Variation in executive function relates to BMI increases in youth who were initially of a healthy weight in the ABCD Study
Abstract
Objective
The study aim was to determine whether (A) differences in executive function (EF) and cognition precede weight gain or (B) weight gain causes changes to EF and cognition.
Methods
Data were gathered from the Adolescent Brain Cognitive Development (ABCD) Study (release 4.0; ages 9–12 years old [N = 2794]; 100% had healthy weight at baseline [i.e., 9/10 years old], 12.4% had unhealthy weight by ages 11/12 years). EF and cognition were assessed across several domains (e.g., impulsivity, inhibitory control, processing speed, memory); BMI was calculated from height and weight. Nested random-effects mixed models examined (A) BMI ~ EF × Time (i.e., variation in EF/cognition precedes weight gain) and (B) EF ~ BMI × Time (weight gain causes changes to EF/cognition) and controlled for sex, puberty, and caregiver education; random effects were site and subject.
Results
Variation in impulsivity, memory, learning, and processing speed was associated with greater increases in BMI trajectories from 9 to 12 years old. Weight gain was associated with a decrease in inhibitory control, but no other associations were observed.
Conclusions
Underlying variation in EF and cognition may be important for weight gain, but 2 years of weight gain may not be enough to have clinical implications for EF and cognition beyond inhibitory control. These findings suggest that more attention should be paid to the inclusion of EF programs in obesity prevention efforts.
Study Importance
What is already known?
- Several studies have shown that variation in executive function (EF) and cognition is related to overeating and obesity. However, the mechanisms are unknown as to what comes first: do underlying differences in EF “cause” obesity (via poor food choices), or does weight gain have negative “consequences” on EF?
What does this study add?
- This study evaluated the natural progression of weight gain and EF and cognitive development while testing two theoretical cause-versus-consequence models in a sample of youth who at baseline (i.e., ages 9/10 years) initially had a healthy weight (12% had overweight by ages 11/12 years). We found support for the notion that underlying variation in EF and cognition relates to weight gain but found less support for the idea that weight gain is related to changes in EF and cognition.
How might these results change the direction of research or the focus of clinical practice?
- Understanding the natural trajectory of weight gain and EF and cognitive development has clinical implications for treatment programs. Importantly, our results showed that 2 years may not be enough time (or not enough weight was gained) to observe clinical effects on EF or cognition during development. This suggests that, if intervention occurs early, it may be able to prevent long-term negative cognitive outcomes.
INTRODUCTION
Prior to the COVID-19 pandemic, 20% of US children had obesity [(1)], but the disruption of daily routines (e.g., diminished physical activity, increased food access) has increased rates dramatically [(2)]. Childhood obesity is associated with several preventable early onset medical comorbidities such as diabetes, cardiovascular disease, cancer, and dementia [(3)]. Because it is highly likely that children with obesity will become adults with obesity [(4)], there is a dire need to understand its causes and create effective interventions. Although the contributing causal factors of obesity are vast and multidimensional [(3)], it is undeniable that the brain plays a key role in facilitating and maintaining obesity [(5)]: internal signals (e.g., neurotransmitters, gut hormones) initiate and terminate food intake to maintain homeostasis. However, external stimuli (e.g., visual stimuli, taste, smell) can override homeostatic mechanisms and induce hedonic overeating at times when energy reserves are plenty (i.e., eating in the absence of hunger) [(6)]. Hedonic overeating is thought to be controlled by brain processes that are involved in executive function (EF) [(7)].
The most common definition of EF includes three cores: cognitive flexibility, working memory, and inhibition, which then relate to higher order EF domains such as reasoning, planning, and problem solving [(8, 9)]. In the current article, we expanded the definition of EF to include domains that do not typically fall within these core functions (e.g., reading comprehension, picture vocabulary), as others have advocated for a broader framework [(10, 11)] that is not limited to traditional definitions [(8, 9)]. For instance, measures of impulsivity are better integrated in hot versus cold EF models as these arguably could be reflective of failures in top-down regulation (cold system, inhibition) [(12)]. This broader framework was chosen because these processes facilitate other cognitive abilities and regulate behavior; deficits in these processes are thought to have maladaptive consequences (e.g., poor eating habits, smoking) [(13)]. In both adults and children, behavioral deficits in EF have been associated with obesity [(14-18)], increased food intake [(19)], and continued weight gain [(12)]. The dual processes model of overeating postulates that hedonic overeating and subsequent weight gain may be related to an underlying inability to suppress unnecessary food intake (i.e., deficits in EF) [(9)]. However, animal models have shown that overeating has downstream effects on cognition, like EF [(20)]. Thus, we postulated that weight gain has a causal role in EF deficits.
To date, most studies evaluating the relationship between EF and weight status have been cross-sectional, limited in scope, or conducted in small samples. Thus, the mechanism underlying EF's role in obesity facilitation and maintenance is unknown. Furthermore, little is known about which EF domains are most related to unhealthy weight gain. Moreover, childhood through adolescence is a period in which the brain is undergoing rapid changes in several regions associated with EF [(21)]. However, it is unknown (A) whether weight gain during this time disrupts or accelerates normative development or its functional consequences and (B) which EF domains may be more sensitive to weight gain during this critical time. Understanding how EF and weight gain coincide during development may offer potential insights for behavioral (e.g., neurocognitive) treatment and intervention programs.
In the current article, we evaluated whether (A) differences in EF and cognition precede weight gain (i.e., the dual processes model of overeating) or (B) weight gain causes changes to EF and cognition. Weight gain was modeled with respect to changes in body mass index (BMI; such that a positive change would be a proxy for weight gain) across a 2-year period in pre- and early adolescence in a subsample of youth enrolled in the Adolescent Brain Cognitive Development (ABCD) Study® (n = 2825; ages 9/10 years to 11/12 years; release 4.0). Importantly, these associations were evaluated in a subsample of youth who had a healthy weight at baseline (i.e., 9/10 years old). As some of these youth (n = 347) transitioned to unhealthy weight (e.g., overweight/obesity) within a 2-year period, the current study can evaluate the natural concurrent progressions of changes to EF and cognition and BMI. Here, we report findings across multidimensional aspects of EF and cognition to better understand how differences in EF and cognition may predispose some youth to gain unhealthy weight and how BMI relates to changes to EF and cognition.
METHODS
Study design
The ABCD Study is a 21-site 10-year cohort study that enrolled 11,878 youth aged 9/10 years old at baseline (August 2016 to October 2018). Recruitment was tailored to match the demographic population of the US Census. Details pertaining to study design, assessments, objectives, and protocols have been published in numerous documents and on the study website (www.ABCDStudy.org). Assessments are conducted annually, but the protocol is varied. Broadly, the ABCD Study was designed to assess cognitive and health development throughout adolescence. The current article focused on assessments from baseline (9/10 years old) and the 2-year follow-up (11/12 years old), and analyses were restricted to a subset of youth who initially had a healthy weight with useable data at each time point (n = 2794, 12.4% had overweight/obesity by ages 11/12 years, 51.2% male, 72.8% White). Details pertaining to overall ABCD Study inclusion as well as exclusion criteria that were applied to obtain a sample optimal for our analyses are available in online Supporting Information. Assessments included in this article were limited to anthropometrics, demographics, and task- and questionnaire-based assessments of EF and cognition. A centralized Institutional Review Board was approved by the University of California, San Diego.
Physical health assessments
Participants were weighed to the nearest 0.1 in at each visit by a trained researcher in light clothing using a physician's scale (Detecto model 439, Webb City, Missouri). Height was assessed on the same scale, with the youth's heels against the height rod. Two measurements were acquired, and a third was taken if measurements varied by more than one-fourth of an inch or 0.1 lb. Height and weight were converted to BMI (kilograms/meters squared) and BMI percentiles according to the Centers for Disease Control and Prevention (CDC) sex-age-height-weight specific growth charts [(22)] for clinical interpretations. Unadjusted (raw) BMI values were used in the statistical analyses to evaluate within-subject change. The pubertal development scale [(23)] was administered yearly to caregivers and youth. Details regarding physical health assessments have been published elsewhere [(24)] and in online Supporting Information.
Demographics
Caregivers reported on the youth's race and ethnicity, sex at birth, date of birth, family structure, and socioeconomic status (e.g., education) of the family (see online Supporting Information for details).
EF and cognitive assessment
Biennial assessments of EF and cognition were conducted at baseline and the 2-year follow-up. EF trait-based questionnaires that measured impulsivity and (the lack of) inhibition and that measured reward responsiveness consisted of the Behavioral Inhibition System/Behavioral Approach System (BIS/BAS) and of the Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behavioral Scale (UPPS-P [i.e., impulsivity assessment]). EF and cognitive tasks included assessments of inhibitory control, proxies of working memory, processing speed, verbal and visual learning and memory, and vocabulary; they were assessed with the National Institutes of Health (NIH) Toolbox, the Rey Auditory Verbal Learning Test (RAVLT), and the Little Man Task. Although not all measures fit the common definition of EF, these were close approximations, so we will use the term EF to refer to both classic EF and other cognitive processes that depend on optimal EF. Details of these assessments are available elsewhere [(24)] and in online Supporting Information.
Linear mixed-effects modeling
RESULTS
General results
The number of participants included for each analysis differed across tasks (see online Supporting Information for the N's included per task; Table 1 displays the demographics). At baseline, all youth had a healthy weight, but by the 2-year follow-up, 323 youth transitioned to have overweight (11.6%), and 23 transitioned to have obesity (0.8%). Additionally, by the 2-year follow-up, 151 youth had extreme weight gain (as defined in [(27)]), whereas 38 youth had extreme weight gain but were still classified as having a healthy weight at the 2-year follow-up. Notably, the demographics of the sample included in the analyses did differ from the entire sample with regard to race, ethnicity, and education. Figure 1 displays the distribution of BMI and weight status for each year of data collection.
| Variable | Whole sample (n = 11,878) | Subsample (n = 2794) | p | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (mo) | |||||
| Baseline | 119 | 7.5 | 119 | 7.0 | 0.741 |
| Y2 | 143.5 | 7.6 | 142.8 | 7.0 | <0.001 |
| Puberty | |||||
| Baseline | 2 | 0.8 | 1.9 | 0.8 | <0.001 |
| Y2 | 2.7 | 1 | 2.6 | 1 | <0.001 |
| BMI (kg/m2) | |||||
| Baseline | 18.8 | 3.8 | 17.0 | 1.4 | <0.001 |
| Y2 | 20.6 | 4.6 | 18.7 | 2.1 | <0.001 |
| Variable | n | % | n | % | p |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 6192 | 52.1 | 1425 | 51.0 | 0.390 |
| Female | 5683 | 47.8 | 1369 | 49.0 | |
| Missing | 3 | ||||
| Race | |||||
| White | 7524 | 64.3 | 2032 | 72.7 | <0.001 |
| Black | 1869 | 16 | 277 | 9.9 | |
| Asian | 275 | 2.3 | 75 | 2.7 | |
| AIAN/NHPI | 78 | 0.7 | 22 | 0.8 | |
| Other | 525 | 4.5 | 96 | 3.4 | |
| Multi-race | 1434 | 12.3 | 277 | 10.5 | |
| Ethnicity | |||||
| Hispanic | 2411 | 20.6 | 414 | 14.8 | <0.001 |
| Non-Hispanic | 9312 | 79.4 | 2380 | 85.2 | |
| Caregiver report of education | |||||
| <HS | 568 | 4.8 | 76 | 2.7 | <0.001 |
| HS/GED | 1079 | 9.1 | 143 | 5.1 | |
| Some college | 2978 | 25.1 | 592 | 21.2 | |
| BA degree | 2969 | 25 | 803 | 28.7 | |
| Postgraduate degree | 3987 | 33.6 | 1180 | 42.2 | |
| Missing | 295 | 2.5 | |||
| Baseline weight class | |||||
| Underweight | 468 | 3.9 | |||
| Healthy weight | 7601 | 64.0 | 2794 | 100 | <0.001 |
| Overweight | 1801 | 15.2 | |||
| Obesity | 1992 | 16.8 | |||
| Missing | 16 | 0.1 | |||
| Y2 weight class | |||||
| Underweight | 286 | 2.7 | |||
| Healthy weight | 4818 | 46.3 | 2448 | 87.6 | <0.001 |
| Overweight | 1216 | 11.7 | 323 | 11.6 | |
| Obesity | 1381 | 13.3 | 23 | 0.8 | |
| Missing | 2714 | 26.1 | |||
- Note: Participant characteristics are displayed for the largest possible N (i.e., those who had complete data for the Urgency, Premeditation [lack of], Perseverance [lack of], Sensation Seeking, Positive Urgency, Impulsive Behavioral Scale [UPPS-P] and Behavioral Inhibition System/Behavioral Approach System [BIS/BAS] questionnaires). Thus, the participant characteristics may differ slightly for those youth who were included in the NIH Toolbox, the Rey Auditory Verbal Learning Test, and the Little Man Task analysis. Descriptive statistics are displayed by caregiver self-reported race only for interpretation of sample diversity. P values reflect χ2 and t tests where appropriate. Puberty scores reflect an averaged caregiver and child report of Tanner staging (range 1-5).
- Abbreviations: AIAN/NHPI, American Indian, Alaska Native/Native Hawaiian, Pacific Islander; BA, bachelor's degree; GED, general equivalency diploma; HS, high school; Y2, year 2 follow-up.

Do underlying differences in EF relate to greater increases in BMI? A test of the dual processes model of overeating
UPPS-P
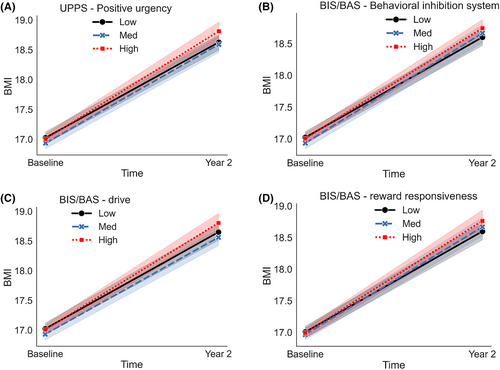
Significant EF × Time interaction effects on BMI were observed for the positive urgency subscale, in which greater positive urgency scores were associated with greater increases in the rate of change in BMI over 2 years (β = 0.12, p < 0.001, Figure 2A). No other associations were observed, and all results are reported in Table 2.
| Interaction | β | 95% CI | df | t statistic | p | Significance |
|---|---|---|---|---|---|---|
| UPPS-P | ||||||
| Negative urgency × Time | 0.05 | [−0.02 to 0.12] | 3192.98 | 1.36 | 0.17 | |
| Lack of planning × Time | 0 | [−0.06 to 0.07] | 3096.1 | 0.06 | 0.95 | |
| Sensation seeking × Time | 0 | [−0.06 to 0.07] | 3007.36 | 0.13 | 0.89 | |
| Positive urgency × Time | 0.12 | [0.06 to 0.19] | 3144.44 | 3.63 | <0.001 | ***a |
| Lack of perseverance × Time | 0.04 | [−0.02 to 0.1] | 3052.97 | 1.19 | 0.23 | |
| BIS/BAS | ||||||
| BIS × Time | 0.08 | [0.02 to 0.15] | 3146.54 | 2.42 | 0.02 | *a |
| Drive × Time | 0.08 | [0.01 to 0.15] | 3155.46 | 2.38 | 0.02 | *a |
| Reward response × Time | 0.07 | [0.0 to 0.14] | 3233.14 | 1.96 | 0.05 | * |
| Fun seeking × Time | 0.03 | [−0.04 to 0.1] | 3212.09 | 0.84 | 0.4 | |
| Little Man Task | ||||||
| Efficiency × Time | 0.09 | [0.02 to 0.164] | 3574.21 | 2.51 | 0.01 | *a |
| NIH Toolbox | ||||||
| Flanker Inhibitory Control × Time | −0.08 | [−0.15 to −0.0] | 2981.9 | −2.1 | 0.04 | *a |
| Picture Vocabulary × Time | −0.08 | [−0.14 to −0.02] | 2687.8 | −2.4 | 0.02 | *a |
| Pattern Comparison × Time | −0.07 | [−0.15 to 0.0] | 2875.43 | −1.94 | 0.05 | |
| Reading Comprehension × Time | −0.08 | [−0.14 to −0.01] | 2645.87 | −2.35 | 0.02 | *a |
| Picture Sequence Memory × Time | −0.1 | [−0.16 to −0.03] | 2928.79 | −2.7 | <0.01 | **a |
| RAVLT | ||||||
| Learning × Time | −0.125 | [−0.195 to −0.054] | 2286.903 | −3.465 | 0.001 | ***a |
| List B correct × Time | −0.148 | [−0.223 to −0.074] | 2475.644 | −3.898 | <0.001 | ***a |
| Immediate Delay × Time | −0.143 | [−0.215 to −0.072] | 2325.556 | −3.93 | <0.001 | ***a |
| Long Delay × Time | −0.146 | [−0.217 to −0.075] | 2303.462 | −4.016 | <0.001 | ***a |
| Repetition List B × Time | 0.015 | [−0.066 to 0.096] | 2781.802 | 0.356 | 0.722 | |
| Repetition Immediate Delay × Time | 0.024 | [−0.056 to 0.103] | 2707.237 | 0.582 | 0.561 | |
| Repetition Long Delay × Time | −0.039 | [−0.121 to 0.044] | 2694.271 | −0.912 | 0.362 | |
| Total Repetitions × Time | −0.009 | [−0.085 to 0.067] | 2490.833 | −0.232 | 0.816 | |
| Intrusions List B × Time | 0.022 | [−0.06 to 0.104] | 2826.468 | 0.52 | 0.603 | |
| Intrusions Immediate Delay × Time | −0.059 | [−0.141 to 0.022] | 2837.695 | −1.423 | 0.155 | |
| Intrusions Long Delay × Time | −0.005 | [−0.086 to 0.076] | 2818.678 | −0.13 | 0.896 | |
- Note: All effects that were significant survived Benjamini-Hochberg correction. Flanker Inhibitory Control and Attention Task was abbreviated in the table to Flanker Inhibitory Control; Pattern Comparison Processing Speed was abbreviated to Pattern Comparison in the table.
- Abbreviations: BIS/BAS, Behavioral Inhibition System/Behavioral Approach System; df, degrees of freedom; RAVLT, Rey Auditory Verbal Learning Test; UPPS-P, Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behaviorial Scale.
- a Survived correction.
- *p < 0.05, **p < 0.01, ***p < 0.001.
BIS/BAS
Significant EF × Time interaction effects on BMI were observed for the drive and the BIS subscales. Youth who scored higher on the drive (e.g., persistent pursuit of desired goals, β = 0.08, p = 0.016) and BIS subscales (e.g., anticipation of punishment, β = 0.08, p = 0.017) had greater increases in the rate of change in BMI over 2 years (Figure 2C,D). No other associations were observed. All results are reported in Table 2.
NIH Toolbox
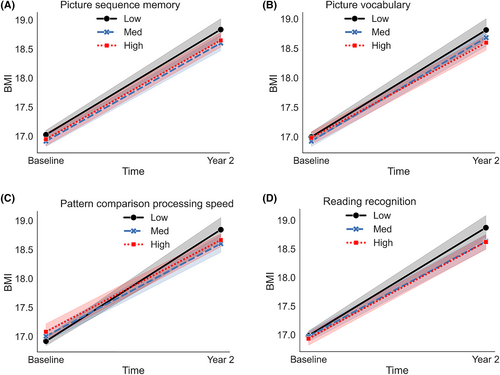
Significant EF × Time interaction effects on BMI were observed for four NIH Toolbox assessments, namely Flanker Inhibitory Control and Attention, Picture Vocabulary, Pattern Comparison Processing Speed, Reading Comprehension, and Picture Sequence Memory. Lower scores on the Flanker Inhibitory Control and Attention (β = −0.08, p = 0.036), Picture Vocabulary (i.e., verbal IQ, β = −0.08, p = 0.017), Reading Comprehension (e.g., language, oral reading, β = −0.08, p = 0.019), and Picture Sequence Memory (e.g., episodic memory, β = −0.1, p = 0.007) were associated with greater increases in the rate of change in BMI over 2 years (Figure 3A–D). All results are reported in Table 2.
Little Man Task
There was a significant EF × Time interaction effect on BMI for efficiency performance on the Little Man Task. Lower efficiency scores (e.g., visuospatial processing, β = −0.13, p = 0.01) were associated with greater increases in the rate of change in BMI over 2 years (Figure 4A). All results are reported in Table 2.
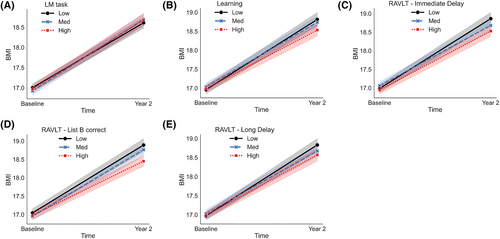
RAVLT
Significant EF × Time interaction effects on BMI were observed for four outcomes on the RAVLT task. Lower scores on the Learning (β = −0.13, p < 0.001), Immediate Recall (β = −0.14, p < 0.001), Long Recall (β = −0.15, p < 0.001), and Interference List B (β = −0.15, p < 0.001) metrics were associated with increases in the rate of BMI over 2 years (Figure 4B–E). All results are reported in Table 2.
Does weight gain lead to variation in EF?
There was a significant BMI × Time interaction effect on the Flanker Inhibitory Control and Attention task (β = −0.60, p = 0.01). No other associations were observed (Table 3).
| Outcome variable | Interaction | β | 95% CI | df | t statistic | p | Significance |
|---|---|---|---|---|---|---|---|
| UPPS-P | |||||||
| Negative urgency | BMI × Time | 0.02 | [−0.12 to 0.15] | 3363.55 | 0.28 | 0.78 | |
| Lack of planning | BMI × Time | −0.06 | [−0.17 to 0.06] | 3314.81 | −1 | 0.32 | |
| Sensation seeking | BMI × Time | 0.08 | [−0.06 to 0.21] | 3263.58 | 1.09 | 0.28 | |
| Positive urgency | BMI × Time | 0.13 | [−0.01 to 0.28] | 3339.42 | 1.78 | 0.08 | |
| Lack of perseverance | BMI × Time | 0.05 | [−0.05 to 0.16] | 3282.29 | 1.01 | 0.31 | |
| BIS/BAS | |||||||
| BIS | BMI × Time | 0.01 | [−0.19 to 0.22] | 3344.46 | 0.13 | 0.89 | |
| Drive | BMI × Time | 0.11 | [−0.04 to 0.26] | 3356.24 | 1.39 | 0.16 | |
| Reward response | BMI × Time | 0.11 | [−0.04 to 0.26] | 3356.24 | 1.39 | 0.16 | |
| Fun seeking | BMI × Time | 0 | [−0.17 to 0.16] | 3359.81 | −0.01 | 0.99 | |
| Little Man Task | |||||||
| Efficiency | BMI × Time | 0 | [−0.0 to 0.0] | 3542.38 | 1.29 | 0.2 | |
| NIH Toolbox | |||||||
| Flanker Inhibitory Control | BMI × Time | −0.59 | [−0.98 to −0.21] | 3212.5 | −3 | <0.01 | **a |
| Picture Vocabulary | BMI × Time | −0.06 | [−0.37 to 0.25] | 3049.55 | −0.36 | 0.72 | |
| Pattern Comparison | BMI × Time | −0.33 | [−1.06 to 0.41] | 3137.93 | −0.87 | 0.38 | |
| Reading Comprehension | BMI × Time | −0.03 | [−0.25 to 0.18] | 2997.16 | −0.3 | 0.76 | |
| Picture Sequence Memory | BMI × Time | 0.36 | [−0.27 to 1.0] | 3172.52 | 1.12 | 0.26 | |
| RAVLT | |||||||
| Learning | BMI × Time | −0.45 | [−0.91 to 0.01] | 2519.61 | −1.91 | 0.06 | |
| List B correct | BMI × Time | −0.08 | [−0.18 to 0.03] | 2637.35 | −1.41 | 0.16 | |
| Immediate Delay | BMI × Time | −0.09 | [−0.24 to 0.05] | 2533.63 | −1.25 | 0.21 | |
| Long Delay | BMI × Time | −0.13 | [−0.29 to 0.02] | 2529.54 | −1.73 | 0.08 | |
| Repetition List B | BMI × Time | −0.01 | [−0.03 to 0.02] | 2831.56 | −0.58 | 0.56 | |
| Repetition Immediate Delay | BMI × Time | 0.04 | [−0.04 to 0.11] | 2767.28 | 0.96 | 0.34 | |
| Repetition Long Delay | BMI × Time | 0.02 | [−0.04 to 0.08] | 2763.25 | 0.68 | 0.50 | |
| Total Repetitions | BMI × Time | −0.03 | [−0.34 to 0.28] | 2653.53 | −0.18 | 0.86 | |
| Intrusions List B | BMI × Time | 0.02 | [−0.02 to 0.06] | 2852.87 | 1.15 | 0.25 | |
| Intrusions Immediate Delay | BMI × Time | −0.04 | [−0.07 to −0.01] | 2834.83 | −2.12 | 0.04 | * |
| Intrusions Long Delay | BMI × Time | 0 | [−0.04 to 0.04] | 2792.81 | 0.02 | 0.99 | |
- Note: All effects that were significant survived Benjamini-Hochberg correction. Flanker Inhibitory Control and Attention task was abbreviated in the table to Flanker Inhibitory Control; Pattern Comparison Processing Speed was abbreviated to Pattern Comparison in the table.
- Abbreviations: BIS/BAS, Behavioral Inhibition System/Behavioral Approach System; df, degrees of freedom; RAVLT, Rey Auditory Verbal Learning Test; UPPS-P, Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behaviorial Scale.
- a Survived correction.
- *p < 0.05, **p < 0.01.
DISCUSSION
Although several studies have suggested that EF is related to overeating and unhealthy weight gain, the mechanisms driving these processes are unknown. To our knowledge, this was the first study to assess the natural progression of changes in BMI and EF over a 2-year period in early adolescence among a sample of youth who initially had a healthy weight at ages 9/10 years old. To this end, we tested whether (A) variation in EF preceded weight gain (i.e., dual processes model of overeating, which postulates that underlying differences in EF contribute to poor food intake decisions) or (B) weight gain had negative consequences on EF [(9, 20, 28)]. Overall, across several assessments of traditional EF (e.g., impulsivity, inhibitory control) and broader cognitive function (e.g., processing span, word recall), we found stronger evidence that underlying differences in EF and cognition may precede weight gain (i.e., dual processes model of overeating). As these underlying differences in EF and other cognitive processes showed greater increases in the rate of change in BMI, this may be due to an inability to make good food-based decisions. Surprisingly, there was less support for the idea that weight gain causes changes to EF and cognition. It is possible that 2 years is not enough time (or that these initially healthy-weight youth did not gain enough weight) to observe weight-related effects on EF. Nevertheless, future studies that follow children over a longer period of time are warranted to determine whether other changes to EF start to occur at a later time.
Differences in EF and their relation to increased weight status: evidence for the dual processes model of overeating
The dual processes model of overeating suggests that underlying differences in EF affect the ability to resist temptation and stick to longer-term plans (e.g., diet adherence, preventing overeating) [(9)]. Essentially, within this framework, the desire to consume a rewarding food is stronger than the ability to stop behavior and adhere to a healthy diet. In our study, we tested this theory by examining how variation in EF and cognition related to the rate of change in BMI over a 2-year period of pre- and early adolescence. Of particular interest was examining the relationship between impulsivity and BMI, as higher scores on impulsivity assessments have been associated with weight gain and food intake across several studies in children [(14, 15, 17, 18)]. Here, impulsivity was indirectly measured with standard and validated trait-based questionnaires (e.g., BIS/BAS, UPPS-P) and tasks (e.g., Flanker Inhibitory Control and Attention–NIH Toolbox). Our results showed that youth who scored higher on trait-based impulsivity measures (e.g., positive urgency, reward responsiveness, drive, and BIS) and lower on inhibitory control assessments (e.g., Flanker Inhibitory Control and Attention) had greater increases in the rate of change in BMI from age 9 years to age 12 years. This suggests that underlying differences in impulsivity may be facilitating increased weight gain. Although the ABCD Study did not assess food intake, we interpret increases in BMI (i.e., weight gain) to be a proxy for overeating, as an energy balance model suggests that weight gain occurs when there is an excess of calories [(29)]. However, future studies are needed to assess the direct mechanism between food intake, unhealthy weight gain, and changes to EF over time. We also acknowledge that there are other factors that may explain these relationships, as environmental factors like socioeconomic status have been associated with both obesity and EF in children [(30-32)]. Notably, our models controlled for caregiver education (a proxy for socioeconomic status), and, as such, we interpret the relationship between impulsivity and weight gain to be independent of socioeconomic status. However, future studies are needed to confirm this relationship. Importantly, our results corroborate the literature showing an association between increased BMI and sensitivity to rewards and punishment [(18)], which are facets of impulsivity.
Although much literature has focused on impulsivity (e.g., reward, inhibitory control) as it relates to food intake and unhealthy weight gain, optimal functioning of other cognitive functions is also integral to making adequate food-based decisions [(33)]. Several studies have noted correlations between these processes and obesity in animals [(34, 35)] and humans [(33, 36, 37)]. Cognitive abilities such as memory interact with basic EF domains to create adaptable responses [(38)]. For example, memories about previously learned associations help to inform consumption based on previous beliefs (such as pleasant or unpleasant experiences) or to inform diet adherence [(33)]. However, memory can help to prevent overeating by providing signals related to satiety (e.g., helping us to remember when we ate last and how full we are) [(39)]. Thus, variation in memory may contribute to issues with appetite control and cause overeating despite not being hungry. As such, this may be one explanation for why steeper increases in the rate of change in BMI over 2 years were related to lower performance on memory and learning paradigms. For example, youth with variation in memory processing may provide inaccurate information about hunger and satiety, which could lead to overeating. Hence, together with the tendency to act impulsively, underlying differences in memory and learning may contribute to unhealthy weight gain. Although our results do confer with cross-sectional studies [(36, 37, 40-42)], future studies are needed to understand the exact physiologic mechanisms or neurocognitive domains driving the associations between cognitive function and weight gain.
Weight gain and its association to changes in EF
BMI was related to the rate of change in performance on the Flanker Inhibitory Control and Attention task; as BMI increased from ages 9/10 to ages 11/12, performance decreased, providing some evidence that weight gain may cause changes to EF [(20)]. However, BMI was not related to changes in any other assessments of EF or cognition. This was somewhat surprising because animal research has shown evidence that overeating and weight gain are related to cognitive deficits via neuroinflammation during adolescence [(34, 35)]. In children, longitudinal studies have suggested that increases in BMI z scores were related to microstructural changes in the nucleus accumbens (a region involved in reward and motivation) in a circular way, such that alterations in this structure were associated with additional weight gain as well as greater intake of high-fat food [(43)]. On the other hand, 2 years of extreme weight gain was related to structural changes in brain regions associated with EF but not trait-based impulsivity [(27)]. Furthermore, in a subsample of healthy-weight youth at baseline, BMI at 9/10 years old was not related to brain structure 2 years later [(44)]. Therefore, it may be that 2 years of human adolescence may not be enough time (or not enough weight was gained among these initially healthy-weight youth) to observe consequences of weight gain on EF (as assessed by questionnaires and tasks). From a prevention and intervention perspective, this lack of findings is encouraging, suggesting that 2 years of weight gain may not lead to long-lasting effects on EF. However, adolescence is also a period of normative development in EF maturation, and it is unknown how weight gain may affect future maturation. Additionally, it is unknown how much weight gain is needed to show effects on EF. As such, future research is needed to understand (A) these associations over a longer period of time; (B) these associations among youth with greater variation in unhealthy weight gain; and (C) whether these associations are due to neuroinflammation or other mechanisms (e.g., vascular, hormonal, metabolic changes).
Implications
EF training has been shown to increase adherence to treatment programs [(28)], but results are largely short-lived as only a few studies showed 10-year effects; while EF training for weight loss is promising, many behavioral programs do not obtain long-term success. One explanation for this could be that we lack a refined understanding of the exact mechanisms of interaction between EF and weight gain and the impact of pubertal development. Therefore, our results do have relevance for treatment programs that may wish to target youth in earlier stages of weight gain, prior to large variability in puberty (although our analyses did control for pubertal effects). Long-term treatment studies are still needed to examine the effects of behavioral treatment programs. Within this vein, optimal functioning of EF can positively contribute to other health-fostering behaviors that go beyond dietary choices; therefore, training may yield crossed benefits with respect to several other quality-of-life determinants (e.g., physical activity, good sleep habits, greater social interactions, academic success) [(13, 45)]. Lastly, since children with obesity are more likely to become adults with obesity [(4)], early interventions may be necessary to prevent the cascade of adverse events often attributed to having obesity. EF training is often not incorporated into daily activities and it is short-term and time-consuming, but our findings also may have benefit forbehavioral lifestyle interventions. Therefore, early life educational programs may benefit by incorporating EF exercises into the core curriculum to strengthen EF early in childhood.
Strengths and limitations
Our study has many strengths, such as evaluating theoretical cause-versus-consequence relationships between EF and cognition and BMI over a 2-year period in a sample of youth who initially had a healthy weight. Notably, the sample used in this study was pooled from a large and geographically diverse group of participants enrolled in the ABCD Study. However, we do recognize the study's limitations. First, the ABCD Study did not collect markers of peripheral (i.e., systemic) or neural inflammation, which effectively limits the insight into the exact causal mechanisms of these relationships apart from the theoretical models [(9, 20)]. Additionally, there were no markers of insulin sensitivity or hormonal and vascular changes, and together this limits the interpretation of our results as to what mechanisms may be driving the association between weight gain and changes to inhibition. Second, the ABCD Study did not collect objective food intake assessments, so it is unknown how our findings relate to actual food intake decisions. Third, it is possible that the EF assessments in the ABCD Study examined general cognitive function, and performance on these tasks may not translate to food-based decision-making. Fourth, the ABCD Study did not assess all components of the NIH Toolbox beyond baseline. Fifth, the sample demographics included in the article differed from the larger consortium participant pool (e.g., higher percentage of youth identifying as White, higher percentage of youth living in families with higher income, lower percentage of youth identifying as Latinx), with the general ABCD Study sample also being relatively homogenous. Relatedly, excluding youth who had overweight or obesity at baseline limits the generalizability of the findings due to potential exclusion of groups who have higher rates of obesity risk (e.g., Black, Latinx). Additionally, we note the limitations of including only individuals with complete data, as this introduces another bias into the data set and dampens the generalizability of the findings. To circumvent bias of a complete case analysis, we ran additional analyses to account for all available data (see online Supporting Information), but the results remained unchanged. However, our results may not be generalizable to diverse groups, and we note that there may have been bias that excluded individuals from participation due to restricting the analyses to only healthy-weight youth. Lastly, BMI is a proxy for adiposity, and the metabolic consequences of an increase in BMI for children are unknown. The ABCD Study did not collect other markers of adiposity or markers of metabolic health.
CONCLUSION
In youth who had a healthy weight at baseline, we found evidence that variation among several EF and cognitive domains was related to a significant increase in the rate of change in BMI over 2 years. This evidence supports the dual processes model of overeating hypothesis, which postulates that underlying differences in EF contribute to poor food intake decisions and subsequent weight gain [(9)]. Specifically, underlying differences in impulsivity and inhibitory control, as well as memory, learning, and processing speed, were all predictive of weight gain. That said, there was less support for the idea that weight gain has negative consequences on EF because greater increases in BMI were related only to decreases in inhibitory control but not to other EF assessments. (e.g., reward, impulsivity, working memory, processing speed). Thus, it may be that 2 years of weight gain affects inhibitory control (i.e., a stopping mechanism), but the amount (or duration) of weight gain may not be enough to have substantial impacts on other EF domains. Moreover, our findings may have implications for prevention programs that may wish to target these cognitive functions to prevent further unhealthy eating and excess weight gain. Additionally, treatment programs may wish to enhance their programs to focus more on strengthening inhibitory control for weight loss success.
AUTHOR CONTRIBUTIONS
Shana Adise wrote the manuscript and performed the analyses with the guidance of Elizabeth R. Sowell, Andrew T. Marshall, Eric Kan, Michael I. Goran, and Kyung E. Rhee. Shana Adise conceptualized and curated the data with the guidance of Elizabeth R. Sowell. Elizabeth R. Sowell provided funding for the project as part of the Adolescent Brain Cognitive Development (ABCD) Study consortium. Lauren Goedde and Jonatan Ottino-Gonzalez contributed to manuscript preparation. All authors contributed feedback and read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors would like to thank the following individuals for their expertise and assistance throughout all aspects of the study: Drs. Stephanie Bodison and Panteha Hayati Rezvan and Ms. Trinh Luu. The authors would also like to thank all of the participants in the ABCD Study.
FUNDING INFORMATION
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM Study (ABCD Study)® (https://abcdstudy.org/), held in the National Institute of Mental Health (NIMH) Data Archive (NDA). The ABCD Study is supported by the National Institutes of Health and National Institute on Drug Abuse and additional federal partners under award numbers U01-DA-041022, U01-DA-041025, U01-DA-041028, U01-DA-041048, U01-DA-041089, U01-DA-041093, U01-DA-041106, U01-DA-041117, U01-DA-041120, U01-DA-041134, U01-DA-041148, U01-DA-041156, U01-DA-041174, U24-DA-041123, U24-DA-041147, U01-DA-050987, U01-DA-050988, U01-DA-050989, U01-DA-051016, U01-DA-051018, U01-DA-051037, U01-DA-051038, and U01-DA-051039. A full list of supporters is available at https://abcdstudy.org/federal-partners/. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators/. The ABCD Study consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This article reflects the views of the authors and may not reflect the opinions or views of the NIH or other ABCD Study consortium investigators. The ABCD Study data repository grows and changes over time. The ABCD Study data used in this report came from https://doi.org/10.15154/1503209. Additional funding from the NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) provided support for SA (K01 DK135847).
CONFLICT OF INTEREST STATEMENT
Michael I. Goran receives book royalties from Penguin Random House for his book Sugarproof. Kyung E. Rhee received funding from the California Initiative for the Advancement of Personalized Medicine. The other authors declared no conflict of interest.