Kids are not just small adults: An attempt to validate pediatric tablet-based digits in noise testing
This article was presented as a poster at the ASPO meeting in 2023.
Abstract
Objective
The objective of this study is to investigate whether conductive hearing loss (CHL) can be differentiated from sensorineural hearing loss in children ages 3–18 using a diotic and antiphasic digits-in-noise (DIN) tablet-based test using existing adult cut-off criteria.
Methods
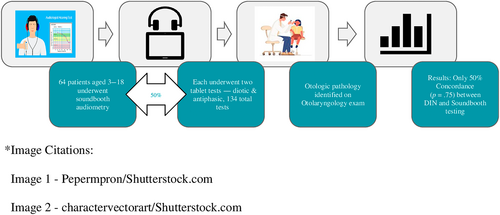
A blinded multi-institutional prospective cohort of 64 children aged 3–18 scheduled for an audiometric soundbooth evaluation with a pediatric audiologist and a same-day otolaryngologist examination were recruited for the study. Following a conventional audiogram, the subjects underwent diotic (same-phased stimuli) and antiphasic (out-of-phase stimuli) DIN testing on a HearX Samsung Galaxy tablet with over-the-ear headphones, for a total of 128 measurements. DIN test results were compared with soundbooth audiometry using known adult “cut off criteria.”
Results
A logistic regression analysis adjusted for demographics (age, sex) and race was performed to compare CHL determination from DIN testing to CHL determination with soundbooth audiometry. The results showed 50% agreement with a p-value of .753. The determinations based on combined DIN testing agreed with each other 33% of the time and had a p-value of .373. Otologic pathology and age were not predictive of outcome.
Conclusion
This preliminary analysis of DIN testing indicated that DIN and audiometric testing completed in a soundbooth were not significantly predictive of one another in the population of children aged 3–18 when using the adult cut-off criteria for CHL differentiation. Given these findings, further testing is required in children to determine pediatric specific cut-off values.
1 INTRODUCTION
Hearing loss is the fourth leading cause of global disability, affecting over 466 million individuals, of which over 32 million are children.1, 2 Childhood hearing loss is associated with speech and language delays, lower literacy, higher likelihood of school dropout, lower educational attainment and decreased employment opportunities.3, 4 Furthermore, the World Health Organization suggests that roughly 60% of childhood hearing loss is preventable, with much of this from chronic serous middle ear effusions causing conductive hearing loss (CHL).5 For children without regular health care access, school-based hearing screening is a critical component of identifying and facilitating treatment of pediatric hearing loss.6 Unfortunately, there has been a lack of standardization in school-based hearing programs, a lack of technological innovation over the past several decades, and a high loss to follow-up rate after referral.7
Recent technological advancements have made audiometric testing equipment more accessible,8 portable,9 and easier to use in low-resourced settings,10 particularly in the absence of a trained audiologist or otolaryngologist.11 Portable smartphone and tablet audiometers have been shown to achieve similar results to conventional audiometry but without the physical limitation of a soundbooth, making this technology a feasible and easily accessible means to collect data.12-14
Although smartphone technology has greatly enhanced the information available to hearing specialists, it lacks the critical ability to discern CHL from sensorineural hearing loss (SNHL).13, 15 This information allows a provider to understand whether a hearing aid (or other amplification) may be necessary or whether the candidate has a potentially treatable cause of hearing loss (cerumen impaction, otitis media, cholesteatoma, etc.) that necessitates intervention prior to considering amplification. Obtaining this information up front can facilitate appropriate triage of patients, especially in a population-based setting such as school-based screening.14 Currently, school-based hearing screening is limited to basic pure tone screening due to a lack of technologic innovation in this area. Subsequently, follow-up rates for pediatric school-based screening referral are poor, a multi-factorial weakness, but at least partially due to the limited information that can be utilized from the referral itself.6
Recently, a new smartphone-based audiometric test has been developed that can discern CHL from SNHL without the use of a soundbooth or a bone transducer.16 A digits-in-noise (DIN) test, which can be administered via smartphone using standard over-the-ear (or insert) headphones, requires the patient to accurately recognize 50% of spoken digit triplets in the presence of speech-weighted masking noise. Two variations of the DIN test, diotic and antiphastic DIN have been shown to differentiate CHL from SNHL.16 In theory, patients with cochlear damage have lower frequency selectivity, and therefore a worse ability to differentiate complex sounds such as speech in noise, when compared with patients with normal hearing or CHL. Adult data suggest that utilization of diotic DIN and pure tone average audiometry can detect CHL at a 97.2% sensitivity and 93.4% specificity in adults.16, 17 A limited number of studies have explored DIN testing in normal-hearing children, supporting its potential use as a screening tool in the pediatric population.18 Furthermore, these tests can be conducted using a smartphone, without the need of a soundbooth, bone transducer or specially trained personnel. Although this concept has been validated in adults and in children with normal hearing, no studies have analyzed this as a pediatric screening tool to differentiate CHL from SNHL. This study evaluates tablet-based DIN testing as a means to differentiate CHL from SNHL in a pediatric population when compared with the gold standard, soundbooth audiometry.
2 METHODS
2.1 Study design
This is a blinded, prospective cohort study of children with hearing loss at Children's Minnesota and the M Health Fairview Masonic Children's Hospital Lions Children's Hearing and ENT Clinic. IRB approval was obtained from both institutions.
2.2 Setting and participants
A prospective cohort of children aged 3–18 scheduled for an audiometric soundbooth evaluation with an audiologist and a same-day otolaryngology evaluation were eligible for the study. Participants were identified at Children's Minnesota or the M Health Fairview Masonic Children's Hospital Lions Children's Hearing and ENT Clinic. Those with CHL, SNHL or normal hearing were eligible to participate. Otologic pathology included normal tympanic membrane, cerumen impaction, tympanic membrane perforation, middle ear effusion/otitis media, otorrhea/otitis externa, cholesteatoma, and/or “other.”
2.3 Inclusion criteria
All children with existing appointments for both soundbooth audiometry and otolaryngology at Children's Minnesota or the M Health Fairview Masonic Children's Hospital Lions Children's Hearing and ENT Clinic were eligible for the study. Children with only an audiometric appointment or only an otolaryngology appointment on that day were not eligible. Children needed to be able to repeat the numbers 1–10 in English. Children who had a difficult time understanding the test were included given that the inability to complete the test is a study outcome. Children were included regardless of their native language or otologic pathology.
2.4 Exclusion criteria
Patients who were unable to participate in traditional soundbooth audiometry or diotic DIN testing due to behavioral issues were excluded from the study. This was determined by confirming with the audiologist if a child was able to participate in behavioral soundbooth audiometry. Children in whom an ear examination was not reliable (such not allowing ear-level examination) were also excluded from the study.
2.5 Eligibility and screening
Prior to the appointment, pre-screening eligibility was determined by the researcher using the electronic health record (EHR) to ensure the patient met the inclusion and exclusion criteria. Recruitment and screening involved providing a description of the study, stating risks and benefits and asking guardians of eligible patients if they were interested in participating. The researcher also discussed risks and benefits and answered any questions regarding the study and participation. Consent was obtained from guardians and eligible patients via an electronic signature in the secure REDcap database on a Samsung Galaxy tablet immediately prior to the clinic appointment. An assent form was reviewed and an electronic signature was obtained from all participants 7 years of age and older. As this was a minimal risk study, only one parent was required to consent.
2.6 Technology and equipment
All DIN tests were conducted via a Samsung Galaxy tablet with ISO-calibrated noise-canceling Sennheiser HD280 Circumaural over-the-ear headphones. HearX provided technical support as needed. REDCap database was used for data collection.
2.7 Testing and study procedures
Following the conventional audiogram, 64 subjects underwent diotic (same-phased stimuli) and antiphasic (out-of-phase stimuli) DIN testing on a Samsung Galaxy tablet with over-the-ear headphones, for a total of 128 measurements (Figure 1). The testing took approximately 15 min in total, with 5 min for demographic data collection, 5 min for the diotic set and 5 min for the antiphasic set. The test used an adaptive one-up, one-down test procedure. Stimuli are binaurally same phased (diotic) and digits were presented with speech weighted masking noise to determine the signal to noise ratio (SNR) at which 50% of digit triplets (i.e., 2, 4, 7) could be recognized correctly and the speech reception threshold (SRT), determined by averaging the SNR of the last 19 of 23 digit triplets. Following the soundbooth and DIN testing, the audiologist and tester were asked to complete a short form rating their perceived reliability of the test as good, fair, or poor.
Upon completion of the protocol, the patient was able to immediately proceed with their scheduled physician appointment. Per standard of care, the child was treated for their soundbooth audiometric findings by their otolaryngologist at this scheduled appointment. Per clinic protocol, if the audiologist identified impacted cerumen to be influencing the patient's hearing, this was removed prior to further audiometric testing. The audiologist and otolaryngologist were blinded to the diotic and antiphasic DIN results.
2.8 Audiometric theory
Hearing loss due to cochlear or nerve damage (SNHL) has lower frequency selectivity, which influences the ability to detect complex sounds such as digits played in the presence of background noise.16 Therefore, a patient with SNHL is expected to perform worse on a DIN test than a patient with CHL. Patients with unilateral CHL or SNHL hearing loss are expected to perform well on a diotic DIN test because their performance will reflect the better hearing ear. Patients with a CHL can more accurately differentiate DIN compared with patients with SNHL due to their better frequency selectivity compared with patients with SNHL as most digits are presented at suprathreshold intensities. Therefore, patients with CHL are also expected to perform well on diotic DIN testing. The antiphasic DIN tests play phase-inverted digits with interaural in-phase masking noise, which reduces the ability of the brain to use binaural integration as a tool to decipher the digits in the presence of background noise. The 180 degree phase shift in the antiphasic DIN simulates interaural timing differences which are easily interpreted by the brain as spatial cues and differentiated into digits from noise. However, if one ear is not hearing well, or if there is CHL, the binaural integration is not possible and the brain cannot decipher these digits as well through the background masking noise. Therefore, patients with unilateral SNHL or CHL are expected to perform worse on antiphasic DIN testing.17
Adult data suggest that patients with normal hearing will perform better on both diotic and antiphasic DIN testing. Patients with bilateral SNHL will perform poorly on both diotic and antiphasic DIN testing.16, 17 Patients with unilateral SNHL or CHL will perform better on diotic DIN testing but poorly on antiphasic DIN testing. Specific adult algorithmic SNR cutoffs for this testing are proprietary to HearX but this concept has been validated in adults with 79% accuracy in differentiating among normal hearing, CHL or unilateral SNHL, and bilateral SNHL.
To differentiate CHL from SNHL, pure tone averages were evaluated. A patient with CHL will have a normal or near-normal SRT on diotic DIN testing; however, they will have elevated pure tone averages due to their hearing loss. A patient with SNHL hearing loss will have lower SRT on diotic DIN testing and elevated pure tone averages. A normal hearing individual will have normal SRT on diotic DIN and normal pure tone averages.
2.9 Data collection
The diotic and antiphasic DIN results were uploaded via the cloud to the M Health studio (HIPAA compliant cloud server run by HearX). The raw data from the DIN and antiphasic test were interpreted by HearX to determine if CHL versus SNHL was present using HearX's proprietary algorithm. The HearX algorithm can differentiate hearing loss into the following categories: normal hearing, CHL/unilateral SNHL, and bilateral SNHL.
Demographic data was collected from EHR via chart review including patient age, native language and sex. Audiometric data was obtained from the audiology note in the EHR. This included pure tone average, severity of hearing loss, air-bone gap if CHL, and tympanometry. As an internal quality metric, the person performing the test answered a single question asking: “Do you feel the child understood and completed the task adequately?” The presence of otoscopic pathology including cerumen impaction, otitis media, and perforation was determined from the otolaryngologist note in the EHR.
The primary outcome of interest was hearing loss, specifically conductive or sensorineural. Raw audiometric data including pure tone averages, air bone gap, and severity of hearing loss was analyzed. Severity of hearing loss was graded using the World Health Organization grading metric.19 The raw data from the diotic and antiphasic DIN test was abstracted including SRT in addition to a yes/no determination of hearing loss. Similar to prior studies on this topic, mixed hearing loss was categorized as SNHL.16, 17 DIN test results were compared with soundbooth audiometry with the primary outcome being the differentiation of CHL from SNHL.
Logistic regression was used to evaluate the association of various parameters with the ability of diotic and antiphasic DIN to accurately distinguish CHL from SNHL. These parameters included age, sex, language, otoscopic pathology (normal tympanic membrane, cerumen impaction, tympanic membrane perforation, effusion/otitis media, otorrhea/otitis externa, cholesteatoma, and/or “other”), and the researcher's perception of the child accurately completing the test. Significance was assessed using an α = .05. Tukey Honest Significant Difference test and Ducan Multiple Range Testing was used to compare diotic and antiphasic DIN SRT to soundbooth audiometry findings.
3 RESULTS
Sixty-four children aged 3–18 underwent soundbooth audiometry and DIN testing. The average age was 8.49 years (range: 3.1–17.1; standard deviation [SD] 3.7). Most subjects were female (59%, n = 38) and white (78.1%, n = 50). Most subjects spoke English as their native language (90.9%, n = 60). Further demographics are described in Table 1.
| Age (years) | |
| Average | 8.5 |
| Range | 3.1–17.1 |
| Standard deviation | 3.7 |
| Sex | |
| Male | 59% (n = 38) |
| Female | 41% (n = 26) |
| Ethnicity | |
| White | 78.1% (n = 50) |
| Black | 4.7% (n = 3) |
| Asian | 4.7% (n = 3) |
| Hispanic | 10.9% (n = 7) |
| Other | 7.8% (n = 5) |
| Native language | |
| English | 90.9% (n = 60) |
| Spanish | 6.1% (n = 4) |
The majority (96.9%, n = 62) of soundbooth testing was deemed to have “good” reliability by the audiologist performing the testing. Most patients (59.4%, n = 38) had normal hearing, whereas 35.9% (n = 23) had unilateral SNHL or CHL, and 4.6% (n = 3) had bilateral SNHL. Most ears had a Type A tympanogram (67.0%, n = 73) on tympanometry. Additional results are described in Table 2a.
| Soundbooth audiometry | |
|---|---|
| Reliability of soundbooth audio | |
| Good | 96.9% (n = 62) |
| Fair | 3.1% (n = 2) |
| Poor | 0.0% (n = 0) |
| Hearing loss (soundbooth audio) | |
| Normal | 48.4% (n = 31) |
| Unilateral SNHL/CHL | 42.2% (n = 27) |
| SNHL | 9.4% (n = 6) |
| Conductive hearing loss only | |
| Yes | 51.6% (n = 33) |
| Average Air Bone Gap (dB) | 27.2 |
| Tympanometry | |
| Type A | 67.0% (n = 73) |
| Type B | 23.9% (n = 26) |
| Type C | 9.2% (n = 10) |
| Otologic pathology | |
| Normal tympanic membrane | 49.2% (n = 63) |
| Cerumen impaction | 17.2% (n = 22) |
| Tympanic membrane perforation | 6.3% (n = 8) |
| Effusion | 3.1% (n = 4) |
| Otitis media | 0.0% (n = 0) |
| Otorrhea otitis externa | 2.3% (n = 3) |
| Cholesteatoma | 0.0% (n = 0) |
| Patent ear tube | 16.4% (n = 21) |
| Othera | 21.1% (n = 27) |
- Abbreviations: CHL, conductive hearing loss; SNHL, sensorineural hearing loss.
- a “Other” includes myringosclerosis, history of cartilage-backed tympanoplasty, dried blood and debris in external auditory canal, retraction of tympanic membrane, etc.
Regarding the DIN testing, 65.6% (n = 42) of cases were deemed to have “good” reliability by the tester, 36.5% (n = 17) were deemed to have “fair” reliability and 7.8% (n = 5) were deemed to have “poor” reliability. Age was correlated with reliability, as the average age of patients with DIN testing with “good” reliability was 9.9 years of age (SD 3.5 years), that of patients with “fair” reliability was 6.3 years of age (SD 2.17), and that of patients with “poor” reliability was 3.56 (SD 0.36 years) (p < .05).
The otologic pathology identified during the otolaryngology examination included normal tympanic membrane (n = 32 right ear, n = 31 left ear), cerumen impaction (n = 10 right ear, n = 12 left ear), tympanic membrane perforation (n = 4 right ear, n = 4 left ear), effusion/otitis media (n = 2 right ear, n = 2 left ear), otorrhea/otitis externa (n = 2 right ear, n = 1 left ear), cholesteatoma (n = 0 right ear, n = 0 left ear), patent ear tube (n = 11 right ear, n = 10 left ear), and “other” (n = 12 right ear, n = 15 left ear) (Table 1). “Other” included, for example, myringosclerosis, history of cartilage-backed tympanoplasty, dried blood and debris in external auditory canal, retraction of tympanic membrane, etc.
The mean duration of diotic DIN testing was 227 s (SD 111 s), whereas the average duration of antiphasic DIN testing was 189.2 s (SD 76.8). The mean response time for diotic DIN was 6.4 s and the mean response time for antiphasic DIN testing was 4.8 s. Seventeen (36.9%) “normal” results were produced with the diotic DIN test with an average SRT of −3.43 and 24 (37.5%) “normal” results were produced with the antiphasic DIN test with an average SRT of −7.37 (Table 2b).
| Reliability of DIN | |
| Good | 65.6% (n = 42) |
| Fair | 26.6% (n = 17) |
| Poor | 7.8% (n = 5) |
| Diotic DIN | |
| Duration (s) | 227 |
| SD of duration (s) | 111 |
| Mean response time (s) | 6.4 |
| Normal | 36.9% (n = 17) |
| Reduced | 73.4% (n = 47) |
| Average SRT | −3.43 |
| Antiphasic DIN | |
| Duration (s) | 189.2 |
| SD of duration (s) | 76.8 |
| Mean response time (s) | 4.8 |
| Normal | 37.5% (n = 24) |
| Reduced | 62.5% (n = 40) |
| Average SRT | −7.37 |
- Abbreviations: SD, standard deviation; SRT, speech reception threshold.
The SRT of both diotic and antiphasic DIN is described for each patient with normal hearing, unilateral SNHL or CHL, and bilateral SNHL in Table 3a. The SRT of the diotic (p = .24) and antiphasic (p = .15) DIN test does not correlate with the soundbooth audiometry findings. When the tests which were deemed to have “fair” or “poor” reliability by the DIN tester were excluded (Table 3b), the results similarly did not correlate with soundbooth audiometry findings (diotic: p = .27 and antiphasic: p = .12).
| Normal (n = 38) | Unilateral SNHL/CHL (n = 23) | Bilateral SNHL (n = 3) | |
|---|---|---|---|
| Diotic DIN | |||
| Duration (s) | 215 | 258 | 147 |
| Mean response time (s) | 5919 | 770 | 2957 |
| SD of response time (s) | 13,408 | 17,603 | 6818 |
| Normal | 12 | 5 | 0 |
| Reduced | 26 | 17 | 3 |
| SRT | −5.29 | 0.21 | −7.87 |
| Antiphasic DIN | |||
| Duration (s) | 189 | 196 | 130 |
| Mean response time (s) | 4772 | 5094 | 2200 |
| SD of response time (s) | 10,240 | 11,712 | 4869 |
| Normal | 21 | 1 | 2 |
| Reduced | 17 | 20 | 1 |
| SRT | −9.55 | −2.76 | −13.67 |
- Abbreviations: CHL, conductive hearing loss; SD, standard deviation; SNHL, sensorineural hearing loss; SRT, speech reception threshold.
| Normal (n = 26) | Unilateral SNHL/CHL (n = 13) | Bilateral SNHL (n = 3) | |
|---|---|---|---|
| Diotic DIN | |||
| Duration (s) | 179 | 188 | 147 |
| Mean response time (s) | 4325 | 4723 | 2957 |
| SD of response time (s) | 9690 | 10,777 | 6818 |
| Normal | 11 | 5 | 0 |
| Reduced | 15 | 8 | 3 |
| SRT | −9.37 | −7.6 | −7.87 |
| Antiphasic DIN | |||
| Duration (s) | 161 | 178 | 130 |
| Mean response time (s) | 3554 | 4289 | 2200 |
| SD of response time (s) | 7537 | 9171 | 4869 |
| Normal | 21 | 1 | 2 |
| Reduced | 5 | 12 | 1 |
| SRT | −15.09 | −9.78 | −13.67 |
- Abbreviations: CHL, conductive hearing loss; SD, standard deviation; SNHL, sensorineural hearing loss; SRT, speech reception threshold.
A logistic regression analysis adjusted for age, sex, and race was performed to compare CHL determination from DIN testing using pure-tone audiometry and diotic DIN to CHL determination with soundbooth audiometry. Results showed 50% agreement with a p-value of .753. The determination based on combined DINs agreed with each other 33% of the time and had a p-value of .373. This indicates that DIN and soundbooth testing were not significantly predictive of one another in the population of children aged 3–18.
4 DISCUSSION
Despite promising findings in adults, DIN testing did not differentiate CHL from SNHL in our pediatric population. The concordance rates of 50% or 33%, based on which method was used are not an acceptable screening standard for hearing loss.
There are many possible explanations for this discordance. First, pediatric audiometric testing is fundamentally different from adult testing. The nuances of a growing pediatric ear, including one that is inherently more prone to transient CHL from fluid, may not behave consistently enough for the frequency selectivity hypothesis that is required for CHL to be differentiated from SNHL using DIN. Perhaps longer term cochlear damage can be perceived by the test but shorter term cochlear damage cannot. The reason for this discrepancy may be much simpler. Children have limited attention spans and conditioning a child to perform the test may be a challenge. The decision to include children who may not have understood the test may have also contributed to the lack of concordance in findings. However, the inability to complete the test is a valuable study outcome because it improves our understanding of how our test performs across various age ranges and native language differences.
To further understand this result, a larger sample size with a greater range of patient ages is necessary. Testing more older children can help determine whether this is an age-dependent failure—a limitation of this study due to sample size. A greater range of ages will offer insight into whether or not age can serve as a predictor of DIN and Antiphasic SRTs, as seen in the population of children with normal hearing.18 Of course, with a larger sample size, one could potentially determine a new pediatric-specific SNR cut-off criterion.
Traditionally, otolaryngologists and audiologists have utilized a myriad of different tools to distinguish CHL from SNHL (tuning fork evaluation, microscopic evaluation of the tympanic membrane, etc.) but the gold standard remains masked soundbooth audiometry with a bone transducer. Although a bone transducer is available through one iPad-based audiometer (Shoebox Professional, Ottawa, ON, Canada), masking is only available in the advanced testing mode and therefore is not currently a feasible tool for screening by a user without an audiology background to utilize without a soundbooth.
With further study, if DIN testing is found to be reproducible in the pediatric population, this test could have profound implications for screening children. Since this test can be run without formal audiometric equipment and without formal audiology training, it could have high utility in the community for school-based screening. The ability to differentiate CHL from SNHL at the point of a failed community or school-based hearing screen could potentially help triage the patient to the appropriate referrals (i.e., audiology/otolaryngologist), thus reducing the burden on our health care system, particularly primary care, by making referrals more efficient. It is important to note that even in the adult population, where this test has been found to be reliable, a formal audiometric evaluation remains important for diagnostic testing. At this point, unfortunately, pediatric DIN testing is not reliable enough to accomplish these goals.
Strengths of this study include the blinded prospective cohort study design with a comparator arm that involved the gold standard audiometric testing of behavioral audiometry conducted by an audiologist in a soundbooth on the same day as the tablet testing. Major limitations include the small sample size and lack of diversity in the study population (78% white).
5 CONCLUSION AND FUTURE DIRECTIONS
This preliminary analysis of DIN testing, regardless of methodology, indicated that DIN and soundbooth were not significantly predictive of one another in our population of children aged 3–18 when using the adult cut-off criteria for CHL differentiation. Given these findings, further testing in a large population of children is needed to determine a new cut-off value for the development of a reliable and valid pediatric specific algorithm.
ACKNOWLEDGMENTS
The authors would like to thank Children's Minnesota IRGP and UMN Foundation for grant funding.