Clinical, economic, and health-related quality of life outcomes in patients with overweight or obesity in the United States: 2016–2018
Abstract
Objectives
This study aimed to estimate clinical, economic (including productivity), and health-related quality of life (HRQoL) outcomes and associated individual characteristics among adults with overweight (OW) or obesity in the United States.
Methods
This study included adult respondents with body mass index (BMI) ≥18.5 kg/m2 in the 2017–2018 National Health and Nutrition Examination Survey (NHANES) and 2016 Medical Expenditure Panel Survey. Respondents were classified according to BMI. Individual characteristics were described by BMI categories. Multivariable regression models estimated the association between BMI categories and outcomes, adjusting for individual characteristics.
Results
Nearly three-quarters (73.7%) of NHANES participants were OW or obese. Relative to Normal weight (NW), respondents with Class 3 obesity had more obesity-related complications (2.07 vs. 4.62, p < 0.001). Higher BMI was associated with significantly lower HRQoL, lower productivity, and higher healthcare expenditures as well as more frequent weight loss attempts in the previous 12 months. Weight loss surgery and prescription anti-obesity medications (AOMs) were used only by a very small proportion of individuals. Despite frequent weight loss attempts, most respondents did not achieve clinically meaningful weight loss.
Conclusions
Adults with OW or obesity experienced worse clinical, economic and HRQoL outcomes than those with NW. Better use of evidence-based obesity treatments, including prescription AOMs, should be considered to achieve more clinically meaningful weight reduction and improved outcomes in individuals with OW or obesity.
Graphical Abstract
Using current US national survey data, we find that increasing overweight (OW) and obesity are significantly associated with increasing burdens in obesity-related comorbidities, health-related quality of life (HRQoL), mobility, productivity, and disability. Weight loss attempts increase with OW and obesity but do not result in clinically meaningful weight loss, while very few survey respondents reported prescription anti-obesity medication (AOMs) use in the previous 12 months. Better use of existing evidence-based obesity treatments may achieve more clinically meaningful weight reduction and improve health and economic outcomes in individuals with OW and obesity.
1 INTRODUCTION
Obesity is one of the biggest drivers of other preventable chronic diseases,1 mortality,2, 3 and healthcare costs and utilization in the United States.4 In 2019, the estimated annual economic cost of obesity in the US was $706 billion.4 Direct medical costs accounted for $304 billion of the annual economic burden, and indirect costs such as lost productivity and disability costs accounted for more than half ($401 billion) of the annual economic burden. Obesity also has a significant psychosocial burden and impact on individuals' health-related quality of life (HRQoL).5-7 Over the past several decades, an increased understanding of the underlying biological basis of obesity and the obesity-related comorbidities (ORCs), for example, Type 2 diabetes, hypertension, cardiovascular disease (CVD), osteoarthritis, and cancer, has prompted innovation in obesity treatment, including the development of several new safe and efficacious anti-obesity medications (AOMs).8
Lifestyle modification has long remained the cornerstone of obesity treatment, with intensive interventions potentially yielding a 5%–10% weight reduction. This degree of weight reduction has been shown to reduce cardiovascular risk factors, prevent or delay the development of Type 2 diabetes, and improve overall well-being.5, 6, 9, 10 However, lifestyle modification typically focuses on caloric restriction, and such approaches have been shown to elicit metabolic adaptive responses that lead to weight regain over time. Current guidelines have thus evolved to recommend both lifestyle modification and medications for initial weight reduction and long-term weight maintenance.11, 12 Metabolic and bariatric surgery is now recommended for consideration for individuals starting with a body mass index (BMI) of 30 who do not achieve substantial or durable weight loss or obesity disease-related improvement using nonsurgical methods.13 Despite these recommendations, utilization of prescription AOMs remains very low—estimates suggest that only 0.1%–1.3% of the eligible population use prescription AOMs.14-17
Current literature describes characteristics of persons in the US with overweight (OW) or obesity (BMI ≥25 kg/m2).18-23 However, there is a lack of current, nationally representative estimates of health outcomes, and clinical and behavioral characteristics such as the utilization of weight-related interventions (e.g., diet, exercise, surgery, AOMs). A current assessment of the health and economic outcomes in persons with OW or obesity is necessary to understand the scale of unmet needs and to inform obesity-related health policy. In this study, nationally representative data were used to investigate clinical, economic (including productivity), and HRQoL outcomes and their association with individual characteristics among adults with OW or obesity in the U.S. In addition, weight loss history within this population was investigated.
2 MATERIALS AND METHODS
2.1 Data sources
This study utilized the 2017–2018 National Health and Nutrition Examination Survey (NHANES) and 2016 Medical Expenditure Panel Survey (MEPS) data. NHANES is a continuous biennial survey that collects demographic, socioeconomic, dietary, and health-related data through interviews and physical examinations from approximately 9000 persons each year.24 MEPS is an annual survey designed to understand the cost and utilization of healthcare among families and individuals across the US. A new panel of approximately 15,000 households is selected from those participating in the National Health Interview Survey each year. The 2016 MEPS data were also used in this study, the most recent year with BMI data available.
2.2 Study samples
Two separate study cohorts were assembled with respondents from the 2017–2018 NHANES and 2016 MEPS databases. Those aged ≥18 years with a BMI ≥18.5 kg/m2 were included. Respondents were classified according to BMI—calculated using current body weight and height for all outcomes. Normal weight (NW) was defined as BMI 18.5–24.9 kg/m2, OW as BMI 25–29.9 kg/m2, class 1 (C1) obesity as BMI 30–34.9 kg/m2, class 2 (C2) obesity as BMI 35–39.9 kg/m2, or class 3 (C3) obesity as BMI ≥40 kg/m2. Respondents with incomplete information on weight, height, or age were excluded. Women who reported being pregnant at the time of the survey were also excluded.
2.3 Measures
2.3.1 National Health and Nutrition Examination Survey
Within the NHANES cohort, demographic, and socioeconomic characteristics (sex, age, race/ethnicity, education, health insurance) and clinical characteristics (BMI, weight history, ORCs, weight management methods utilized, clinically meaningful weight reduction) were summarized and compared across BMI categories (NW, OW, and C1, C2, C3 obesity). Clinically meaningful weight reduction was defined as a loss of ≥ 5% of body weight over the previous 12 months. To describe a clinically meaningful weight reduction by BMI category, the respondent's BMI category prior to their subsequent weight loss was used. This was calculated using the individual's self-reported body weight from the previous year and their current measured height. Weight management methods reported by NHANES respondents were grouped into the following categories: commercial, general dietary guidelines, evidence-based, and unhealthy methods (see Table 1 for each group's respective weight management methods). The full list of NHANES’ obesity-related comorbidities and their definitions are provided in Supplemental Table S1. The comorbidities were identified through self-reported medical histories, clinical lab testing, or inferred via self-reported prescription drug use.
| Normal (N = 1373, 26.3%) | OW (N = 1708, 31.3%) | C1 obesity (N = 1144, 22.3%) | C2 obesity (n = 580, 11.1%) | C3 obesity (N = 474, 8.9%) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, mean [median] | 43.8 | [41] | 49.6 | [50] | 49.5 | [52] | 48.4 | [52] | 45.5 | [45] | <0.001 |
| Female, n % | 734 | 53.5% | 778 | 45.6% | 557 | 48.7% | 326 | 56.2% | 304 | 64.1% | <0.001 |
| Married, n % | 699 | 50.9% | 1062 | 62.2% | 643 | 56.2% | 323 | 55.7% | 251 | 53.0% | 0.039 |
| Smoker, n % | 274 | 20.0% | 272 | 15.9% | 186 | 16.3% | 93 | 16.0% | 87 | 18.4% | <0.001 |
| Race/ethnicity, n % | |||||||||||
| White | 470 | 34.2% | 547 | 32.0% | 411 | 35.9% | 209 | 36.0% | 173 | 36.5% | 0.243 |
| Black | 280 | 20.4% | 328 | 19.2% | 276 | 24.1% | 174 | 30.0% | 161 | 34.0% | 0.008 |
| Mexican American | 113 | 8.2% | 264 | 15.5% | 184 | 16.1% | 99 | 17.1% | 63 | 13.3% | 0.008 |
| Other hispanic | 94 | 6.8% | 205 | 12.0% | 117 | 10.2% | 50 | 8.6% | 28 | 5.9% | 0.004 |
| Other | 416 | 30.3% | 364 | 21.3% | 156 | 13.6% | 48 | 8.3% | 49 | 10.3% | 0.008 |
| Education, n % | |||||||||||
| Less than high school degree | 229 | 16.7% | 360 | 21.1% | 238 | 20.8% | 98 | 16.9% | 68 | 14.3% | 0.797 |
| High school diploma without bachelor's degree | 645 | 47.0% | 849 | 49.7% | 654 | 57.2% | 355 | 61.2% | 314 | 66.2% | 0.006 |
| Bachelor's degree and above | 380 | 27.7% | 436 | 25.5% | 223 | 19.5% | 100 | 17.2% | 78 | 16.5% | 0.018 |
| Health insurance, n % | |||||||||||
| Private health insurance | 676 | 49.2% | 853 | 49.9% | 570 | 49.8% | 271 | 46.7% | 223 | 47.0% | 0.668 |
| Medicare | 330 | 24.0% | 479 | 28.0% | 338 | 29.5% | 158 | 27.2% | 100 | 21.1% | 0.027 |
| Medicaid | 237 | 17.3% | 264 | 15.5% | 194 | 17.0% | 106 | 18.3% | 102 | 21.5% | 0.189 |
| Other health insurance | 250 | 18.2% | 348 | 20.4% | 250 | 21.9% | 122 | 21.0% | 100 | 21.1% | 0.792 |
| No health insurance | 207 | 15.1% | 252 | 14.8% | 167 | 14.6% | 90 | 15.5% | 76 | 16.0% | 0.412 |
| Obesity-related comorbidities, n % | |||||||||||
| Metabolic | |||||||||||
| Dyslipidemia | 402 | 29.3% | 742 | 43.4% | 496 | 43.4% | 268 | 46.2% | 195 | 41.1% | 0.003 |
| Hypertension | 649 | 47.3% | 1065 | 62.4% | 805 | 70.4% | 427 | 73.6% | 373 | 78.7% | <0.001 |
| Metabolic syndrome | 352 | 25.6% | 738 | 43.2% | 575 | 50.3% | 315 | 54.3% | 262 | 55.3% | <0.001 |
| Pre-diabetes | 465 | 33.9% | 725 | 42.4% | 518 | 45.3% | 264 | 45.5% | 227 | 47.9% | <0.001 |
| NAFLD | 147 | 10.7% | 383 | 22.4% | 331 | 28.9% | 199 | 34.3% | 174 | 36.7% | <0.001 |
| Type 2 diabetes | 144 | 10.5% | 331 | 19.4% | 289 | 25.3% | 188 | 32.4% | 166 | 35.0% | <0.001 |
| Inflammatory | |||||||||||
| Asthma | 178 | 13.0% | 207 | 12.1% | 182 | 15.9% | 98 | 16.9% | 133 | 28.1% | 0.006 |
| Gout | 175 | 12.7% | 368 | 21.5% | 321 | 28.1% | 222 | 38.3% | 211 | 44.5% | <0.001 |
| Cardiorenal | |||||||||||
| CVD | 256 | 18.6% | 408 | 23.9% | 328 | 28.7% | 167 | 28.8% | 146 | 30.8% | 0.005 |
| Heart failure | 22 | 1.6% | 41 | 2.4% | 50 | 4.4% | 30 | 5.2% | 35 | 7.4% | 0.01 |
| CKD/ESRD | 194 | 14.1% | 267 | 15.6% | 230 | 20.1% | 128 | 22.1% | 94 | 19.8% | <0.001 |
| Neoplastic | |||||||||||
| Cancer | 68 | 5.0% | 117 | 6.9% | 67 | 5.9% | 35 | 6.0% | 22 | 4.6% | 0.300 |
| Mechano-physical | |||||||||||
| Sleep apnea | 193 | 14.1% | 349 | 20.4% | 292 | 25.5% | 175 | 30.2% | 189 | 39.9% | <0.001 |
| Osteoarthritis | 119 | 8.0% | 191 | 11.2% | 155 | 13.5% | 89 | 15.3% | 88 | 18.6% | 0.021 |
| Reproductive | |||||||||||
| Female infertility | 43 | 3.1% | 40 | 2.3% | 37 | 3.2% | 20 | 3.4% | 32 | 6.8% | 0.138 |
| Erectile dysfunction | 3 | 0.2% | 2 | 0.2% | 2 | 0.2% | 2 | 0.3% | 1 | 0.2% | 0.846 |
| Psychological | |||||||||||
| Depression | 124 | 9.0% | 194 | 11.4% | 196 | 17.1% | 104 | 17.9% | 104 | 21.9% | 0.051 |
| Anxiety | 34 | 2.5% | 64 | 3.7% | 65 | 5.7% | 33 | 5.7% | 32 | 6.8% | 0.712 |
| Total number of obesity-related comorbidities, mean [median] | 2.07 | [2] | 3.04 | [3] | 3.58 | [4] | 4.12 | [4] | 4.62 | [4] | <0.001 |
| Weight history | |||||||||||
| Current BMI (kg/m2), mean [median] | 22.31 | [23.06] | 27.41 | [27.81] | 32.29 | [31.97] | 37.07 | [36.37] | 45.84 | [43.47] | <0.001 |
| Change in weight (lbs.) in last 12 monthsa mean [median] | 10.29 | [6.68] | 7.66 | [3.95] | 7.18 | [3.57] | 5.89 | [4.15] | 4.20 | [3.15] | <0.001 |
| Lost ≥5% of weight in last 12 monthsa, n % | 11 | 0.8% | 50 | 2.9% | 49 | 4.3% | 28 | 4.8% | 19 | 4.0% | 0.005 |
| Weight loss methods | |||||||||||
| Tried to lose weight in last 12 months, n % | 220 | 16.0% | 602 | 35.2% | 498 | 43.5% | 272 | 46.9% | 272 | 57.4% | <0.001 |
| Total # of weight loss methods mean [median] | 1.27 | [0] | 2.86 | [1] | 3.43 | [3] | 3.74 | [4] | 4.23 | [5] | <0.001 |
| # of commercial weight loss methods mean [median] | 0.03 | [0] | 0.12 | [0] | 0.13 | [0] | 0.19 | [0] | 0.23 | [0] | <0.001 |
| # of dietary guideline weight loss methods mean [median] | 0.49 | [0] | 1.08 | [0] | 1.19 | [1] | 1.35 | [1] | 1.61 | [2] | <0.001 |
| # of evidence-based loss methods mean [median] | 0.33 | [0] | 0.77 | [0] | 0.90 | [1] | 0.90 | [1] | 1.05 | [1] | <0.001 |
| # of unhealthy weight loss methods mean [median] | 0.04 | [0] | 0.08 | [0] | 0.17 | [0] | 0.17 | [0] | 0.17 | [0] | <0.001 |
| Weight loss surgery (any time), n % | 4 | 0.3% | 10 | 0.6% | 17 | 1.5% | 23 | 4.0% | 18 | 3.8% | 0.034 |
| Prescription AOM (last 12 months), n % | 2 | 0.1% | 18 | 1.1% | 21 | 1.8% | 15 | 2.6% | 31 | 6.5% | 0.010 |
- Note: Dietary guideline weight loss methods: ate less fat to lose weight, ate more fruits, vegetables, salads, ate less sugar, candy, sweets, ate less junk or fast food, and drank a lot of water; Commercial weight loss methods: ate diet foods or products, used a liquid diet formula, took non-rx supplement, and joined a weight loss program; Evidence based weight loss methods: having weight loss surgery (ever), prescription diet pills, ate less (to lose weight), switched to low caloric foods, and exercised (to lose weight); Unhealthy weight loss methods: skipped meals, took laxatives/vomited, and started smoking (to lose weight).
- Abbreviations: AOM, anti-obesity medication; CKD, chronic kidney disease; CVD, cardiovascular disease; ESRD, end-stage renal disease; HF, heart failure; NAFLD, non-alcoholic fatty liver disease; Rx, prescription. See supplemental table for definition of comorbidities.
- a These variables are stratified and grouped using previous year's BMI to assign them to Normal, OW, C1 obesity, C2 obesity, and C3 obesity.
2.3.2 Medical Expenditure Panel Survey
Within the MEPS cohort, measures of productivity, healthcare expenditures, and quality of life were summarized and compared across BMI categories. Productivity was represented by self-reported inability to work, limited ability to work (regardless of employment status), and missing days of work due to illness or injury. Inability to work was defined as an impairment that incapacitates an individual, preventing them from gainful employment. Limited ability to work was defined as an individual's inability to complete a role in a similar manner before their impairment. Health-related quality of life was measured by the SF-12 mental (mental functioning (MCS)) and physical component summary (PCS) scores. SF-12 scores are norm-based to the US population average (50 ± 10), with higher scores indicating better health status. Additionally, within MEPS, BMI is calculated using self-reported height and weight. As self-reported data are at increased risk of bias, resulting in either under or overestimations, a previously reported adjustment method to more accurately predict BMI was used.25, 26
2.4 Data analyses
All analyses were conducted separately for each study cohort (i.e., data for NHANES and MEPS cohorts were not combined). This study summarized measures by current BMI category using descriptive statistics, with the exception of weight management methods and clinically meaningful weight reduction, which were summarized by the previous year's BMI category for the NAHNES cohort. For continuous variables, both means and medians are reported. Statistical significance across BMI categories was evaluated using analysis of variance tests for the differences in the means of the continuous variables and assessed by chi-squared tests for categorical variables. In addition, multivariable regression was conducted to estimate the association between BMI categories and (1) total number of obesity-related comorbidities, (2) number of weight management methods used, and (3) clinically meaningful weight reduction over the preceding 12 months in the NHANES cohort, as well as (1) SF-12 MCS and SF-12 PCS scores, (2) limited ability to work, and (3) inability to work in the MEPS cohort. Negative binomial regression was used to model the number of obesity-related comorbidities in the NHANES cohort. A generalized linear model with a log link was used to model SF-12 PCS and MCS scores in the MEPS cohort. Logistic regression was used to model the probability of inability to work and limited ability to work in the MEPS cohort, as well as achieving clinically meaningful weight reduction in the NHANES cohort.
All the models included age, race/ethnicity, sex, education, and type of health insurance (private health insurance, Medicaid, Medicare, other health insurance, none) as covariates. Education was (1) less than high school level, (2) less than bachelor's level (high school degree, some college—no degree, or an associate degree), and (3) bachelor's level and higher. As smoking is reported as a weight management method, there will be a direct relationship between the number of weight management methods and being a smoker. Only NHANES included the variable for smoking status; this was controlled for in models using this data source, but not controlled in the analysis of weight management methods.27
Unless indicated otherwise, analyses of NHANES and MEPS data were conducted using the survey weights and primary sampling units/strata for the respective survey to account for the complex survey designs. Survey weights determined how much each respondent would count in a statistical procedure, ensuring that the percentages of count variables and the means and medians of continuous variables presented in this study represent national estimates. Effect differences between groups were assessed using two-sided chi-squared and two-sided t-tests, with a threshold of 0.05 to assess statistical significance in all analyses. All analyses were conducted using Stata-MP 16.0.28
3 NATIONAL HEALTH AND NUTRITION EXAMINATION SURVEY COHORT RESULTS
3.1 BMI and patient characteristics
Patient characteristics by BMI category for the NHANES cohort are displayed in Table 1. In the NHANES 2017–2018 survey, there were 5279 respondents who met the study inclusion criteria. Nearly three-quarters of NHANES participants had OW or obesity (3905, 73.7%), including over 4 in 10 with obesity (42.3%). Specifically, 31.3% (1708; 95% CI: 28.6%–33.9%) had OW, 22.3% (1144; 95% CI: 20.0%–24.7%) had C1 obesity, 11.1% (580; 95% CI: 9.8%–12.3%) had C2 obesity, and 8.9% (474; 95% CI: 7.0%–10.8%) had C3 obesity. The remaining were NW (1373; 26.3% [95% CI: 23.4%–29.1%]). The majority of individuals with NW, C2, and C3 obesity were female ([NW: 734; 53.5%] [C2: 326; 56.2%] [C3: 304; 64.1%]), while a majority of those with OW and C1 obesity were male ([OW: 930; 54.3%] [C1: 587; 51.3%]). Individuals with NW and C3 obesity were the youngest, with a median age of 41 (95% CI: 37.5–44.4) and 45 (95% CI: 41.6–48.43), respectively. Individuals with OW, C1, and C2 obesity were significantly older with median ages at 50 (95% CI: 47.1–52.9), 52 (95% CI: 49.1–54.9), and 52 (95% CI: 49.1–54.9) respectively. As BMI increased, Black respondents accounted for increasingly higher proportions of each category (OW: 328, 19.2%; C1: 276, 24.1%; C2: 174, 30.0%; C3: 161, 34.0%).
Educational attainment varied significantly across BMI categories. The proportion of respondents categorized as having a high school diploma without a bachelor's degree increased as BMI increased (NW: 645 (47.0%); OW: 849 (49.7%); C1: 654 (57.2%); C2: 355 (61.2%); C3: 314 (66.2%)–p = 0.006). The proportion of respondents categorized with a bachelor's degree or higher decreased as BMI increased (NW: 380 (27.7%); OW: 436 (25.5%); C1: 223 (19.5%); C2: 100 (17.2%); C3: 78 (16.5%), p = 0.018). Medicare coverage differed significantly across BMI categories, with trends appropriate to the age distribution.
3.2 Obesity-related comorbidities
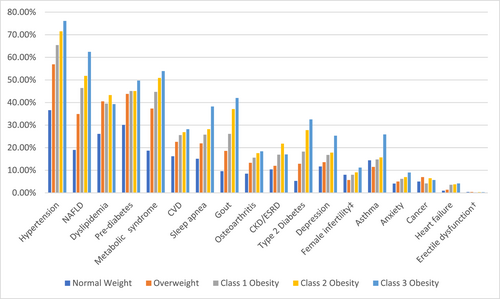
Most cardiometabolic, inflammatory and mechanophysical complications of obesity were positively associated with the BMI category (Table 1 and Figure 1). Particularly, the presence of hypertension, metabolic syndrome, pre-diabetes, non-alcoholic fatty liver disease (NAFLD), Type 2 diabetes, gout, CVD, heart failure (HF), sleep apnea, and osteoarthritis (p < 0.05 for all of these categories) were all positively associated with BMI category. Compared to NW, obesity-related complications in respondents with C3 obesity were over 40% higher for pre-diabetes (33.9% vs. 47.9%), nearly doubled for CVD, OSA, and osteoarthritis (18.6% vs. 30.80%, 14.1% vs. 39.9%, and 8.0% vs. 16.6% respectively), and approximately tripled for NAFLD (10.7% vs. 36.7%). Rates of hypertension and metabolic syndrome were over 50% and 100% higher (47.3% vs. 78.7%, and 25.6% vs. 55.3%, respectively). Gout and HF was 4 times more common in C3 obesity than NW (12.7% vs. 44.5%, and 1.6% vs. 7.4%, respectively), and Type 2 diabetes was 3.5 times more common (10.5% vs. 35.0%, respectively). Psychological comorbidities, including depression and anxiety, became more common with increasing BMI category, but these were not statistically significant. In addition, dyslipidemia, asthma, and chronic kidney disease/end-stage renal disease, although not higher with each increase in BMI category, were significantly higher in those with obesity compared to NW and/or OW. Overall, relative to NW respondents, those with C3 obesity had more obesity-related complications (2.07 vs. 4.62, respectively; p < 0.001). In the multivariable regression, the incidence rate ratios (IRRs) of the total number of obesity-related complications were 1.237 (p < 0.001), 1.464 (p < 0.001), 1.700 (p < 0.001), and 1.967 (p < 0.001) for those with OW, C1, C2 and C3 obesity, respectively, relative to those with NW (Table 2).
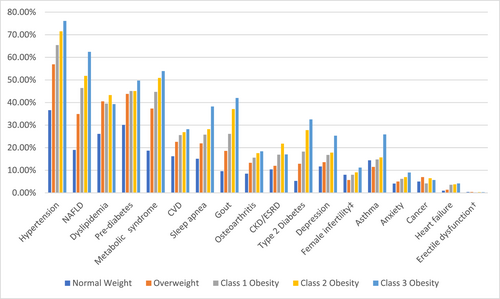
The prevalence of obesity-related complications among the population with overweight (OW) or obesity using body mass index (BMI) category, National Health and Nutrition Examination Survey (NHANES) 2017–2018. ‡ Among females only, † among males only. CVD, cardiovascular disease; ESRD, end-stage renal disease; HF, heart failure; NAFLD, non-alcoholic fatty liver disease.
| NHANES sample | MEPS sample | |||||||
|---|---|---|---|---|---|---|---|---|
| # comorbidities (n = 4286) | ≥5% weight loss (n = 4933) | # of weight loss methods (n = 4933) | # of days missed due to illness or injury (n = 20,312) | Limited ability to work (n = 20,312) | Inability to work (n = 20,312) | Physical component score SF-12 (n = 20,312) | Mental component score SF-12 (n = 20,312) | |
| IRR | OR | IRR | IRR | OR | OR | Exp(b) | Exp(b) | |
| Overweight | 1.237*** (p < 0.001) | 0.958 (p = 0.841) | 2.015*** (p < 0.001) | 1.488*** (p < 0.001) | 0.974 (p = 0.741) | 0.98 (p = 0.779) | 0.989*** (p = 0.002) | 0.997 (p = 0.378) |
| C1 obesity | 1.464*** (p < 0.001) | 0.836 (p = 0.450) | 2.925*** (p < 0.001) | 1.696*** (p < 0.001) | 1.330*** (p < 0.001) | 1.251*** (p = 0.005) | 0.960*** (p < 0.001) | 0.984*** (p < 0.001) |
| C2 obesity | 1.700*** (p < 0.001) | 1.071 (p = 0.808) | 3.452*** (p < 0.001) | 1.436*** (p < 0.001) | 1.596*** (p < 0.001) | 1.612*** (p < 0.001) | 0.932*** (p < 0.001) | 0.979*** (p < 0.001) |
| C3 obesity | 1.967*** (p < 0.001) | 1.144 (p = 0.573) | 3.831*** (p < 0.001) | 1.606*** (p < 0.001) | 2.731*** (p < 0.001) | 2.554*** (p < 0.001) | 0.863*** (p < 0.001) | 0.962*** (p < 0.001) |
- Note: Exp(b) denotes that the estimated coefficient from the log-link model is exponentiated for ease of interpretation.
- Abbreviations: IRR, Incidence Rate Ratio; NHANES, National Health and Nutrition Examination Survey; OR, Odds ratio.
- p-value in parentheses, ***p < 0.01, **p < 0.05, *p < 0.1.
3.3 Weight loss history
The proportion of respondents reporting weight loss attempts in the previous 12 months significantly increased with increasing BMI category (NW: 16.0%; OW: 35.2%; C1: 43.5%; C2: 46.9%; C3: 57.4%, p < 0.001). The mean total number of weight loss methods attempted followed the same pattern (NW: 1.3; OW: 2.9; C1: 3.4; C2: 3.7; C3: 4.2 p < 0.001). Across all BMI categories, following general dietary guidelines and using an evidence-based lifestyle modification were the most frequently reported weight loss methods, while commercial and unhealthy methods were the least common. Only 5.2% of respondents with C3 obesity used prescription AOMs in the previous 12 months and 3.7% had a lifetime history of weight loss surgery (Table 1). Controlling for demographic and socioeconomic variables, regression results indicate that the number of weight loss attempts increased with increasing BMI. Relative to respondents with NW, the IRRs of the total number of weight loss attempts were 2.015 (p < 0.001), 2.925 (p < 0.001), 3.452 (p < 0.001), and 3.831 (p < 0.001) for those with OW, C1, C2 and C3 obesity, respectively (Table 2). Correspondingly, the proportion of respondents who achieved clinically meaningful weight loss (≥5% body weight) over the previous 12 months significantly increased with increasing BMI category up to C2 obesity (NW: 0.8%; OW: 2.9%; C1: 4.3%; C2: 4.8%; C3: 4.0%, p = 0.005) (Table 1). However, respondents across all BMI categories, on average, gained weight over the previous 12 months. Weight gain tended to be positively skewed as there were outliers who gained over 100 lbs. thus, the mean estimates tended to be higher. Median weight gained in the previous 12 months for NW individuals was 6.68 lbs., whereas individuals with OW or obesity gained 3–4 lbs., (OW: 3.95 lbs., C1: 3.57 lbs., C2: 4.15 lbs., C3: 3.15 lbs., p < 0.001 across all BMI categories) (Table 1).
4 MEDICAL EXPENDITURE PANEL SURVEY COHORT RESULTS
4.1 Health-related quality of life
Higher BMI was associated with significantly lower scores on both SF-12 PCS and MCS (Table 3). The median PCS score was 55.86 for NW respondents, while respondents with OW, C1, C2 and C3 obesity had a median PCS score of 54.52, 52.83, 51.28, and 47.21, respectively (p < 0.001). The median MCS score for respondents who were NW, OW, C1, C2, and C3 obesity was 54.74, 54.96, 54.59, 54.20, and 52.41, respectively (p < 0.001) (Table 3). When controlling for demographic and socioeconomic factors, the multivariable regression analysis showed that as BMI severity increased, both PCS and MCS scores decreased. Relative to the NW group, higher BMI had an increasing adverse and significant effect on physical functioning (PCS) in the OW, C1, C2, and C3 groups, and on MCS in the C1, C2, and C3 groups (Table 2).
| Normal (N = 6244, 29%) | OW (N = 7877, 34.5%) | C1 obesity (N = 4952, 21%) | C2 obesity (N = 2235, 9.5%) | C3 obesity (N = 1516, 6%) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Employment/productivity | |||||||||||
| Employed, n % | 4057 | 64.9% | 5301 | 67.3% | 3261 | 65.9% | 1429 | 63.9% | 908 | 59.9% | 0.002 |
| Missing work due to illness/injury, mean [median] | 1.71 | [0] | 2.30 | [0] | 2.47 | [1] | 2.66 | [1] | 2.92 | [1] | <0.001 |
| Inability to work, n % | 644 | 10.3% | 879 | 11.2% | 723 | 14.6% | 398 | 17.8% | 408 | 26.9% | <0.001 |
| Limited ability to work, n % | 687 | 11.0% | 940 | 11.9% | 771 | 15.6% | 420 | 18.8% | 426 | 28.1% | <0.001 |
| Healthcare visits | |||||||||||
| Outpatient, mean [median] | 0.5 | [0] | 0.51 | [0] | 0.58 | [0] | 0.77 | [0] | 0.8 | [0] | 0.007 |
| ER, mean [median] | 0.17 | [0] | 0.18 | [0] | 0.22 | [0] | 0.24 | [0] | 0.35 | [0] | <0.001 |
| Inpatient, mean [median] | 0.08 | [0] | 0.1 | [0] | 0.11 | [0] | 0.11 | [0] | 0.14 | [0] | <0.001 |
| Healthcare expenditures (2019 USD) | |||||||||||
| Total, mean [median] | $5236 | [$1120] | $5665 | [$1304] | $6656 | [$1652] | $8169 | [$2279] | $9212 | [$2468] | <0.001 |
| Prescription, mean [median] | $1232 | [$30] | $1270 | [$70] | $1899 | [$156] | $2254 | [233] | $2954 | [331] | <0.001 |
| Outpatient, mean [median] | $408 | [$0] | $525 | [$0] | $525 | [$0] | $952 | [$0] | $837 | [$0] | 0.008 |
| Inpatient, mean [median] | $1207 | [$0] | $1482 | [$0] | $1596 | [$0] | $1809 | [$0] | $2050 | [$0] | 0.025 |
| ER, mean [median] | $187 | [$0] | $222 | [$0] | $244 | [$0] | $288 | [$0] | $341 | [$0] | 0.002 |
| OOP RX, mean [median] | $166 | [$0] | $165 | [$0] | $214 | [$0] | $298 | [$0] | $287 | [$0] | <0.001 |
| OOP total, mean [median] | $813 | [$0] | $761 | [$0] | $773 | [$0] | $915 | [$0] | $790 | [$0] | 0.136 |
| SF-12 component scores | |||||||||||
| Physical component summary, mean [median] | 52.03 | [55.86] | 50.59 | [54.52] | 48.64 | [52.83] | 47.24 | [51.28] | 43.47 | [47.21] | <0.001 |
| Mental component summary, mean [median] | 52.35 | [54.74] | 52.63 | [54.96] | 51.89 | [54.59] | 51.43 | [54.2] | 50.20 | [52.41] | <0.001 |
- Abbreviation: OOP, out of pocket.
4.2 Productivity
The proportion of respondents who reported an inability to work increased significantly (p < 0.001) with increasing BMI category (NW: 10.3%; OW: 11.2%; C1: 14.6%; C2: 17.8%; C3: 26.9%) (Table 3). In models controlling for demographic and socioeconomic variables, the odds-ratio of reporting an inability to work did not differ significantly between OW and NW respondents (p = 0.77) (Table 2). In contrast, the odds-ratio of reporting an inability to work among respondents with obesity was higher when compared to NW individuals (C1: 1.251, p = 0.005; C2: 1.612, p < 0.001; C3: 2.55, p < 0.001) (Table 2).
Having a limited ability to work was significantly (p < 0.001) more likely to increasing BMI category. Respondents with C3 obesity (426, 28.1%) were more than twice as likely to have a limited ability to work compared to those with OW (940, 11.9%) or NW (687, 11.0%) (Table 2). After controlling for demographic and socioeconomic factors, respondents with obesity had higher odds of having a limited ability to work relative to NW respondents (OR C1: 1.330, p < 0.001; OR C2: 1.596, p < 0.001; OR C3: 2.731, p < 0.001) (Table 2). The odds-ratio of having limited ability to work did not differ significantly between OW and NW respondents (OR: 0.958, p = 0.87).
Compared to NW respondents (1.71 days per 6 months), the respondents in all the other BMI categories missed significantly more days of work due to illness or injury (OW: 2.30; C1: 2.47; C2: 2.66, C3: 2.92 days per 6 months; p < 0.001). After adjusting for demographic and socioeconomic factors, results from the negative binomial regression indicate that respondents with OW or obesity had higher rates of missing days of work due to illness or injury relative to respondents with NW (IRR of OW: 1.488, p < 0.001; C1: 1.696, p < 0.001; C2: 1.436, p < 0.001; C3: 1.606, p < 0.001) (Table 2).
4.3 Healthcare expenditures
Healthcare expenditures, adjusted to the 2019 consumer price index, significantly increased with increasing BMI category (Table 2). The average total annual expenditures among respondents with C3 obesity were 60% higher than for NW respondents ($9212 vs. $5,236, respectively; p < 0.001). Also, the average annual prescription drug expenditures were more than double for respondents with C3 obesity compared to NW respondents ($2954 vs. $1,232, respectively; p < 0.001). Annual expenditures were driven largely by inpatient and pharmacy costs, which increased with increasing BMI (Table 2).
5 DISCUSSION
Using recent nationally representative data, this study found that health and economic burden is higher among respondents with OW or obesity compared to those with NW, and that this burden increases significantly with increasing BMI category. Relative to NW respondents, those with C3 obesity had more obesity-related complications (2.07 vs. 4.62, respectively; p < 0.001) and were up to 4 times as likely to have the following conditions: hypertension, metabolic syndrome, NAFLD, Type 2 diabetes, gout, CVD, HF, sleep apnea, and osteoarthritis. Studies using national survey data have previously documented a substantially increased risk of certain obesity-related complications, such as Type 2 diabetes, with increasing BMI.28, 29 In the 2001 Behavioral Risk Factor Surveillance System survey, for example, 7.3% of respondents who were OW and 25.6% of respondents with C3 obesity had self-reported Type 2 diabetes.29 The current study used national survey data to assess the presence of 18 obesity-related complications to comprehensively capture the multimorbidity associated with obesity.
The greater proportion of respondents attempting to lose weight in each higher BMI category, as well as the greater number of weight loss methods used in each higher category, suggests that there may be an increased desire to reduce weight as BMI increases. Weight loss strategies that focus on lifestyle modification (changing diet, eating less, exercising more) were more frequently used by those with higher BMI and in some instances unhealthy methods, such as skipping meals, were used more frequently as well. Weight loss surgery and the use of prescription AOMs also increased with increasing BMI, but relative to the other methods, they were utilized only by a very small proportion of those with OW or obesity. Our estimates of prescription AOM utilization in the last 12 months among those with OW or obesity were consistent with previous estimates.14, 15 As the number of weight loss attempts increased with higher BMI categories, there was a modest increase in the likelihood of these respondents (OW, C1, C2, C3) achieving clinically meaningful weight loss. However, the overall success rate was low, and on average, respondents in each BMI category gained weight. This is consistent with the progressive and chronic nature of obesity, and the known limited effectiveness of lifestyle modification alone for the treatment of this disease. Physician understanding of and confidence in AOM prescribing need to be improved along with initiatives to improve access to AOM treatment, including their costs and coverage may also be warranted.
In addition, this study contributes to the existing body of evidence demonstrating the adverse impact of obesity on HRQoL,5-7, 30, 31 mobility,30, 32, 33 and productivity/disability.22, 32, 34-40 The evidence suggests that weight reduction improves HRQoL,5-7, 10, 41 particularly the physical domains of HRQoL,41, 42 consistent with our finding that the decline in HRQoL associated with higher obesity class was greater for the SF-12 PCS than MCS. A review of the literature found that the odds of missing work due to illness or injury ranged from 1.15 to 2.8 for those with obesity relative to those with OW.37 Our estimated odds of having a limited ability to work, which could include missing work, for those with obesity relative to NW ranged from 1.3 to 2.7.
A systematic review found that direct costs (treatment and management of the diseases, e.g., inpatient or outpatient care) related to obesity represented a significant amount of cost to the system.43 Another study estimated that the total costs of OW and obesity could cost up to 2.90% of a country's gross domestic product on average and rise to 3.29% by 2060.44 Intervention with AOM has the potential to reduce the cost burden related to ORCs and lost workplace productivity.
This study had some limitations. First, information on obesity-related complications, historical body weight, and weight loss methods attempted was self-reported in NHANES, as were current height and weight (and therefore BMI) in MEPS, and thus subject to recall bias and misreporting. We have attempted to correct for reporting bias in current BMI in the MEPS cohort, but some bias could remain. Moreover, regarding how obesity-related complications were collected, some conditions could have been misreported. Additionally, BMI is not a perfect measure of obesity/adiposity, and it is possible that the study missed unmet needs and high-risk groups within each BMI category based on other measures of adiposity. Given the cross-sectional design of NHANES, our multivariable analysis could not identify causal relationship of OW and obesity with health, HRQoL, and economic outcomes. Lastly, not all the outcomes of interest were available in a single data source or for the same patient cohort, hence we evaluated outcomes for patients meeting the same inclusion/exclusion criteria using two nationally representative surveys.
In conclusion, the health and economic burden of excess body weight in the United States between 2017 and 2018 was high among individuals with OW or obesity and increased with higher BMI categories. Severe obesity, measured by BMI category, was associated with a greater number of obesity-related complications, loss of productivity, lower HRQoL, and higher healthcare expenditures. While weight loss strategies that focus on changing diet and exercise were commonly utilized by those with greater obesity severity, evidence-based weight management strategies such as prescription AOMs and bariatric surgery were underutilized. Despite high counts of weight loss attempts, most respondents with OW or obesity did not achieve clinically meaningful weight loss. Greater utilization of existing and future evidence-based treatment strategies may lead to more clinically meaningful weight reduction and better health and economic outcomes in individuals with OW or obesity.
ACKNOWLEDGMENTS
The authors would like to thank Ronaé McLin, Richard Murphy, Emma Sondergaard Jensen, Jonathan Wong, and Katie Everson for research, writing, editing, and data programming support.
CONFLICT OF INTEREST STATEMENT
Joanna MacEwan is a current employee of Genesis Research Group and a former employee of PRECISIONheor, which are both research consultancies in the health and life science industries. Kevin Chiu is a current employee of Santa Clara Unive and a former employee of PRECISIONheor. Hong Kan, Nadia N. Ahmad, Shraddha Shinde, and Jiat Ling Poon are employees and shareholders of Eli Lilly and Co.