Inflammatory phenotype of osteoarthritis and its potential therapies
Abstract
Introduction
Osteoarthritis (OA) is the most common joint disorder in the world but there are no approved therapies to slow disease progression. Historically, OA has been considered a wear and tear joint disease and efforts to identify and develop disease modifying therapies have primarily focused on inhibiting cartilage degradation directly. However, increasing studies have suggested that inflammation is a key player of joint pathology in some OA patients and also a link between obesity and OA. Therefore, targeting inflammation in these patients could be a promising therapeutic strategy.
Areas Covered
In this review, we collate the latest evidence on the relationship between inflammation and OA which allows to propose the inflammatory phenotype of OA, and summarize major results of some emerging therapies targeting this phenotype in clinical trials which could implicate future directions for OA treatment.
Expert Opinion
The authors believe early diagnosis, phenotyping OA patients and precise therapies would expedite the development of DMOADs targeting OA inflammatory phenotype. In the future, well-designed clinical trials including appropriate subgroups or phenotypes of patients according to underlying causes and mechanisms of OA are expected for investigational therapies.
Highlights
-
This review summarize the major results of some emerging therapies targeting inflammatory phenotype in clinical trials, implying future directions for OA treatment.
-
This work provide a new perspective to develop true DMOADs that target the OA inflammatory phenotype.
1 INTRODUCTION
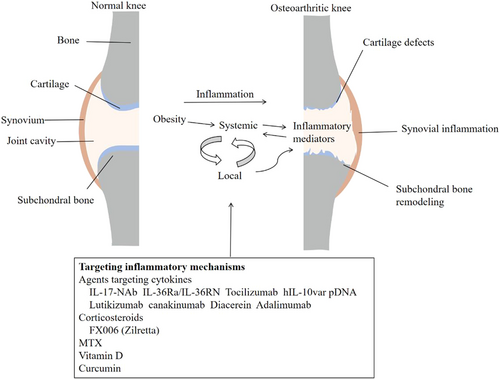
Osteoarthritis (OA) is viewed as a whole-organ disease of the joint, including degradation of cartilage, remodeling of subchondral bone, formation of ectopic bone, meniscal damage, deterioration of tendons and ligaments, and inflammation of the synovial lining.1-3 It is associated with chronic pain, joint function impairment, and disability, resulting in worsened quality of life and significant socioeconomic burdens worldwide.4, 5 On the basis of its multiple pathological features, OA is divided into different phenotypes, such as synovial inflammatory phenotype, osteoporotic phenotype, articular cartilage degradation phenotype, and metabolic phenotype.6, 7 Although the pathogenesis of OA is unclear, growing evidence indicates that inflammation plays an integral role in its pathogenesis.8, 9 In other words, OA is a whole-joint disease in which inflammation can lead to many pathological changes in certain patients (Figure 1).
The inflammation in OA differs from that in rheumatoid arthritis and other autoimmune diseases, because it is chronic, low-grade, and predominantly mediated by the innate immune system.10, 11 Current therapies mainly concentrate on pain management together with rehabilitation and exercise strategies. For advanced cases, joint replacement surgery is the only option.12-14 Hence, there is an unmet need to develop effective and safe drugs that can prevent or slow the progression of OA. Given the critical role of low-grade inflammation in OA, novel anti-inflammatory therapeutic agents could offer new opportunities for the treatment of this disease.15, 16 In OA-related research, there has been a strong focus on the identification of OA inflammation that contributes to the balance between anabolism and catabolism in articular cartilage in the inflammatory phenotype.
2 INFLAMMATORY PHENOTYPE OF OA
The inflammatory process has been overlooked for many years in research on the pathogenesis of OA.9, 17 Recent studies have consistently revealed that both local and systemic inflammation play critical roles in the onset and progression of OA.18 Synovial fluid effusion and synovitis represent partial inflammation within the knee joint and are universal in patients with symptomatic and radiographic knee OA.19, 20 Effusion–synovitis visualized on magnetic resonance imaging and ultrasonography is closely correlated with structural and clinical measures of OA, including total knee replacement.21-23 Likewise, Hoffa-synovitis can strongly predict the development of incident radiographic knee OA.24
In addition to local inflammation in the joint, systemic inflammation has an important role in OA pathogenesis.9 For example, obesity can predispose individuals to OA,17, 25, 26 not only by increasing the mechanical load on joints but also by causing chronic systemic inflammation through inflammatory mediators (proinflammatory cytokines, adipokines, alarmins) that are produced by adipose tissue and released into the bloodstream.27, 28 Proinflammatory cytokines, including interleukin (IL)-1β, tumor necrosis factor (TNF)-α, and IL-6, contributed to progressive cartilage loss in OA29 and were positively associated with changes in knee pain.30 A meta-analysis demonstrated that serum high-sensitivity C-reactive protein was upregulated in OA patients compared with control participants.31 Moreover, weight loss was associated with significantly lower systemic levels of C-reactive protein and IL-6 in OA patients, and may prevent OA onset or alleviate existing OA symptoms.32 Furthermore, serum IL-17F and IL-23 predicted increased knee bone marrow lesion (BML) scores in women, suggesting involvement of inflammation in BML pathogenesis in knee OA, particularly in women.33 Our preliminary research results suggested that serum S100A8/A9 in patients with knee OA was positively correlated with total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, cartilage defects, and serum matrix metalloproteinase 3 (MMP3).34 Our recently published article indicated that serum IL-10 and IL-12 were associated with increased cartilage volume and decreased effusion–synovitis and WOMAC scores, while leptin, adipsin, and C-reactive protein were positively associated with WOMAC scores.35 Thus, it is possible that systemic inflammation, which is associated with chronic inflammatory states like obesity and certain chronic diseases, promotes local inflammation in joints that ultimately leads to the inflammatory phenotype of OA.
3 ANTI-INFLAMMATORY THERAPEUTIC AGENTS FOR OA
Because efforts to develop effective disease-modifying OA therapies against major inflammatory targets have not borne fruit, ongoing research is essential to better understand the inflammatory response in OA joint tissues and identify new drug targets.6, 16 A number of different therapeutic approaches are currently under investigation that may eventually provide effective anti-inflammatory therapies for OA patients (Table 1). These approaches are summarized below.
| Type of drug | Route of administration | Major findings | The current phase of development | References |
|---|---|---|---|---|
| Agents targeting cytokines | ||||
| IL-17-NAb | Intra-articular | Il-17-NAb could significantly reduce joint degeneration and relieve pain in the OA animal model | – | [36] |
| IL-36Ra/RN | Intra-articular | IL-36Ra/RN showed greater improvements in OA development in mice and human OA chondrocytes | – | [37] |
| Tocilizumab | Intraperitoneal injection | Tocilizumab contributed to cartilage preservation and increased bone volume in the ischemic osteonecrosis mice model, and reduced cartilage damage and synovitis in a mouse model of DMM-induced OA | – | [38] |
| hIL-10var pDNA | Intra-articular | hIL-10var pDNA was safe, and significantly improved pain symptoms | – | [39] |
| Lutikizumab | Subcutaneous | Lutikizumab was generally well tolerated in patients with knee OA and elicited an anti-inflammatory response. | Phase I trial | [40-42] |
| Canakinumab | Intra-articular | The clinical trial was completed, but the results have not been released | Phase II trial | [43, 44] |
| Diacerein | Intra-articular | Diacerein has shown a reduction in synovitis in animal models of OA | – | [45] |
| Oral | Diacerein was noninferior to celecoxib in reducing pain, stiffness, or functional limitations | Phase III | [46] | |
| Adalimumab | Intra-articular | Adalimumab showed a significant improvement from baseline in VAS pain, WOMAC pain, stiffness, and function scores as well as physician assessments | – | [47, 48] |
| Corticosteroids | ||||
| FX006 (Zilretta) | Intra-articular | FX006 (Zilretta) markedly improved WOMAC scores for pain, stiffness, and physical function, and knee injury and KOOS-QOL scores compared with both placebo and TA crystal suspensions | Phase III | [49-51] |
| MTX | Oral | MTX remarkably reduced pain and improved synovitis in patients with symptomatic knee OA | – | [52] |
| The effect of oral MTX on pain and synovitis in patients with mid-to late-stage knee OA with effusion–synovitis is ongoing | Phase III | [53] | ||
| Vitamin D | Oral | Vitamin D showed significant effects on WOMAC total score, WOMAC function, VAS knee pain, and increase in BMLs, and might be beneficial for foot pain and depressive symptoms. | Phase III | [54-56] |
| Oral | Both supplementation of vitamin D and maintaining vitamin D sufficiency had dramatical effects on knee joint effusion–synovitis in knee OA patients | Phase III | [57, 58] | |
| Curcumin | Oral | Curcumin was more effective than placebo for knee pain but did not affect knee effusion–synovitis or cartilage composition | Phase II | [59] |
| The clinical trial is ongoing | Phase III | |||
- Abbreviations: BML, bone marrow lesion; DMM, destabilization of medial meniscus; IL, interleukin; KOOS-QOL, knee injury and osteoarthritis outcome score quality of life; MTX, methotrexate; Nab, neutralizing antibody; OA, osteoarthritis; TA, triamcinolone acetonide; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
3.1 Agents targeting cytokines
Inflammation is part of the OA process and inflammatory cytokines released by different articular cells are involved in pain and joint degradation.30, 60, 61 Several promising agents have shown disease-modifying effects on low-grade inflammation in animal models of OA that require confirmation in human clinical trials.62, 63 For example, intra-articular (IA) injection of an IL-17-neutralizing antibody in mice decreased cyclin-dependent kinase inhibitor 1A and MMP13 expression and increased expression of IL-4, thereby reducing joint degeneration and relieving pain.36 In addition to neutralizing antibodies, receptor blockers appeared to be effective in experimental OA studies. A study found that IA injection of mouse IL-36 receptor (IL-36R) antagonists attenuated OA development in mice, while human IL-36R antagonists reduced MMP13 in human OA chondrocytes.37 Tocilizumab, an IL-6R blocker, contributed to cartilage preservation and increased bone volume in a mouse model of ischemic osteonecrosis, and reduced cartilage damage and synovitis in a mouse model of medial meniscus destabilization-induced OA.38 An experimental study on a plasmid DNA containing a human IL-10 transgene variant (hIL-10var pDNA) was conducted to examine its effects on pain measures in companion (pet) dogs with naturally occurring OA.39 The results revealed that IA injection of hIL-10var pDNA led to significant improvements in pain measures in vivo without toxicological effects, suggesting that IL-10var pDNA was well tolerated as a therapeutic option. Therefore, therapies targeting cytokines may be useful in OA with inflammatory features. Nevertheless, well-designed randomized controlled trials are required to confirm the findings obtained in these experimental studies.
Lutikizumab, an anti-IL-1α/β dual variable domain immunoglobulin, provided limited improvement in knee pain and synovitis in a Phase II trial but reduced neutrophil levels and plateaued high-sensitivity C-reactive protein levels when applied as a 100-mg injection subcutaneously every 2 weeks for 50 weeks.40 Two Phase I clinical studies of lutikizumab demonstrated an anti-inflammatory response and good tolerance in healthy subjects and patients with mild-to-moderate knee OA (NCT01668511).41, 42 In patients with symptomatic, radiographic, and inflammatory knee OA, lutikizumab decreased WOMAC pain score at Week 16 (NCT02087904). Canakinumab, a humanized monoclonal antibody that blocks IL-1βR and is considered a disease-modifying antirheumatic drug (DMARD), showed symptom improvement for juvenile idiopathic arthritis and rheumatoid arthritis, with decreased cartilage destruction.43 A posthoc analysis in a randomized, double-blind, placebo-controlled trial (NCT01327846) was performed to determine the effects of canakinumab on incident hip and knee replacement. The results revealed significantly lower incidence rates for total hip or total knee replacement during a median follow-up of 3.7 years in participants receiving canakinumab compared with participants receiving placebo.44 The results supported further investigation of canakinumab for the treatment of large-joint OA. Another Phase II study (NCT01160822) on the safety, tolerability, pharmacokinetics, and pain effects of a single IA injection of canakinumab in patients with knee OA has been completed, but the results have not yet been released.
Diacerein is an inhibitor of IL-1β, and has an anticatabolic effect on OA tissues, and reduces MMP generation. In animal models of OA, diacerein has generally shown limited long-term effects on cartilage composition or pathology, but there is some evidence for a reduction in synovitis.45 Meanwhile, an international, multicenter, double-blind, randomized study reported that diacerein was noninferior to celecoxib in reducing pain, stiffness, and functional limitations.46 Adalimumab, a fully human anti-TNF-α monoclonal antibody, binds specifically to TNF-α and neutralizes its biological function by blocking the interactions with tumor necrosis factor receptor 1 (TNFR1) and TNFR2 receptors. An open-label randomized controlled trial concluded that there were significant improvements from baseline in visual analog scale (VAS) pain score, WOMAC pain, stiffness, and function scores and physician assessments after IA injection of adalimumab.47, 48 A Phase-2 clinical trial has evaluated the safety and efficacy of a single injection of XT-150 (formally hIL-10var pDNA) for the treatment of patients with knee OA (NCT04124042), and is estimated to be completed in 2022.
3.2 Corticosteroids
Corticosteroids are the most widely used anti-inflammatory agents worldwide, especially in the treatment of inflammatory diseases such as rheumatoid arthritis and gout. IA corticosteroids are commonly used for OA, with most trials focusing on knee OA, because they offer the opportunity to target inflammation at the joint level, thereby reducing systemic exposure to the drugs and the associated complications. However, corticosteroid injections have only short-term effects on knee pain and function, and treatments with sustained efficacy are needed.62 Furthermore, long-term (2 years) IA corticosteroid injections were reported to result in greater cartilage loss and no effects on pain compared with saline injection.49 FX006 (Zilretta), a novel type of extended-release triamcinolone acetonide (TA) formulation in 75:25 polymicrospheres, is designed to prolong conventional TA residence in the joint.50 FX006 significantly improved WOMAC scores for pain, stiffness, and physical function, as well as a knee injury and osteoarthritis outcome score quality of life scores for quality of life at 12 weeks, compared with both placebo and TA crystal suspensions.51 Owing to its reduced blood glucose elevation compared with standard TA crystal suspensions in patients with type 2 diabetes, FX006 was licensed by the Food and Drug Administration in October 2017 for the treatment of OA-related knee pain.
3.3 Methotrexate
Methotrexate (MTX) has an anti-inflammatory effect by curbing the inflammatory functions of neutrophils, macrophages, monocytes, dendritic cells, and lymphocytes through adenosine release, thereby suppressing the secretion of inflammatory cytokines such as TNF-α and IL-6.52 In an open-label study on moderate-dose oral MTX for symptomatic knee OA, a high proportion of participants had a significant reduction in pain, suggesting that MTX could be a therapeutic option for knee OA.52 However, a systematic review published in 2018 found that DMARDs, including MTX, showed poor efficacy.64 These results suggest that MTX may be particularly effective for OA patients with effusion–synovitis. A multicenter randomized controlled trial to investigate the effects of oral MTX on pain and synovitis in patients with mid-to-late-stage knee OA with effusion–synovitis (NCT03815448) is ongoing, and further data are expected soon.53 Overall, more evidence is needed to clearly define the role of MTX in OA treatment.
3.4 Vitamin D
Vitamin D supplementation did not prevent tibial cartilage loss or relieve WOMAC knee pain score over 2 years but had significant effects on WOMAC total score, WOMAC function score, VAS knee pain score, and BML increase, and may be beneficial for foot pain and depressive symptoms.54-56 Interestingly, both supplementation of vitamin D and maintenance of vitamin D sufficiency had significant effects on knee joint effusion–synovitis in patients with knee OA.57, 58
3.5 Curcumin
Curcumin is a natural phenol (diferuloylmethane) responsible for the yellow color of turmeric and is derived from the Curcuma longa root.65 Preclinical research showed that curcumin exhibited anti-inflammatory, antioxidant, and anticatabolic effects on chondrocytes by inhibiting expression of the inflammatory mediators IL-6, inducible nitric oxide synthase, and cyclooxygenase-2.65 Curcumin also blocked expression of MMPs and a disintegrin and metalloproteinase with thrombospondin motifs and increased expression of SOX-9 and production of collagen II, thus attenuating cartilage degradation.66, 67 We performed a randomized, double-blind, placebo-controlled trial to determine the efficacy of curcumin extract (CL) treatment for 3 months in reducing knee symptoms and effusion–synovitis in patients with symptomatic knee OA with effusion–synovitis.59 The results suggested that CL was more effective than placebo for knee pain but did not affect knee effusion–synovitis or cartilage composition. Thus, there is a need for multicenter and well-conducted randomized trials using larger samples to assess their efficacy.
4 CONCLUSION
OA is a complex, heterogeneous, and whole-joint disease with multiple etiologies.1, 68 As the nature of its pathophysiology has become clearer, it has become increasingly common to see OA described in phenotypes.69 OA phenotyping has the potential to make important and impactful contributions to the development of more effective and/or disease-modifying interventions for OA.13, 16, 70 Further knowledge of the heterogeneity of many aspects around OA can help to refine the design of future trials for potential disease-modifying osteoarthritis drugs (DMOADs), better delineate potential treatment targets, improve the ability to select appropriate patients for tested interventions, and adapt outcome measures to the situation.71 Thus, further work is needed to identify effective inhibitors of the low-grade inflammation in OA, and to determine whether therapies that target inflammation can prevent or slow the onset and progression of this disease with the inflammatory phenotype and eventually lead to transformative therapies.
5 PERSPECTIVES
The marked variations in disease expression and pathobiological manifestations in OA suggest the significant value of personalized and precision medicine from the therapeutic perspective.12, 69, 72 Personalized medicine is used to treat patients on the basis of their individual clinical characteristics, taking account of the diversity of symptoms, severity, and genetic defects.73 In precision medicine, molecular information maximizes the accuracy of patient classification and treatment, typically applying large amounts of data for the identification of patient phenotypes that share specific relevant characteristics to predict diagnosis, progression, or treatment response and utilize appropriate therapeutic targets.74, 75 Clinical phenotypes, endotypes, and molecular and imaging biomarkers are being identified, but their exact interactions and the underlying mechanisms remain to be elucidated.69, 76 While these biomarkers may have potential benefits in detecting patients at the greatest risk for structural progression, their use needs to be translated into efficient clinical trial designs and widespread clinical applications. Several recent clinical trials have utilized effusion–synovitis, an imaging biomarker, as a selection criterion and an endpoint to test the effects of anti-inflammatory agents on knee OA progression.53, 59 Such precise clinical trials will eventually help to develop true DMOADs that target the OA inflammatory phenotype.
ACKNOWLEDGMENT
No other people was involved in this paper.
CONFLICTS OF INTEREST
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
ETHICS STATEMENT
Ethics approvement was not required.
AUTHOR CONTRIBUTIONS
All authors contributed to the article and approved the submitted version.
Open Research
DATA AVAILABILITY STATEMENT
No data was used in this review paper.