increasing the cardiac index was maintained in patients with PAH.28 In another study, bosentan combined with sildenafil increased 6MWD more evidently than sildenafil alone.29 A meta-analysis conducted by Chinese researchers on PAH also examined the efficacy of different medications for improving 6MWD, with the following results: bosentan + sildenafil (Surface Under the Cumulative RAnking curve [SUCRA] of 82.9%) > bosentan alone (49.2%) > sildenafil alone (48.5%).30 Another meta-analysis included 40 studies and showed that for 6MWD, bosentan + sildenafil (weighted mean difference [WMD] 98.53, SUCRA of 99%) was more effective than sildenafil (WMD 79.24, SUCRA of 87.5%) or bosentan (WMD 55.68, SUCRA of 70%). Moreover, bosentan + sildenafil (WMD −10.8, SUCRA of 84.4%) was more effective than bosentan (WMD 5.89, SUCRA of 61.3%) in reducing the average PAP.26 In newborn patients with PAH, the average length of hospital stay (days) in the sildenafil + bosentan group was much shorter than in the sildenafil alone group.31 In terms of clinical worsening, bosentan combined with sildenafil was better than sildenafil alone (odds ratio 0.21 vs. 0.33).30 Initial combination of at least two of iloprost, bosentan, and sildenafil has been reported to improve short-term survival.8 Our results confirm that the combination of two or three targeted drugs (bosentan, sildenafil, and beraprost) was more effective in decreasing PAP, improving cardiac function, and decreasing mortality. The side effects did not increase with combination therapy (data not shown). The combination of targeted vasodilators has two schemes: initial combination and sequential combination. The former is more frequently used at our hospital. An increasing number of guidelines for PH have been published in recent years, such as the 2018 ACCP guideline,32 the 2021 Chinese guideline by the Chinese Thoracic Society,33 and the Chinese expert consensus for CTD-PAH in 2021.34 The common opinion is that initially targeted drug combinations, such as ambrisentan + tadalafil, for severe adult PAH (World Health Organization grade ≥ II) should be used, with recommendations for bosentan and sildenafil. Therefore, we recommend that for severe CTD-PAH, the preferred choice should be early combined use of bosentan and sildenafil. Alternative options are bosentan plus beraprost or sildenafil plus beraprost.
In conclusion, patients with CTD, especially SLE and SSc, should be closely monitored by echocardiography to diagnose and treat PAH early. The treatment of patients with severe CTD-PAH should be improved and should include early and adequate usage of targeted vasodilators and combination therapy, in which bosentan is preferred over sildenafil, and routine treatment with GC and strong immunosuppressants, in particular, CTX. However, the number of enrolled patients with severe CTD-PAH was not very large in the present study. In the future, a prospective, controlled, large-sample study on CTD-PAH with a prolonged follow-up period should be performed to obtain more credible results and to provide guidance for clinical practice.
AUTHOR CONTRIBUTIONS
Bo Jiang contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Bo Jiang, Chun Wang, Yansheng Jin, and Kangxing Zhou. The first draft of the manuscript was written by Bo Jiang. Genhong Yao and Xuebing Feng edited the manuscript. Cardiac ultrasound was mainly operated by Guanjun Guo. All authors have read, approved, and agreed to take full responsibility for all aspects of the final manuscript. All authors have confidence in the integrity of their contributions.
ACKNOWLEDGMENTS
This work was supported by the Nanjing Science and Technology Development Plan (No. 201715021); the PANDA Project 2018-Clinical Research Special Fund of China Foundation for International Medical Exchange (No. Z-2014-06-2-1863); the Clinical Research Special fund of Nanjing Drum Tower Hospital (No. 2022-LCYJ-MS-39); and the Chinese Hospital Reform and Development Research Institute Project of Nanjing University (No. NDYG2022047).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital (No. 2020-093-01) and conforms to the Declaration of Helsinki.
Open Research
DATA AVAILABILITY STATEMENT
The data in the current study are available from the corresponding author upon reasonable request.