Association of immunoglobulin G4-related disease with a family history of malignancy: A retrospective study of 168 cases
Diping Hu and Yanhong Li contributed equally to this study.
Abstract
Objective
Immunoglobulin G4-related disease (IgG4-RD) is a systemic immune-mediated fibroinflammatory condition. Previous studies have indicated relationships between malignancy and autoimmunity. This retrospective cohort study aimed to determine IgG4-RD incidence and clinical features in patients with a family history of malignancy.
Methods
To analyze the relationship between IgG4-RD and family history of malignancy, we reviewed IgG4-RD patients with a family history of malignancy diagnosed in various departments in West China Hospital, Sichuan University from December 2012 to September 2019. Clinical data and laboratory features were compared between IgG4-RD patients with and without a family history of malignancy.
Results
Among 168 enrolled patients with IgG4-RD, 22 (13.1%) had a family history of malignancy. The most frequently involved system in family members with malignancy was the digestive system (38.5%). Among patients with a family history of malignancy, the most frequently involved organs in IgG4-RD were the pancreas (31.9%) and lymph nodes (31.9%). Age at symptom onset was older in IgG4-RD patients with a family history of malignancy than in patients without a family history of malignancy (50–59 years: 36.3% vs. 16.4%, p = 0.0393). Hemoglobin (p = 0.0172) and albumin (p = 0.0247) levels were higher and globulin (p = 0.0232) levels were lower in patients with a family history of malignancy.
Conclusions
Our findings suggest that a family history of malignancy may be associated with IgG4-RD development. We hypothesize that genetic susceptibility may be involved in the pathogenesis of IgG4-RD.
Key points
-
Immunoglobulin G4-related disease (IgG4-RD) is a systemic immune-mediated fibroinflammatory condition. Previous studies have indicated relationships between malignancy and autoimmunity.
-
This retrospective cohort study found that a family history of malignancy was present in 13.1% of IgG4-RD patients.
-
Family history of malignancy may be associated with IgG4-RD development and genetic susceptibility may be involved in the pathogenesis of IgG4-RD, but further studies are needed to test this hypothesis and explore possible susceptibility genes.
1 INTRODUCTION
Immunoglobulin G4-related disease (IgG4-RD) is a systemic immune-mediated fibroinflammatory condition of unclear etiology that is characterized by elevated serum IgG4 concentrations and mass lesions in the pancreas, lymph nodes, lacrimal gland, parotid gland, lung, and other organs infiltrated by IgG4+ plasma cells.13 IgG4-RD tends to occur in men of middle and older age, and can affect nearly any organ.1-3 The condition did not appear in medical publications until 2003, and it tends to mimic malignancy.4 Moreover, owing to the relatively small number of confirmed cases, clinicians of various specialities have insufficient knowledge about the condition. Consequently, IgG4-RD is often misdiagnosed as cancer because it mimics tumors, and failure to recognize IgG4-RD at the early stage may lead to unnecessary surgical interventions and delayed treatment.5
Previous studies indicated that malignancy plays an important role for autoimmunity in rheumatic diseases and suggested an increased incidence of malignancy in IgG4-RD.6-11 For example, Wallace et al.12 indicated a possible association between history of cancer and subsequent development of IgG4-RD. It is interesting to note that, based on our observations, many family members of IgG4-RD patients have a history of cancer. However, no studies to date have identified a relationship between IgG4-RD and family history of malignancy.
This retrospective study aimed to analyze the relationship between IgG4-RD and family history of malignancy, by reviewing 168 IgG4-RD patients diagnosed in various departments in West China Hospital, Sichuan University from December 2012 to September 2019. The findings of the study may improve our understanding of IgG4-RD and the relationship between autoimmune disease and malignancy.
2 PATIENTS AND METHODS
2.1 Study population
The study was approved by the Ethics Committee of West China Hospital, Sichuan University, China. We searched the institutional database of West China Hospital, Sichuan University using the term “IgG4” for discharge diagnosis, and identified 168 cases with IgG4-RD appropriately diagnosed by doctors in various departments from December 2012 to September 2019. Most of the IgG4-RD cases were proven by biopsy.
2.2 Variables of interest
The electronically stored clinical notes for all patients before treatment were retrospectively reviewed, particularly with regard to organs involved in IgG4-RD, family history of malignancy, and serum IgG4 concentration. We reviewed the details, including age at symptom onset and disease diagnosis, sex, disease course, starting organ, involved organs, family history of malignancy, serum IgG4 concentration, serum immunoglobulin concentrations, serum complement C3 and C4 concentrations, hemoglobin concentration, platelet count, white blood cell count, neutrophil count, lymphocyte count, eosinophil count, serum albumin concentration, serum globulin concentration, and rheumatoid factor concentration.
2.3 Ethics approval
The study was approved by the Ethics Committee on Biomedical Research, West China Hospital, Sichuan University. All participants in the study provided written informed consent.
2.4 Statistical analysis
GraphPad Prism 8.0.2 software was used for all analyses. The statistical significance of differences in data was determined by Fisher's exact test for categorical data or by an unpaired t test or the Wilcoxon rank sum test for continuous data. A probability value of p < 0.05 was considered to indicate statistical significance.
3 RESULTS
3.1 Characteristics of the IgG4-RD cohort
Of the 168 enrolled patients, 116 (69%) were men and 52 (31%) were women (Table 1). The mean (SD) age at morbidity was 51.63 (14.9) years, and the mean (SD) disease course of IgG4-RD was 1.46 (2.57) years. In the total IgG4-RD cohort, the mean (SD) number of involved organs was 1.73 (1.17). The most commonly affected organs were the lymph nodes (57 cases; 33.9%), followed by the pancreas (43 cases; 25.6%), lacrimal gland (30 cases; 17.9%), submandibular gland (26 cases; 25.5%), bile duct (22 cases; 13.1%), kidney (20 cases; 11.9%), liver (19 cases; 11.3%), and parotid gland (17 cases; 10.1%).
| Demographic features | All (n = 168) | Without a family history of malignancy (n = 146) | With a family history of malignancy (n = 22) | P |
|---|---|---|---|---|
| Age at IgG4-RD onset (years, mean, SD) | 51.63 ± 14.9 | 51.19 ± 15.34 | 54.55 ± 11.4 | 0.3265 |
| 14–39 (N, %) | 37 (22.0%) | 36 (24.7%) | 1 (4.5%) | 0.0493* |
| 40–49 | 40 (23.8%) | 34 (23.3%) | 6 (27.3%) | 0.6026 |
| 50–59 | 32 (19.0%) | 24 (16.4%) | 8 (36.3%) | 0.0393* |
| 60–69 | 39 (23.2%) | 36 (24.7%) | 3 (13.6%) | 0.4155 |
| 70–79 | 17 (10%) | 13 (8.9%) | 4 (18.1%) | 0.2448 |
| 80–90 | 2 (1.0%) | 2 (1.4%) | 0 (0%) | >0.9999 |
| Time to diagnosis | 1.46 ± 2.57 | 1.49 ± 2.63 | 1.24 ± 2.11 | 0.6619 |
| Male | 116 (69.0%) | 100 (68.5%) | 16 (72.7%) | 0.8075 |
| Number of organs affected (mean, SD) | 1.73 ± 1.17 | 1.73 ± 1.14 | 1.73 ± 1.35 | 0.9963 |
| Single organ | 103 (61.3%) | 87 (59.6%) | 16 (72.7%) | 0.3478 |
| Multiorgan (≥2 organs) | 65 (38.7%) | 59 (40.4%) | 6 (27.3%) | 0.3478 |
| Organ involvement | ||||
| Lymph nodes | 57 (33.9%) | 50 (34.2%) | 7 (31.8%) | >0.9999 |
| Lacrimal gland | 30 (17.9%) | 26 (17.8%) | 4 (18.2%) | >0.9999 |
| Orbital | 10 (6.0%) | 9 (6.2%) | 1 (4.5%) | >0.9999 |
| Submandibular gland | 26 (25.5%) | 20 (13.7%) | 6 (27.3%) | 0.1159 |
| Parotid gland | 17 (10.1%) | 15 (10.3%) | 2 (9.1%) | >0.9999 |
| Sublingual gland | 5 (3.0%) | 3 (2.1%) | 2 (9.1%) | 0.1283 |
| Nasal cavity | 3 (1.8%) | 3 (2.1%) | 0 (0%) | >0.9999 |
| Lung | 15 (8.9%) | 13 (8.9%) | 2 (9.0%) | >0.9999 |
| Pleura | 2 (1.2%) | 1 (0.7%) | 1 (4.5%) | 0.2454 |
| Thoracic aorta | 3 (1.8%) | 3 (2.1%) | 0 (0%) | >0.9999 |
| Abdominal aorta | 1 (0.6%) | 0 (0%) | 1 (4.5%) | 0.1310 |
| Pancreas | 43 (25.6%) | 36 (24.7%) | 7 (31.8%) | 0.4456 |
| Liver | 19 (11.3%) | 18 (12.3%) | 1 (4.5%) | 0.4733 |
| Bile duct | 22 (13.1%) | 21 (14.4%) | 1 (4.5%) | 0.3139 |
| Retroperitoneum | 6 (3.6%) | 5 (3.4%) | 1 (4.5%) | 0.5751 |
| Renal | 20 (11.9%) | 19 (13.0%) | 1 (4.5%) | 0.4775 |
| Skin | 2 (1.2%) | 2 (1.4%) | 0 (0%) | >0.9999 |
| Forehead | 1 (0.6%) | 0 (0%) | 1 (4.5%) | 0.1310 |
| Meninx | 1 (0.6%) | 1 (0.7%) | 0 (0%) | >0.9999 |
- Abbreviation: IgG4-RD, immunoglobulin G4-related disease.
- * p < 0.05, significant difference between patients with and without family history of malignancy.
3.2 IgG4-RD patients with a family history of malignancy
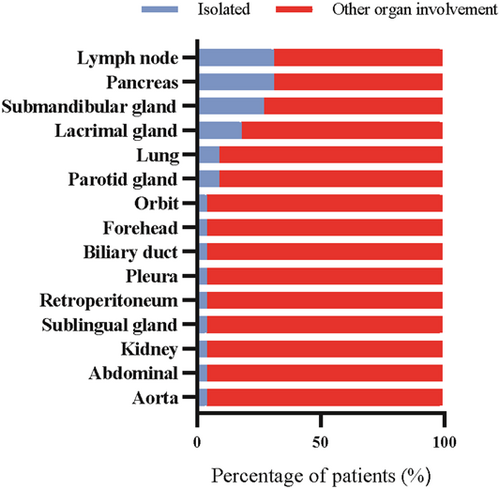
Among the 22 patients (13.1%) with a family history of malignancy, 16 (72.7%) were men and 6 (27.3%) were women (Table 2). In these 22 patients, the mean number of organs involved was 1.72 (range: 1–5), and the most commonly involved organs were the pancreas (31.9%), lymph nodes (31.9%), submandibular gland (27.3%), lacrimal gland (18.2%), parotid gland (9.1%), and lung (9.1%) (Figure 1). The pancreas was the most frequent starting organ (27.3%), followed by the lymph nodes (18.2%), submandibular gland (9.1%), lacrimal gland (9.1%), and lung (9.1%).
| Patient | Sex | Age at onset, years | Starting organ | Organs involvement | Family member with malignancy | Malignancy location |
|---|---|---|---|---|---|---|
| 1 | M | 61 | Kidney | Kidney, abdominal aorta | Father | Esophagus |
| 2 | M | 75 | Pancreas | Pancreas | Sister | Not detailed |
| 3 | F | 42 | Pleura | Pleura | Father | Liver |
| 4 | M | 55 | Submandibular gland | Submandibular gland | Parents | Lung-father Stomach-mother |
| 5 | F | 74 | Biliary duct | Biliary duct | Parents | Bladder-father Lung-mother |
| 6 | M | 52 | Pancreas | Pancreas | Father | Colon |
| 7 | M | 64 | Pancreas | Pancreas | Father | Brain |
| 8 | M | 50 | Lymph node | Lymph node, lacrimal gland, submandibular gland | Father | Liver |
| 9 | M | 50 | Lymph node | Lymph node | Uncle | Lymph node |
| 10 | M | 44 | Lymph node | Lymph node | Parents | Not detailed-father Not detailed-mother |
| 11 | M | 50 | Lung | Lung | Parents | Esophagus-father Stomach-mother |
| 12 | F | 40 | Forehead | Forehead, parotid gland, submandibular gland | Father | Larynx |
| 13 | M | 47 | Lacrimal gland | Lacrimal gland, parotid gland, submandibular gland, sublingual gland, lymph node | Father | Lung |
| 14 | F | 46 | Lymph node | Lymph node | Mother | Breast |
| 15 | M | 56 | Pancreas | Pancreas | Father | Liver |
| 16 | F | 56 | Orbit | Orbit, lymph node, submandibular gland | Father | Nasopharynx |
| 17 | F | 70 | Pancreas | Pancreas | Mother | Not detailed |
| 18 | M | 34 | Pancreas | Pancreas | Father | Liver |
| 19 | M | 65 | Submandibular gland | Submandibular gland, lacrimal gland, pancreas, lymph node | Father | Prostate |
| 20 | M | 52 | Lung | Lung | Father | Digestive tract |
| 21 | M | 46 | Lacrimal gland | Lacrimal gland | Father | Rectum |
| 22 | M | 71 | Retroperitoneum | Retroperitoneum | Father | Prostate |
- Abbreviations: F, female; IgG4-RD, immunoglobulin G4-related disease; M, male.
The 22 patients had 26 family members who had developed cancer, including a first-degree relative in 21 (95.5%) patients. The most commonly affected family member with malignancy was the father (63.6%), followed by both parents (18.2%), the mother (9.1%), a sister (4.5%), and an uncle (4.5%).
We also examined data for a natural population cohort in Sichuan Province and included 10,554 people as healthy controls. Among the healthy controls, 1179 (11.2%; 340 men, 839 women) had a family history of malignancy in 1259 family members. The proportion of 11.2% in the healthy controls was similar to the proportion of 13.1% in the IgG4-RD cohort. Interestingly, the healthy controls with a family history of malignancy were predominantly women (71.2%), while the IgG4 patients with a family history of malignancy were predominantly men (72.7%).
Regarding the location of the malignancy in the 26 family members of the 22 IgG4-RD patients, there were 10 cases (38.5%) of digestive system cancer (4 liver cancer, 2 esophageal cancer, 2 stomach cancer, 1 rectal cancer, and 1 colon cancer), 5 cases (19.2%) of respiratory system cancer (3 lung cancer, 1 nasopharyngeal cancer, and 1 laryngeal cancer), and 3 cases (11.5%) of urinary system cancer (2 prostate cancer and 1 bladder cancer). Other malignancies included brain cancer (one case; 3.6%), lymphoma (one case; 3.6%), and breast cancer (one case; 3.6%) (Table 3). Details were not available for five cases (Table 3). In the 1259 family members of the 1179 healthy controls, lung cancer (30.0%) was the most common, followed by esophageal cancer (10.6%), liver cancer (10.1%), and gastric cancer (8.9%) (Table 3).
| Cases (n = 168) | Controls (n = 10,554) | |||
|---|---|---|---|---|
| Number | (%) | Number | (%) | |
| Family history of malignancy | ||||
| No | 146 | 86.9 | 9375 | 88.8 |
| Yes | 22 | 13.1 | 1179 | 11.2 |
| Family members | 26 | 1259 | ||
| Type of malignancy | ||||
| Liver cancer | 4 | 15.4 | 127 | 10.1 |
| Lung cancer | 3 | 11.5 | 378 | 30.0 |
| Esophageal cancer | 2 | 7.6 | 133 | 10.6 |
| Stomach cancer | 2 | 7.6 | 112 | 8.9 |
| Prostate cancer | 2 | 7.6 | 36 | 2.9 |
| Rectal cancer | 1 | 3.8 | 89 | 7.1 |
| Colon cancer | 1 | 3.8 | 25 | 2.0 |
| Nasopharyngeal cancer | 1 | 3.8 | 21 | 1.7 |
| Laryngeal cancer | 1 | 3.8 | 18 | 1.4 |
| Bladder cancer | 1 | 3.8 | 14 | 1.1 |
| Brain cancer | 1 | 3.8 | 21 | 1.7 |
| Lymphoma | 1 | 3.8 | 25 | 2.0 |
| Breast cancer | 1 | 3.8 | 41 | 3.3 |
| Others | 5 | 19.2 | 219 | 17.4 |
- Abbreviation: IgG4-RD, immunoglobulin G4-related disease.
3.3 Clinical features of the IgG4-RD patients with and without a family history of malignancy
Among the 168 IgG4-RD patients, 22 (13.1%) had a family history of malignancy (Table 1). The median age of these patients was 54.55 years (range: 34–75 years). The patients with a family history of malignancy at symptom onset were older than the patients without a family history of malignancy (50–59 years: 36.3% vs. 16.4%, p = 0.0393; 14–39 years: 4.5% vs. 24.7%, p = 0.0493) (Table 2). Although there was no significant difference in the involved organs between the IgG4-RD patients with and without a family history of malignancy, it should be noted that patients with a family history of malignancy were more prone to the involvement of the submandibular gland than patients without a family history of malignancy (27.3% vs. 13.7%), but less prone to the involvement of the liver and bile duct (9.0% vs. 16.7%).
3.4 Serological features of the IgG4-RD patients with and without a family history of malignancy
The serological features of the IgG4-RD patients with and without a family history of malignancy are presented in Tables 4 and 5. There were no significant differences in the platelet, white blood cell, neutrophil, lymphocyte, and eosinophil counts between the patients with and without a family history of malignancy (Table 4). However, the hemoglobin level was significantly higher in patients with a family history of malignancy than in patients without a family history of malignancy (131.7 ± 19.35 vs. 119.7 ± 25.60 mg/L, p = 0.0172). Anemia defined as hemoglobin <120 mg/L was detected in 6 of the 22 patients (27.3%) with a family history of malignancy, compared with 66 of the 146 patients (45.2%) without a family history of malignancy.
| Laboratory index | All (n = 168) | Without a family history of malignancy (n = 146) | With a family history of malignancy (n = 22) | P |
|---|---|---|---|---|
| Hemoglobin (g/L) | 119.7 ± 25.60 | 119.7 ± 25.60 | 131.7 ± 19.35 | 0.0172* |
| ≥120 | 96 (57.1%) | 80 (54.8%) | 16 (72.7%) | 0.1648 |
| 90–120 | 48 (28.6%) | 43 (29.5%) | 5 (22.7%) | 0.6187 |
| 60–90 | 24 (14.3%) | 23 (15.8%) | 1 (4.5%) | 0.2068 |
| Platelet (×109/ml) | 224.1 ± 105.7 | 228.7 ± 107.6 | 193.1 ± 88.06 | 0.1414 |
| White blood cell (×109/ml) | 7.134 ± 3.139 | 7.211 ± 3.202 | 6.635 ± 2.690 | 0.4246 |
| Neutrophil (×109/ml) | 4.546 ± 2.856 | 4.580 ± 2.904 | 4.318 ± 2.564 | 0.6895 |
| Lymphocyte (×109/ml) | 1.677 ± 0.7681 | 1.684 ± 0.7550 | 1.629 ± 0.8682 | 0.7552 |
| Neutrophil/Lymphocyte | 3.994 ± 8.919 | 4.067 ± 9.482 | 3.512 ± 3.394 | 0.7866 |
| Eosinophil (×109/ml) | 0.315 ± 0.421 | 0.320 ± 0.433 | 0.283 ± 0.343 | 0.7012 |
| Albumin | 36.32 ± 7.450 | 35.82 ± 7.529 | 39.63 ± 6.067 | 0.0247* |
| Globulin | 41.82 ± 17.22 | 42.77 ± 17.710 | 33.74 ± 8.768 | 0.0232* |
| Albumin/Globulin | 1.032 ± 0.464 | 1.002 ± 0.463 | 1.231 ± 0.425 | 0.0306* |
| Complement C3 | ||||
| Not checked | 18 (10.7%) | 17 (11.6%) | 1 (4.5%) | 0.4730 |
| Normal | 80 (47.6%) | 72 (49.3%) | 8 (36.4%) | 0.3601 |
| <0.785 g/L | 70 (41.7%) | 57 (39.0%) | 13 (59.1%) | 0.1036 |
| Complement C4 | ||||
| Not checked | 17 (10.1%) | 16 (11.0%) | 1 (4.5%) | 0.7024 |
| Normal | 92 (54.8%) | 81 (55.5%) | 11 (50.0%) | 0.6526 |
| <0.145 g/L | 59 (35.1%) | 49 (33.6%) | 10 (45.5%) | 0.3389 |
| Rheumatoid factor | ||||
| Not checked | 28 (16.7%) | 25 (17.1%) | 3 (13.6%) | >0.9999 |
| Normal | 99 (58.9%) | 84 (57.5%) | 15 (68.2%) | 0.4862 |
| >20 IU/ml | 41 (24.4%) | 37 (25.3%) | 4 (18.2%) | 0.5991 |
- Abbreviation: IgG4-RD, immunoglobulin G4-related disease.
- * p < 0.05, significant difference between patients without and with a family history of malignancy.
| Immunoglobulin | All (n = 168) | Without a family history of malignancy (n = 146) | With a family history of malignancy (n = 22) | P |
|---|---|---|---|---|
| IgG4 concentration | 14.78 ± 22.46 | 14.96 ± 23.00 | 13.60 ± 18.98 | 0.9639 |
| Not checked | 9 (5.4%) | 8 (5.5%) | 1 (4.5%) | >0.9999 |
| Normal | 19 (11.3%) | 17 (11.6%) | 3 (13.6%) | 0.7293 |
| >Normal <2× ULN | 25 (14.9%) | 19 (13.0%) | 4 (2.7%) | 0.5093 |
| >2× Normal <5× ULN | 45 (26.8%) | 39 (26.7%) | 6 (27.2%) | >0.9999 |
| >5× ULN | 70 (41.7%) | 62 (42.5%) | 8 (36.3%) | 0.6488 |
| Immunoglobulin G | ||||
| Not checked | 16 (9.5%) | 14 (9.6%) | 2 (9.1%) | >0.9999 |
| Normal | 47 (28.0%) | 37 (25.3%) | 10 (45.5%) | 0.0723 |
| >15.5 mg/L | 105 (62.5%) | 95 (65.1%) | 10 (45.5%) | 0.0984 |
| Immunoglobulin A | ||||
| Not checked | 16 (9.5%) | 14 (9.6%) | 2 (9.1%) | >0.9999 |
| Normal | 113 (67.3%) | 96 (65.8%) | 17 (77.3%) | 0.3377 |
| >2900 mg/L | 39 (23.2%) | 36 (24.7%) | 3 (13.6%) | 0.4155 |
| Immunoglobulin M | ||||
| Not checked | 16 (9.5%) | 14 (9.6%) | 2 (9.1%) | >0.9999 |
| Normal | 118 (70.2%) | 105 (71.9%) | 13 (58.1%) | 0.2220 |
| >2200 mg/L | 34 (20.2%) | 27 (18.5%) | 7 (31.8%) | 0.1596 |
| Immunoglobulin E | ||||
| Not checked | 28 (16.7%) | 25 (17.1%) | 3 (13.6%) | >0.9999 |
| Normal | 45 (26.8%) | 40 (27.4%) | 5 (22.7%) | 0.7984 |
| >150 mg/L | 95 (56.5%) | 81 (55.5%) | 14 (63.6%) | 0.5000 |
- Abbreviations: IgG4-RD, immunoglobulin G4-related disease; ULN, upper limit of normal.
The mean serum levels of albumin (ALB) and globulin (GLB) in the 168 patients were 36.32 ± 7.450 and 41.82 ± 17.22 g/L, respectively (Table 4). The ALB level was significantly higher in patients with a family history of malignancy than in patients without a family history of malignancy (39.63 ± 6.067 vs. 35.82 ± 7.529 g/L, p = 0.0247), while the GLB level was significantly lower (33.74 ± 8.768 vs. 42.77 ± 17.710 g/L, p = 0.0232). Elevation of serum IgG levels, defined as IgG >15.5 mg/L, was seen in 105 of the 168 patients (62.5%) (Table 5). The frequency of elevated IgG levels in patients with a family history of malignancy was lower than that in patients without a family history of malignancy (45.5% vs. 65.1%, p = 0.0984). Elevation of serum IgG4 levels, defined as IgG4 ≥ 135 mg/dl, was detected in 140 of the 168 patients (83.3%) (Table 5). The median concentration of IgG4 in patients with a family history of malignancy was 453 mg/dl (range: 87.3–6880 mg/dl). However, there were no significant differences in the serum IgG4, IgA, IgE, IgM, rheumatoid factor, complement C3, or complement C4 levels between the patients with and without a family history of malignancy.
4 DISCUSSION
To our knowledge, this study is the first to report data on IgG4-RD patients with a family history of malignancy. We have described the clinical and laboratory features of 168 IgG4-RD patients, of whom 22 (13.1%) had a family history of malignancy. For the patients with a family history of malignancy, the most frequently involved organs in the IgG4-RD patients were the pancreas and lymph nodes, while the digestive system was most frequently affected by cancer in their family members. Compared with patients without a family history of malignancy, patients with a family history of malignancy were older at symptom onset and had higher hemoglobin and ALB levels and lower GLB levels.
Recent studies have shown that cancer and autoimmune disorders can affect one another.13 On the one hand, malignancy can be accompanied by certain autoimmune disorders, while on the other hand, certain autoimmune disorders and immunosuppressive therapy can increase the risk of malignancy.13 These findings may be partly explained by genetic risk factors, immune surveillance, and environmental factors.13 Data from the Swedish Multigeneration Register and the Swedish Cancer Register revealed that family history of autoimmune disease in siblings was associated with a higher incidence of gastric corpus cancer, with a standardized incidence ratio of 1.36 (95% confidence interval: 1.22–1.52), suggesting that genetic polymorphisms may play a role and provide novel mechanisms in cancer and autoimmune diseases.14 A smaller study on 279 childhood acute leukemia patients and 285 controls15 revealed similar findings that history of autoimmune disease in first-degree or second-degree relatives was significantly associated with acute lymphocytic leukemia (odds ratio: 1.7; 95% confidence interval: 1.0–2.8). According to a previous study, K-ras mutations occur most frequently in the pancreatobiliary region in patients with autoimmune pancreatitis, and autoimmune pancreatitis may be a risk factor for pancreatobiliary cancer.16 In the present study, the incidence of a family history of malignancy among IgG4-RD patients was 13.1%. The malignancy in the family members of the IgG4-RD patients most often involved the digestive system (45.5%), with liver cancer (18.2%) being the most common. Furthermore, the most commonly affected family member with malignancy was the father. We hypothesize that family history of malignancy may be associated with increased incidence of IgG4-RD and that genetic susceptibility may be involved in the pathogenesis of IgG4-RD. Future prospective studies are needed to clarify underlying mechanisms for these results.
The most commonly involved organs in IgG4-RD patients are the pancreas, kidney, orbital adnexal structures, salivary gland, and retroperitoneum.3 Similarly, we found that the most frequently involved organs in IgG4-RD patients with a family history of malignancy were the pancreas and lymph nodes. We further found that patients with a family history of malignancy were older at symptom onset than patients without a family history of malignancy. In the study, the age at symptom onset in patients with a family history of malignancy was higher for the range of 50–59 years and lower for the range of 14–39 years compared with patients without a family history of malignancy. According to previous research, IgG4-RD mostly occurs in the sixth decade of life.3 Interestingly, Wallace et al.12 found that patients with a history of malignancy were significantly older than patients without a history of malignancy. In another study, patients with IgG4-RD onset at ≥65 years of age tended to have a greater frequency of a history of malignancy than IgG4-RD patients with onset at <65 years of age.17 Consequently, older patients with cancer should have attention paid to the possibility of their disease being accompanied by IgG4-RD when their symptoms cannot be explained by cancer alone, especially in patients with a family history of malignancy.
Elevated serum IgG4 levels are useful for screening but nonspecific for diagnosis.2, 3 Nevertheless, high IgG4 levels appear to be associated with multiorgan involvement,3 and there is a relationship between serum IgG4 concentration and disease activity in some patients.2 In the present study, serum IgG4 level was elevated in 83.3% of patients with a family history of malignancy, with a median concentration of 453 mg/dl. However, there was no significant difference in serum IgG4 concentration between patients with and without a family history of malignancy. Interestingly, previous studies also found that the differences in serum IgG4 concentration between patients with and without a history of malignancy were not significant.9, 12 Elevated immunoglobulin G (IgG), IgE, erythrocyte sedimentation rate, C-reactive protein, and peripheral blood eosinophilia were observed in IgG4-RD patients but were nonspecific findings,3 and few studies have shown that hemoglobin, ALB, and GLB have significance for this disease. In the present study, however, we found that hemoglobin and ALB levels were higher in patients with a family history of malignancy than in patients without a family history of malignancy, while the GLB level was lower. The latter may result from the finding that IgG4-RD patients with a family history of malignancy had less involvement of the liver than IgG4-RD patients without a family history of malignancy (4.5% vs. 12.3%) because ALB is predominantly synthesized in the liver.18 More studies are needed to explain these findings.
The present study has several strengths. First, the cases in this study were relatively well diagnosed, and biopsies of the patients with masses revealed IgG4-positive infiltrating cells that met the diagnostic criteria. Second, at the time of evaluation, the patients in our study were not receiving regular treatment. Third, the study included patients diagnosed in various departments and not in a single department, such as the Rheumatology and Immunology Department or Gastroenterology Department. Fourth, this is the first study to analyze the association between IgG4-RD and family history of malignancy.
The study also has some limitations. Most of the patients in the study were from the southwest region of China, which may limit the generalizability of the findings. Owing to the retrospective design, some elements of the data set may have been affected by recall bias. Because of the limited number of patients, we were unable to detect potential differences in other clinical and laboratory features of IgG4-RD between patients with and without a family history of malignancy.
In conclusion, we evaluated the incidence of a family history of malignancy in IgG4-RD patients and described clinical and laboratory features of these patients as well as the clinical characteristics of their family members with malignancy. The pancreas and lymph nodes were the most frequently involved organs in IgG4-RD patients with a family history of malignancy. For IgG4-RD patients with a family history of malignancy, the digestive system was the most frequently affected system by cancer in their family members with malignancy. Compared with patients without a family history of malignancy, patients with a family history of malignancy were older at symptom onset and had higher hemoglobin and ALB levels and lower GLB levels. The findings of the present study may support contemporary hypotheses about the relationships between malignancy and subsequent development of autoimmune conditions. We hypothesize that genetic susceptibility may be involved in the pathogenesis of IgG4-RD. Further studies are needed to test this hypothesis and explore possible susceptibility genes.
ACKNOWLEDGMENTS
The authors thank Ling Ma for generously checking the literature. The authors also thank the Natural Population Cohort Study of West China Hospital of Sichuan University participants and the staff members for their contribution to data collection and for making the data available to us. This study was supported by the National Key Research and Development Program of China (2019YFE0108200), the National Natural Science Foundation of China (81771742, 81770101, 81403041, 82001728), 1·3·5 project for Outstanding interdisciplinary project of West China Hospital, Sichuan University (ZYGD18015, 312 ZYJC18003, ZYJC18024), China Postdoctoral Science Foundation (2019M663522), Sichuan Science and Technology Program (20YYJC3358), and Sichuan University postdoctoral interdisciplinary Innovation Fund.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ETHICS STATEMENT
The studies involving human participants were reviewed and approved by Ethics Committee on Biomedical Research, West China Hospital of Sichuan University. The patients/participants provided their written informed consent to participate in this study.
AUTHOR CONTRIBUTION
Hu DP, Li YH, Zhao Y and Liu Y contributed to study conception and design. Hu DP, Li YH, Zhou Y, Luo YB, Cheng L, Tan CY, Zhang QP, Zhao Y and Liu Y especially contributed to acquiring data. Hu DP, Li YH, Zhou Y, Luo YB, Cheng L, Tan CY, Zhang QP, Zhao Y and Liu Y contributed to analyzing data. Hu DP, Li YH, Zhou Y, Luo YB, Cheng L, Tan CY, Zhang QP, Zhao Y and Liu Y contributed to interpreting data. Hu DP, Li YH, Zhou Y, Luo YB, Cheng L, Tan CY, Zhang QP, Zhao Y and Liu Y contributed to enhancing the intellectual content. All authors contributed to the article and approved the submitted version.
Open Research
DATA AVAILABILITY STATEMENT
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.