Outcomes of heliox use in children with respiratory compromise: A 10-year single institution experience
The study was presented as a poster in the AAO-HNSF Annual Meeting & OTO Experience at Nashville TS, October 2023.
Abstract
Objective
Heliox, a mixture of helium and oxygen, has been shown to improve laminar airflow and decrease airway resistance in children. This study aims to describe the outcomes of heliox use in children with respiratory compromise and to identify variables associated with a need for airway surgical intervention.
Methods
A retrospective cohort study of patients who received heliox between 2012 and 2022 at a tertiary care children's hospital.
Results
A hundred and thirty-eight heliox treatments were recorded in 119 children. Twelve patients were excluded. Most (n = 100, 84%) patients had significant comorbidities. On average, patients spent a cumulative mean of 94 ± 187 h on heliox therapy per hospital admission. Patients with croup or asthma without known airway pathology presented at an older age than patients with other indications for heliox therapy (4.0 ± 4.7 vs. 2.2 ± 3.6 years, p = 0.04) and were significantly less likely to have background diseases (n = 14, 52% vs. n = 74, 93%, p < 0.0001). Overall, 51 (47.7%) patients were recommended tracheostomy placement, airway reconstruction, or palliative care. Cumulative use of heliox for more than 47 h was associated with an increased risk of needing tracheostomy or airway reconstruction (odds ratio 6.2, 95% confidence intervals 2.56–14.13, p < 0.0001). In multivariable regression analysis, neuromuscular disease, intracranial neuropathology, and cumulative time of heliox were associated with a need for definitive airway intervention.
Conclusions
Heliox may be used as a temporizing agent in children with upper airway obstruction. The effectiveness of heliox use for more than 47 h in children, especially in the presence of neuromuscular disease and intracranial neuropathology should be reconsidered.
Level of evidence: 4.
1 INTRODUCTION
Heliox is a gas mixture of helium and oxygen that is clinically used to improve airflow in children and adults with airway obstruction. The theoretic benefits of heliox are derived from its physical properties because they are related to fluid dynamics. Specifically, the low density of helium may reduce the resistance of airflow in obstructed airways and convert turbulent airflow into a more efficient laminar flow.1, 2 Thus, heliox may result in decreased work of breathing and improved ventilation in patients with airway obstruction.
Several small cohort studies have investigated the therapeutic utility of heliox in children with respiratory compromise. The majority of these studies examined heliox use in children with lower airway disease. The limited, conflicting data suggest that heliox may improve work of breathing, dyspnea, and gas exchange, may be used as a temporizing method until the obstruction subsides, and even may prevent the need for intubation in children with bronchiolitis or asthma exacerbations.1, 3-11 Fewer studies have examined the clinical application of heliox in upper airway obstruction and demonstrated some success in improving respiratory distress in children with croup and post-extubation stridor.1-3, 12 The potential benefit of heliox in children with laryngeal edema and upper airway obstruction secondary to non-croup etiologies has scarcely been studied in several small studies and resulted in mixed findings.3, 4 Hence, to date, there are no guidelines or evidence-based data to direct the decision to treat children with upper airway obstruction with heliox.
Although heliox is a safe intervention without any direct known adverse effects, overutilization of heliox may result in high costs for both the patient and the health system, extended lengths of stay, and delayed definitive care. The primary aim of this retrospective hypothesis-generating study was to describe our experience with heliox use in children with respiratory compromise. The secondary aim was to identify clinical factors that were associated with definitive surgical airway interventions in patients who received heliox. The data generated from this study will be used to pursue further research with higher levels of evidence.
2 METHODS
2.1 Study population and data sources
Institutional review board approval was obtained from the Ann and Robert H. Lurie Children's Hospital of Chicago. A retrospective chart review was performed in which data were extracted from the electronic medical records of patients who underwent heliox treatment between December 2012 and November 2022. Patients were included if they were 18 years old and younger and received heliox treatment for any amount of time and for any indication. Patients who received heliox for croup, bronchiolitis, or asthma were not excluded to avoid selection bias, as some of these patients had significant underlying conditions that could impair their recovery from infection-related airway obstruction. Exclusion criteria included patients older than 18 years and patients who underwent definitive airway surgical intervention (airway reconstruction, cricoid split or tracheostomy placement) prior to heliox initiation during the same admission.
2.2 Study variables and outcomes
Charts were reviewed for demographic data, comorbidities, heliox use, other medical and surgical interventions, and outcomes. To assess cumulative time on heliox, patient records were examined to identify each time heliox was initiated and discontinued during the same hospital admission. The amount of time spent receiving heliox was then calculated for each individual heliox treatment and summed together to the closest hour. Open airway reconstruction or tracheostomy data were identified for the same admission or future admissions.
Patients were considered enteral feed dependent if they required nutrition supplements through nasogastric or gastrostomy tube. The use of systemic steroids, racemic epinephrine, or ciprofloxacin/dexamethasone nebulizers was recorded if patients received any of these medications during the same admission as heliox treatment. Intracranial neuropathology was defined as non-neuromuscular neurologic disorders and structural brain defects (microcephaly, hydrocephalus, intracranial hemorrhage, or encephalopathy).
Heliox was delivered via high-flow nasal cannula at concentrations of 70/30 or 80/20 helium/oxygen as commonly practiced. At our institution, this treatment can only be provided in an intensive care unit (ICU) setting. Due to a lack of guidelines on heliox use, the decision to initiate heliox treatment was at the discretion of the ICU or otolaryngologist clinicians and was based on the increased work of breathing, the presence of stridor, or the degree of respiratory distress.
The need for re-intubation was determined by the ICU clinicians based on the patients' vitals, work of breathing, oxygen levels, and transcutaneous levels of carbon dioxide. The need for tracheostomy tube placement was determined by the ICU and otolaryngology clinicians based on clinical evaluation and commonly-practiced consensus. Airway reconstruction was recommended by the otolaryngologist based on the presence of upper airway obstruction as determined during direct laryngoscopy and bronchoscopy in the operating room in the presence of prolonged or unresponsive respiratory distress. The primary outcome of interest was the need for definitive surgical intervention, defined as airway reconstruction (laryngotracheal reconstruction [LTR] or cricoid split) or tracheostomy tube placement. As secondary outcomes, factors associated with the need for definitive surgical intervention were evaluated.
2.3 Statistical analysis
Baseline characteristics were summarized as means and standard deviations or proportions. Patient age was presented as median and IQRs. For the unadjusted comparisons, group differences between patients who required definitive airway interventions and patients who were able to wean off heliox were assessed using student t-test. Categorical variables were tested with Chi-square or Fisher's exact tests as appropriate. A correction method was not applied for categorical variables in the multiple comparisons. To avoid type I errors, p-values were not calculated for the sub-categories.
The relationship between the need for definitive airway intervention and variables of interest was modeled with multivariable logistic regression to attain risk-adjusted odds ratios (ORs) and corresponding 95% confidence intervals (95% CI). Independent variables included in models were chosen based on the hypothesized clinical significance or p-value < 0.2 on comparison of baseline characteristics. Covariates included: the presence of genetic anomaly or syndrome, bronchopulmonary disease, hypotonia or neuromuscular disease, secondary airway lesion, intracranial neuropathology, congenital heart disease, enteral feed dependence, use of systemic steroids, age, and cumulative time for heliox use. The Youden index is a metric commonly used to determine an optional cut-point for a continuous variable by identifying the threshold that maximizes the sum of sensitivity and the specificity.13
All statistical analyses were performed using R, Version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). Graphs were plotted with Prism GraphPad (741) 9.3.1 (GraphPad Software, San Diego, California USA, www.graphpad.com).
3 RESULTS
3.1 Patient characteristics and hospitalization data
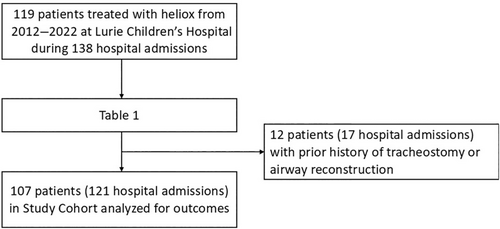
A total of 119 patients received heliox therapy during 138 hospital admissions (Figure 1). Table 1 summarizes patient characteristics and hospitalization data of the cohort. The patients, aged 12 (3, 31) months old, had medically complex backgrounds. Patients were born at a mean gestational age of 34.62 ± 5.82 weeks and had a mean 1-min APGAR score of 5.28 ± 2.97. Most (n = 100, 84%) patients had significant comorbidities such as enteral feed dependence (n = 87, 73.1%), a genetic or syndromic disorder (n = 43, 36.1%), hypotonia or a neuromuscular disorder (n = 63, 52.9%), and secondary airway lesions (n = 78, 65.6%). On average, patients spent a cumulative mean of 94 ± 187 h on heliox therapy per hospital admission. The most common indication for heliox was stridor due to upper airway obstruction (n = 89, 64%). Other indications included croup (n = 12, 10%), lower respiratory infection (n = 11, 9%), post-extubation stridor in patients with status epilepticus requiring intubation (n = 8, 7%), and status asthmaticus (n = 9, 8%). Additional medical treatments, such as systemic steroids, racemic epinephrine, and ciprofloxacin/dexamethasone nebulizers, were used in n = 132 (98%), n = 123 (89%) and n = 46 (33%) admissions, respectively. Eighty-five patients underwent surgical airway interventions (definitive and nondefinitive) during the same admission as heliox treatment.
| Patients, n (%) | 119 |
| Demographics, n (%) | |
| Gender | |
| Male | 71 (60) |
| Female | 48 (40) |
| Race | |
| Asian | 8 (7) |
| Black | 40 (34) |
| White | 43 (36) |
| Other | 28 (4) |
| Ethnicity | |
| Hispanic | 31 (26) |
| Birth history, Mean (SD) | |
| Gestational age (weeks) | 34.62 (5.82) |
| APGAR1 | 5.28 (2.97) |
| Indications for heliox use, n (%) | |
| Status asthmaticus | 9 (7) |
| Status epilepticus | 8 (6) |
| Croup | 12 (9) |
| Lower respiratory infection | 11 (8) |
| Post-LTR (pre-emptively) | 9 (7) |
| Upper airway obstruction | 89 (64) |
| Surgical interventions, any, n (%) | 85 (62) |
| Tracheostomy | 21 (15) |
| LTR | 14 (10) |
| Cricoid split | 8 (6) |
| Supraglottoplasty | 20 (14) |
| Epiglottopexy | 9 (7) |
| Balloon dilation | 25 (18) |
| Granulation or mass removal | 27 (20) |
| Adenotonsillectomy | 10 (7) |
| Palatal/tongue base surgery | 3 (2) |
- Abbreviations: LTR, laryngotracheal reconstruction; SD, standard deviation.
3.2 Patient outcomes following heliox treatment
Outcomes following heliox treatment were analyzed in 107 patients during 121 hospital admissions. Data from 17 hospitalizations, including 12 unique patients, were excluded because the patient had a history of definitive airway surgery prior to heliox initiation at current admission (Figure 1). Thirty-eight (35.5%) patients, representing 44 hospitalizations, underwent definitive airway intervention 12.26 ± 16.83 weeks following heliox treatment on average, at either their current hospital admission or a future hospitalization. An additional 13 (12.1%) patients were recommended definitive airway intervention but elected to forgo tracheostomy placement in preference of palliative care. During the 10-year follow-up, two patients (5.3%) who underwent airway surgical intervention passed away, compared with eight patients (61.5%) who elected palliative care.
3.3 Factors associated with the indication for the use of heliox
Eighty unique patients, representing 94 hospital admissions, received heliox for upper airway obstruction not related to croup, bronchiolitis, or asthma or related to croup, bronchiolitis, or asthma in the presence of known upper airway pathology. Twenty-seven patients, representing 35 admissions, received heliox for croup, bronchiolitis, or asthma (Table 2).
| Characteristic | Indications other than croup, bronchiolitis or asthma, or known upper airway pathology | Croup, bronchiolitis, or asthma | p-Value |
|---|---|---|---|
| Patients, n (%) | 80 (48) | 27 (52) | |
| Demographics | |||
| Gestational age, mean (SD) | 35.05 (5.30) | 37.13 (4.52) | 0.0707 |
| Comorbidities, n (%) | 74 (93) | 14 (52) | <0.0001* |
| GERD | 61 (76) | 7 (26) | |
| Enteral feed dependence (any) | 70 (88) | 0 (0) | |
| Genetic or syndromic disorder | 41 (51) | 2 (7) | |
| BPD/PH | 21 (26) | 3 (11) | |
| Asthma | 8 (10) | 12 (44) | |
| Neuromuscular disorder/hypotonia/DD | 58 (73) | 2 (7) | |
| Intracranial pathology | 46 (58) | 0 (0) | |
| Seizures | 35 (44) | 1 (4) | |
| Congenital heart disease | 28 (35) | 2 (7) | |
| Secondary airway lesions | 64 (80) | 1 (4) | |
| Subglottic stenosis | 39 (49) | 0 (0) | |
| Vocal cord immobility | 25 (31) | 0 (0) | |
| LM/TBM | 40 (50) | 0 (0) | |
| Hospital admissions, n (%) | 94 (78) | 27 (22) | |
| Stridor, n (%) | 85 (90) | 16 (59) | |
| Heliox use | |||
| Age at heliox (years), mean (SD) | 2.19 (3.63) | 4.00 (4.72) | 0.0409* |
| Cumulative time (h), mean (SD) | 120.4 (220.2) | 35 (43.40) | 0.0485* |
| Indications for heliox use, n (%) | |||
| Status asthmticus | 0 (0) | 9 (33) | |
| Post extubation stridor in patients with status epilepticus | 8 (9) | 0 (0) | |
| Respiratory infection in setting of upper airway lesions | 18 (19) | 0 (0) | |
| Upper airway obstruction not related to croup or asthma | 68 (72) | 0 (0) | |
| Hospitalization | |||
| Medical interventions, n (%) | |||
| Racemic epinephrine | 90 (100) | 18 (67) | 0.0002* |
| Systemic steroids | 89 (90) | 27 (100) | 0.6 |
| Ciprofloxacin-dexamethasone nebulizer | 33 (40) | 0 (0) | |
| Surgical interventions, n (%) | |||
| Airway reconstruction or tracheostomy | 59 (63) | 1 (4) | <0.0001* |
- Abbreviations: BPD/PH, bronchopulmonary dysplasia/pulmonary hypertension; LM/TBM, laryngomalacia/trachea-bronchomalacia; SD, standard deviation.
- *p < 0.05 indicates significance.
Most (n = 74, 93%) patients who received heliox for indications other than croup or asthma had other significant comorbidities, most commonly enteral feed dependence (n = 70, 88%), gastroesophageal reflux disease (n = 61, 76%), neuromuscular abnormalities (n = 58, 73%), genetic/syndromic disorders (n = 41, 51%) and history of seizures (n = 35, 44%). Common airway lesions in this group were subglottic stenosis (n = 39, 49%), vocal cord paralysis (n = 25, 31%) and laryngomalacia and/or tracheobronchomalcia (n = 40, 50%). The average age at time of heliox initiation was 2.2 ± 3.6 years. Indications for heliox in this population included stridor not related to infectious disease or asthma (n = 68, 72%), post-extubations stridor in patients with status epilepticus (n = 8, 9%), and respiratory infection in the setting of pre-existing airway lesion (n = 18, 19%).
Patients with croup or asthma without known airway pathology who required heliox during their admission presented at an older age than patients with other indications for heliox therapy (4.0 ± 4.7 vs. 2.2 ± 3.6 years, p = 0.04) and were significantly less likely to have background diseases (n = 14, 52% vs. n = 74, 93%, p < 0.0001). Particularly, none of the patients with croup or asthma were enteral feed-dependent or were diagnosed with intracranial neuropathology, compared with patients with other indications for heliox treatment. Congenital heart disease, neuromuscular disease, and genetic/syndromic disorder were uncommon in this cohort (n = 2, 7% each, respectively). The cumulative time spent receiving heliox was significantly higher in patients with other indications for heliox, who spent a mean of 120.4 ± 220.2 h receiving heliox, compared with a mean of 35 ± 43.4 h in patients with croup or asthma, p = 0.048 (Figure 2). Patients treated with heliox for indications other than croup or asthma were significantly more likely to require re-intubation following heliox discontinuation (n = 43 [46%] vs. n = 1 (4%), p < 0.0001), and definitive airway intervention (n = 59 [63%] vs. n = 1 [4%], p < 0.0001), compared with patients treated for croup or asthma. Racemic epinephrine was less commonly used in patients with croup or asthma (n = 18, 67% vs. n = 90, 100%, p = 0.0002), whereas steroids were similarly used by both groups. Of the patients treated for croup or asthma, 14 patients (52%) required heliox for more than 24 h, three (11%) of whom received heliox for more than 47 h. Neither one of these patients required a tracheostomy nor other definitive airway surgery. The patient who was recommended a tracheostomy had an upper airway infection complicated by pneumonia and pulmonary hemorrhage and subsequently passed away.
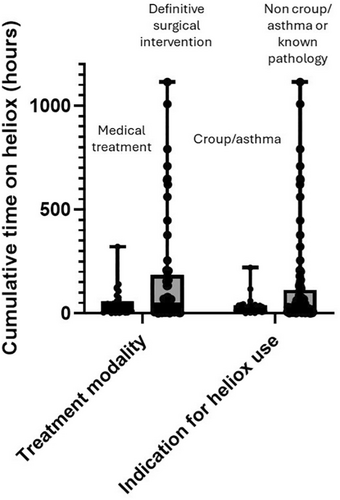
3.4 Factors associated with the need for definitive airway surgery
Table 3 summarizes patient characteristics and hospitalization data by need for definitive airway surgical intervention. Patients who were recommended definitive airway intervention but opted for palliative care were categorized with patients who underwent definitive airway intervention. Fifty-one (48%) patients, representing 60 (50%) hospital admissions, required LTR, cricoid split or tracheostomy tube placement. Patients who required definitive airway surgery were more likely to have other, non-definitive, airway surgical interventions prior to pursuing definitive care (43 [64.2%], vs. 24 [35.8%], p = 0.0005). On univariate analysis, the need for definitive airway intervention was associated with the presence of secondary airway lesions (n = 47, 92% vs. n = 19, 34%, p < 0.0001), neuromuscular disorder (n = 42, 83% vs. n = 18, 32%, p < 0.0001), intracranial neuropathology (n = 35, 68% vs. n = 11, 20%, p < 0.0001), a genetic or syndromic disorder (n = 30, 59% vs. n = 13, 23%, p < 0.0001), and enteral feed dependence (n = 48, 94% vs. n = 29, 52%, p < 0.0001). In contrast, the prevalence of asthma was significantly higher in patients who did not require surgical interventions (16 [29%] vs. 4 [8%], p = 0.0009). Figure 2 depicts the cumulative time spent receiving heliox in patients by a need for definitive airway surgical intervention. Patients who required tracheostomy or airway reconstruction received a mean of 160 ± 265.1 h on heliox therapy compared with a mean of 35 ± 32 h in those who did not (p = 0.0004). Length of hospital stay, from heliox initiation to either discharge or definitive surgical intervention, was significantly higher in those who required definitive airway intervention (93 ± 90 days vs. 8.95 ± 11.1 days, p < 0.0001).
| Characteristic | Definitive airway surgery | No definitive airway surgery | p-Value |
|---|---|---|---|
| Patients, n (%) | 51 (48) | 56 (52) | |
| Comorbidities, n (%) | 50 (98) | 38 (68) | <0.0001* |
| Gastroesophageal reflux | 45 (88) | 22 (39) | |
| Enteral feed dependence (any) | 48 (94) | 29 (52) | |
| Genetic or syndromic disorder | 30 (59) | 13 (23) | |
| BPD/PH | 13 (25) | 11 (0.20) | |
| Asthma | 4 (8) | 16 (29) | |
| Neuromuscular disorder | 42 (82) | 18 (32) | |
| Intracranial pathology | 35 (68) | 11 (20) | |
| Congenital heart disease | 20 (39) | 10 (18) | |
| Secondary airway lesions | 47 (92) | 19 (34) | <0.0001* |
| Subglottic stenosis | 31 (61) | 9 (16) | <0.0001* |
| Vocal cord immobility | 24 (47) | 1 (2) | <0.0001* |
| LM/TBM | 31 (61) | 9 (16) | <0.0001* |
| Hospital admissions, n (%) | 60 (50) | 61 (50) | |
| Heliox use | |||
| Age at heliox (years), median (IQR) | 7 (2, 29) | 15 (7, 33.5) | 0.07 |
| Cumulative time (h), mean (SD) | 160.4 (265.1) | 35 (32.40) | 0.0005* |
| Cumulative time (h), median (IQR) | 36 (11, 160) | 28 (11, 160) | |
| Re-intubated after heliox, n (%) | 37 (62) | 7 (12) | 0.0003* |
| Indications for heliox use, n (%) | |||
| Status asthmaticus | 0 (0) | 9 (15) | 0.0028* |
| Status epilepticus | 3 (5) | 5 (8) | 0.7 |
| Respiratory infection (any) | 16 (27) | 25 (41) | 0.12 |
| Upper airway obstruction | 41 (68) | 22 (36) | 0.0005* |
| Hospitalization | |||
| Length of stay (days), mean (SD) | 93 (90.0) | 8.95 (11.10) | <0.0001* |
| Medical interventions, n (%) | |||
| Racemic epinephrine | 59 (1.0) | 49 (80) | 0.0025* |
| Systemic steroids | 56 (9) | 60 (98) | 0.21 |
- Abbreviations: BPD/PH, bronchopulmonary dysplasia/pulmonary hypertension; LM/TBM, laryngomalacia/trachea-bronchomalacia; SD, standard deviation.
- *p < 0.05 indicates significance.
In multivariable regression analysis, neuromuscular disease, intracranial neuropathology, and cumulative time of heliox were associated with a need for tracheostomy or airway reconstruction. Age at the time of heliox initiation and bronchopulmonary dysplasia were not identified as risk factors associated with needing a definitive airway intervention. The presence of neuromuscular disease and intracranial neuropathology were associated with higher odds of requiring definitive airway surgery (OR, 4.63 [95% CI 1.16–21.2, p = 0.035] and OR, 6.76; 95% CI 1.27–54.5, p = 0.033), respectively. Using the Youden method, an optimal threshold of 47 h (sensitivity 0.52, specificity 0.84) receiving heliox was identified (Figure 3). Need for heliox greater than 47 h was associated with a 6.2-fold increased risk of requiring definitive airway intervention (95% CI 2.56–14.13, p < 0.0001), whereas heliox dependence for more than 5 days had a specificity of 0.98 and positive predictive value of 0.94 in predicting a need for definitive airway intervention.

3.5 Patients with upper airway obstruction not related to croup, bronchiolitis, or asthma
Sub-analysis of the group of patients who received heliox for indications other than croup, bronchiolitis, or asthma and required definitive airway intervention (n = 50) compared with medical treatment (n = 30) revealed that although demographic data were similar between the groups, comorbidities and the presence of other airway lesions were significantly more common among patients who required definitive airway intervention (n = 50, 100% vs. n = 26, 87%, p = 0.02 and n = 47, 94% vs. n = 17, 57%, p<0.0001, respectively). Patients who did not require definitive airway intervention were more likely to present with croup or asthma in the setting of secondary airway lesion than other indications for heliox, like post extubations or congenital stridor. The average time on heliox was significantly higher in patients who required definitive surgical intervention (164.5 ± 266.2 h vs. 47.4 ± 60.2, p = 0.01).
4 DISCUSSION
Helium–oxygen gas mixtures are given to children with a variety of upper and lower airway disorders with the aim of decreasing the work of breathing, improving stridor, and temporizing the airway to prevent intubation. Helium is an inert gas with no intrinsic bronchodilatory or anti-inflammatory properties.1 Rather, the low density of helium is the basis for its potential therapeutic benefit. In airways with increased airflow turbulence or resistance, a greater driving pressure and, therefore, work of breathing is required to sustain steady airflow.2, 3 The low density of helium may change airflow from turbulent to a more efficient laminar flow and increase airflow even under turbulent conditions.1
Our study demonstrates that heliox is an uncommon measure to address upper airway obstruction in children. Nevertheless, despite the lack of evidence-based data, the most common indication for heliox use was non-croup/asthma upper airway obstruction. Patients treated with heliox for croup or asthma did not require definitive airway intervention, even in the setting of prolonged heliox use, if they did not have pre-existing upper airway lesions. In patients with other indications for heliox treatment or in patients with croup or asthma and pre-existing upper airway lesions, multivariable regression analysis identified neuromuscular disease, intracranial neuropathology, and cumulative time receiving heliox as being associated with a need for tracheostomy or airway reconstruction. Specifically, cumulative use of heliox over 47 h was associated with 6.2-fold higher odds of needing airway reconstruction or tracheostomy. Ninety-seven percent of patients who received heliox for more than 5 days during the same admission required definitive airway surgery.
Several studies have demonstrated the benefit of heliox in clinical applications, such as children with asthma exacerbations or lower airway infection. Kudukis et al.4 enrolled 18 children with status asthmaticus in a double-blind, randomized, controlled trial and found that heliox use significantly increased peak flow and lessened the dyspnea index. In another randomized controlled trial of 30 children presenting to the emergency department with asthma exacerbation, heliox therapy was associated with a greater degree of clinical improvement.5 Randomized, controlled trials evaluating the utility of heliox in children with bronchiolitis or croup have also demonstrated possible benefits in a few small cohorts and in a recent Cochrane review.6-9 Most of these studies did not elaborate on the patient's background diseases or excluded patients with significant comorbidities.
Less evidence exists for the use of heliox in children with upper airway obstruction secondary to etiologies other than croup or asthma. Patients with a reversible etiology for upper airway obstruction, like laryngeal edema secondary to prolonged intubation, trauma, or reflux, or patients with acute-on chronic airway obstruction like upper airway infection in patients with low-grade subglottic stenosis or vocal cords paralysis, pose a special challenge. These patients often present with increased work of breathing that may escalate to a need for intubation, which, in turn, may further increase the level of airway edema. Heliox, theoretically, may be used to buy time and bridge this period, preventing increased breathing work and additional trauma from the turbulent airflow to the already inflamed and edematous airway. In a randomized, controlled trial of 15 pediatric patients with post-extubation stridor by Kemper et al.,4 stridor scores were lower in patients treated with heliox than oxygen. In Grosz et al.3 retrospective cohort study of 42 children with upper airway obstruction, 72.7% of the patients had decreased work of breathing after heliox treatment. Similar to our findings, patients with croup were more likely to respond to heliox treatment compared with patients with other causes of respiratory compromise, such as subglottic stenosis or edema. Few other case series and case reports14-16 evaluated the overall effect of heliox on post-extubation stridor and work of breathing and reported immediate relief and decrease in respiratory distress. The length of heliox treatment and overall effect beyond the immediate time period were not discussed in detail. In a prospective study evaluating patterns of heliox usage in children and adults in the ICU, Berkenbosch et al.17 described their experience with 27 children with upper airway obstruction who were treated with heliox for 17.6 h on average. Heliox was considered of no benefit in five children, and three patients required tracheostomy or intubation. The mean length of heliox treatment prior to airway manipulation was only 2.9 h on average; however, no further data were given on these patients.
Although heliox does not have any known direct adverse effects, overutilization of heliox is associated with high costs, prolonged admission in the ICU, significant respiratory therapy staffing needs, and may delay the definitive care for the patient. Our study demonstrates that patients who were recommended a tracheostomy or LTR spent a significantly longer amount of time receiving heliox therapy prior to the decision on appropriate treatment. This suggests that continuing heliox in preference of pursuing other treatment options may significantly delay the definitive care that is needed. Therefore, early identification of patients who will likely require definitive airway intervention is of utmost importance. Our data suggest that a need for heliox for 47 h is associated with a higher likelihood of needing surgical intervention. Other risk factors that should be considered are neuromuscular disease and known neuropathology. Almost all the children who required heliox for more than 5 days during the same admission required definitive airway intervention. Furthermore, randomized, prospective studies are required to analyze the full effect of heliox on patients with upper airway edema and other comorbidities and identify risk factors associated with a need for definitive airway interventions.
Our study has a few limitations that should be considered when interpreting the results. First, our study is retrospective in nature without control groups. The study cohort is relatively small and heterogenic, which limits generalizability. We did not investigate clinical outcomes such as reduction in stridor or work of breathing, tachypnea reduction, or vital sign stability, which could provide further insight into the immediate clinical utility of heliox in relieving obstructive symptoms. Due to lack of guidelines or consensus, the decision to initiate or terminate heliox treatment was at the discretion of the clinician and was not standardized, which may affect the generalizability of our results to other institutions. Similarly, the subjective decision regarding heliox treatment, the retrospective nature of this study, and the heterogenicity of our cohort may limit the precision of our data. Hence, the interpretation of the Youden Index may not be generalized to other institutions. Finally, we categorized patients who were recommended definitive airway surgery but pursued palliative care with patients who received definitive airway care, which may affect the validity of our results. Nonetheless, to the best of our knowledge, this hypothesis-generating study is the first to evaluate the end-point outcomes of cumulative heliox usage in children with respiratory compromise. Larger, multi-institutional prospective studies are needed to obtain high-level data required to establish a consensus regarding the use of heliox in children with upper airway obstruction not related to croup or asthma.
5 CONCLUSIONS
Heliox may be used as a temporizing agent in children with respiratory compromise and upper airway obstruction. Variables associated with the need for definitive airway intervention include complex comorbidities, intracranial neuropathology, and neuromuscular disorders. The effectiveness of heliox use for more than 47 h in children, especially if other comorbidities are present, should be reconsidered.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.