Introduction of universal transvaginal cervical length measurement does not decrease spontaneous preterm delivery rate compared to universal transabdominal screening with reflex cut-off: A pre-post study
Abstract
Objectives
The objective of our study is to examine cervical length measurements, identification of short cervix, vaginal progesterone use, and rate of spontaneous preterm delivery before and after departmental transition to a universal transvaginal ultrasound screening protocol from a universal transabdominal screening protocol.
Methods
This is a retrospective observational pre–post study examining the year prior to and year following a transition to a universal transvaginal ultrasound screening protocol to assess cervical length at the time of the anatomy survey. Prior to this transition, universal transabdominal cervical length screening was performed, with reflex transvaginal ultrasound measurement if transabdominal measurement was <35 mm or was unable to be obtained.
Results
A total of 1760 charts were reviewed; 962 charts were from the pre-transition/transabdominal year and 798 charts were from the post-transition/transvaginal year. In the post-transition/transvaginal year, cervical length less than 20 mm was identified in 1.5% of cases, compared to 0.7% of cases in the pre-transition/transabdominal year (p = 0.114). There was no difference in the rate of spontaneous preterm delivery between the two groups (5.1% in the pre-transition/transabdominal year vs. 6.9% in the post-transition/transvaginal year; p = 0.111).
Conclusions
In this pre-post study, introduction of a universal transvaginal cervical length screening did not decrease spontaneous preterm delivery rates or detection of short cervix <20 mm, compared to a protocol of universal transabdominal cervical length screening with reflex to transvaginal for measurement <35 mm.
Abbreviation
-
- MFM
-
- Maternal Fetal Medicine
1 INTRODUCTION
It has been well established that the short cervix is associated with increased risk of preterm delivery [1-5]. Currently, routine assessment of cervical length is recommended for all patients without prior preterm delivery between 18 and 22 6/7 weeks of gestation, with the aim of identifying patients with short cervix and, by extension, those patients at increased risk of preterm delivery [1]. The definition of short cervix has varied over time; it has been most frequently defined as either cervical length less than 25 mm or cervical length less than 20 mm [2]. Interventions for prevention of preterm delivery after identification of short cervix may include vaginal progesterone or cervical cerclage, depending on the patient's physical exam findings and the patient's prior obstetric history. Our study will look at the percentage of identified patients with a short cervix, as well as preterm delivery rates, before and after a protocol change in our academics, tertiary care center, and a Maternal Fetal Medicine (MFM) run ultrasound unit.
At midtrimester ultrasound, the mean cervical length is 35.2 ± 8.3 mm [6]. The best way to assess short cervix has yet to be determined, with protocols including transabdominal ultrasound, reflex to transvaginal ultrasound versus universal transvaginal cervical length ultrasound. Transvaginal ultrasound has been shown to have advantages to transabdominal ultrasound, with less effect from maternal body habitus, bladder size and the fetal presenting part [7]. In one center, with a policy for transabdominal cervical length measurements, with reflex to transvaginal cervical length ultrasound, 5.1% of their patients required a transvaginal cervical length for proper assessment [8]. Other studies have looked at physician willingness to perform transvaginal cervical length measurement, and have shown that 85% of physicians will perform transvaginal cervical length, but recommend it in populations at high risk of preterm delivery, and not for universal screening [9]. Some studies have shown that the specificity of transabdominal ultrasound for detection of a short cervix is around 30%, with over 50% of patients requiring a transvaginal cervical length for either concern for short cervix or proper assessment of cervical length [10].
Barriers to implementation of routine use of transvaginal screening may include the logistic workflow complications of transvaginal ultrasound probes as well as the impression that patients prefer a less invasive technique. Existing studies suggest that although transvaginal ultrasound is acceptable to many patients, a number of patients experience anxiety, pain, and even psychological trauma [11-13]. The performance of transvaginal ultrasound increases the time needed to complete the full ultrasound visit. Cleaning and storage of transvaginal ultrasound probes, while necessary, increases the length of the ultrasound visit and prolongs turnover time between patient visits. These barriers may add a considerable burden to practices, particularly those in low resource settings. Universal transvaginal ultrasound screening has also been shown to increase the diagnostic incidence of low lying placenta at time of cervical length screening, without increasing the incidence of persisting low lying placenta diagnosis at term, which may potentially lead to excessive follow up and iatrogenic intervention for false positives [14].
As the cervical lengths shortens, the risk of preterm delivery increases significantly. One study showed that with a midtrimester cervical length of 10 mm, the risk of preterm delivery was 10% and exponentially increased with shorter cervical lengths [15]. The risk of short cervix <20 mm was 1.2% in another retrospective study [16]. Beyond the importance of detection of short cervical length as a predictor for preterm delivery, there also needs to be adequate treatment in order to implement universal cervical length screening. In women with singleton pregnancy without a previous history of preterm birth, with cervical lengths 10–20 mm, the use of vaginal progesterone has been shown to decrease the risk of preterm delivery [17]. Similarly, Romero et al. in a large meta-analysis showed that with vaginal progesterone in singleton gestations with short cervix <25 mm, the use of vaginal progesterone decreased spontaneous preterm delivery <34 weeks, as well as neonatal deaths [18]. Another large study showed that in singleton pregnancies with transvaginal cervical length <15 mm, the relative risk with treatment with vaginal progesterone for delivery <34 weeks was 0.57, as compared to the placebo [19].
At this time, the American College of Obstetricians and Gynecologists states, “Regardless of the uncertainty about the utility of universal endovaginal cervical length screening for the prevention of preterm birth, the cervix should be visualized as part of the 18 0/7–22 6/7 weeks of gestation anatomy assessment … the cervix should be visualized at the 18 0/7–22 6/7 weeks of gestation anatomy assessment in individuals without a prior preterm birth, with either a transabdominal or endovaginal approach” [1]. This study aims to examine cervical length measurements before and after a universal transvaginal cervical length screening strategy was implemented, as well as vaginal progesterone use and rate of spontaneous preterm delivery.
2 MATERIALS AND METHODS
2.1 Study methods
This is a retrospective observational pre–post study. Prior to April 2018, at the time of anatomic survey between 17 0/7 and 22 6/7 weeks, in singleton pregnancies, a transabdominal cervical length measurement was performed on all singleton gestations without a history of previous preterm birth. If the measurement was <3.5 cm or appropriate cervical length measurements were unable to be obtained, a transvaginal ultrasound was performed. In patients with a previous preterm delivery, transvaginal cervical length screening was reviewed with the patient and pregnancy management plan was implemented at the discretion of the MFM physician. In general, at the time of this study, in patients with history of preterm delivery <34 weeks, serial cervical length examinations would be recommended, starting at 16 weeks, every 2 weeks until 23 weeks gestation. This study was approved by the Institutional Review Board at the Loyola University Medical Center, approval number IRB# 213872, approval date 7/16/2020. Starting in April of 2018, our MFM division changed our protocol to universal transvaginal ultrasound for all singleton pregnancies, 17 0/7–22 6/7 weeks, without a history of preterm delivery. In both pre- and post-groups, cervical length ≤20 mm, based on standard of care ACOG guidelines at the time of the study, was considered clinically significant cervical shortening and patients were offered treatment with vaginal progesterone. If an exam determined the cervix to be dilated, they were instead offered a physical examination indicated cerclage placement if eligible. All ultrasounds were performed by highly qualified MFM sonographers and read by our MFM group of four physicians. Our 2 study groups were from 4/2017 to 3/2018, the control group, compared to the intervention group, universal transvaginal ultrasound, 4/2018–3/2019 (Figure 1). All patients who had an anatomic survey from April 2017 to March 2019 were included, except as noted below in exclusion criteria. Identification of appropriate charts were via Digi-Sonics, our obstetric ultrasound reporting system. See Figure 1 for description of study groups.
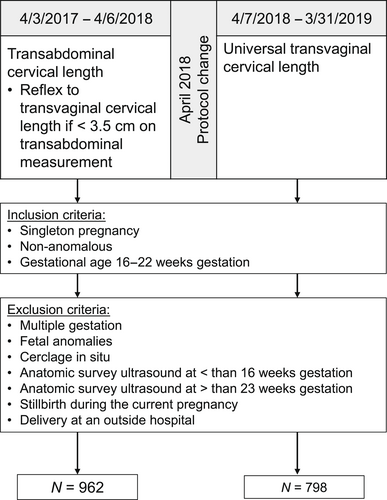
Flow diagram of patients included in the pre and post study of cervical length screening.
2.2 Data collection
Demographic, ultrasound, and delivery data were collected from the electronic medical record. Demographic and baseline data included age, BMI, chronic hypertension, pregestational diabetes, tobacco use, and history of prior preterm delivery (either spontaneous or medically indicated). Ultrasound and clinical data included gestational age at anatomy survey, whether transvaginal ultrasound was performed, cervical length estimate, identification of cervical length <20 mm, whether the patient was offered vaginal progesterone, and whether the patient used vaginal progesterone. Delivery data included gestational age at delivery, birthweight, spontaneous preterm delivery or preterm prelabor rupture of membrane with preterm delivery, and medically indicated preterm birth. Exclusion criteria consisted of: multiple gestation, fetal anomalies, cerclage in situ, anatomic survey ultrasound occurring at less than 16 weeks gestation or more than 23 weeks gestation, stillbirth during the current pregnancy, and delivery at an outside hospital. Spontaneous preterm delivery was defined as spontaneous preterm labor or prelabor rupture of membranes resulting in delivery prior to 37 weeks gestation, without a medical indication for preterm delivery.
2.3 Statistical analysis
The pre-transition/transabdominal and post-transition/transvaginal groups were compared using two-sample t-tests, Mann–Whitney U tests, Pearson's chi-square tests, or Fisher's Exact tests as statistically appropriate. Comparisons were repeated using stratification by history of prior preterm delivery. History of prior preterm delivery was determined by the reported obstetric history in the ultrasound report and did not differentiate between spontaneous or medically indicated. All analyses were performed using SPSS Statistics (version 27) and p < 0.05 was considered statistically significant.
3 RESULTS
A total of 1760 charts were reviewed; 962 charts were from the pre-transition/transabdominal year (4/3/2017–4/6/2018, the one year leading up to the transition to universal transvaginal screening for cervical length) and 798 charts were from the post-transition/transvaginal year (4/7/2018–3/31/2019, the year following the transition to universal transvaginal ultrasound screening). There were no statistically significant differences in age, hypertension, or tobacco use between the two groups (Table 1). The patients in the post-transition/transvaginal group had lower BMI, were less likely to have diabetes, and were more likely to have had a prior preterm delivery. There were statistically significant, but likely not clinically significant, differences in gestational age at anatomy ultrasound (19.0 vs. 18.6 weeks), gestational age at delivery (39.1 vs. 39.0 weeks), and birthweight (3258 vs. 3155 g) (Table 1).
| Variables | Pre-transition year 4/2017–4/2018 | Post-transition year 4/2018–4/2019 | p value |
|---|---|---|---|
| Transabdominal ultrasound (n = 962) | Transvaginal ultrasound (n = 798) | ||
| Age (years) | 30.0 ± 5.9 | 30.2 ± 5.9 | 0.565a |
| BMI (kg/m2) | 29.0 [25.0, 34.0] | 27.5 [23.6, 33.9] | <0.001 b |
| Hypertension (yes) | 56 (5.8) | 42 (5.3) | 0.611c |
| Diabetes (yes) | 57 (5.9) | 28 (3.5) | 0.019 c |
| Tobacco | 7 (0.7) | 5 (0.6) | 0.798c |
| Prior history of preterm delivery | 37 (3.8) | 59 (7.4) | 0.001 c |
| Gestational age at anatomy ultrasound (weeks) | 19.0 [18.3, 19.5] | 18.6 [18.3, 19.4] | 0.025 b |
| Gestational age at delivery (weeks) | 39.1 [38.0, 39.4] | 39.0 [37.3, 39.3] | <0.001 b |
| Birthweight (g) | 3258 ± 590 | 3155 ± 658 | <0.001 a |
| Transvaginal ultrasound performed (yes) | 32 (3.3) | 638 (79.9) | <0.001 c |
| Cervical length estimate (mm) | 40.6 ± 6.2 | 39.9 ± 7.2 | 0.033 a |
| Identified cervical length <20 mm | 7 (0.7) | 12 (1.5) | 0.114c |
| Offered vaginal progesterone | 4 (0.4) | 10 (1.3) | 0.049 c |
| Used vaginal progesterone | 4 (0.4) | 8 (1.0) | 0.136c |
| Spontaneous preterm delivery or PPROM with PTD | 49 (5.1) | 55 (6.9) | 0.111c |
| Medically indicated preterm birth | 48 (5.0) | 52 (6.5) | 0.168c |
- Note: Data are presented as mean ± SD, median [P25, P75], or No. (%). Bold indicates p < 0.05.
- a Student's t test.
- b Mann–Whitney U test.
- c Pearson Chi-Square.
In the pre-transition/transabdominal year, transvaginal ultrasound was used to confirm cervical length if length was less than 35 mm on transabdominal ultrasound or if cervical length was unable to be obtained transabdominally. In this group, transvaginal ultrasound was performed in 3.3% of cases. In the post-transition/transvaginal year, transabdominal ultrasound was used to measure cervical length if the patient declined transvaginal ultrasound. Transvaginal ultrasound was performed in 79.9% of cases. Patients declined transvaginal ultrasound 20% of the time (Table 1).
At the time of study implementation, our MFM group was utilizing 20 mm as the cutoff for short cervix in those patients without a previous history of preterm delivery. 20 mm was the standard of care per ACOG guidelines. This group of patients would be offered vaginal progesterone, or if appropriate based on physical examination, a physical examination indicated cerclage. In the post-transition/transvaginal year, cervical length less than 20 mm was identified in 1.5% of cases, compared to 0.7% of cases in the pre-transition/transabdominal year (p = 0.114) (Table 1). The post-transition/transvaginal year had a mean cervical length estimate of 39.9 mm (SD = 7.2 mm), compared to 40.6 mm (SD = 6.2) in the pre-transition/transabdominal year (p = 0.033); a statistically significant difference that is likely not clinically significant. Vaginal progesterone was offered to 1.3% of patients in the post-transition/transvaginal year compared to 0.4% of patients in the pre-transition/transabdominal year (p = 0.049). Vaginal progesterone was declined by two of the patients in the post-transition year, so the number of patients taking vaginal progesterone between the 2 groups was not statistically significant. Ultimately, when examining the outcomes of these pregnancies, there was no difference in the rate of spontaneous preterm delivery between the two groups (5.1% in the pre-transition/transabdominal year vs. 6.9% in the post-transition/transvaginal year; p = 0.111).
Because the post-transition/transvaginal year had a higher percentage of patients with history of prior preterm delivery, suggesting a potentially higher risk of subsequent preterm delivery in that cohort, and similarly a potentially higher risk of short cervix in that cohort, data were then stratified post hoc by history of prior preterm delivery (Table 2). In patients with no prior history of preterm delivery, cervical length less than 20 mm was identified in 1.5% of cases in the post-transition/transvaginal year compared to 0.6% of cases in the pre-transition/transabdominal year (p = 0.048). In patients that did have a prior history of preterm delivery, there was no difference in detection of cervical length less than 20 mm between the pre-transition/transabdominal year and post-transition/transvaginal year (Table 2).
| Variables | No prior history of preterm delivery | Prior history of preterm delivery | ||||
|---|---|---|---|---|---|---|
| Pre-transition year | Post-transition year | p | Pre-transition year | Post-transition year | p | |
| Transabdominal ultrasound (n = 925) | Transvaginal ultrasound (n = 739) | Transabdominal ultrasound (n = 37) | Transvaginal ultrasound (n = 59) | |||
| Age (years) | 30.0 ± 5.9 | 30.0 ± 5.8 | 0.960a | 29.2 ± 5.6 | 32.0 ± 5.7 | 0.022 a |
| BMI (kg/m2) | 29.0 [25.0, 34.0] | 27.2 | <0.001 b | 30.0 [24.3, 34.0] | 31.1 [25.3, 39.2] | 0.212b |
| Gestational age at anatomy ultrasound (weeks) | 19.0 [18.3, 19.5] | 18.6 [18.3, 19.4] | 0.030 b | 18.6 [18.2, 19.4] | 18.5 [18.3, 19.3] | 0.997b |
| Gestational age at delivery (weeks) | 39.1 [38.1, 39.5] | 39.0 | <0.001 b | 37.2 [35.4, 38.8] | 37.4 [36.2, 39.0] | 0.557b |
| Birthweight (grams) | 3273 ± 575 | 3177 ± 639 | 0.001 a | 2882 ± 813 | 2886 ± 822 | 0.981a |
| Cervical length estimate (mm) | 40.7 ± 6.0 | 39.8 ± 7.1 | 0.008 a | 38.5 ± 9.6 | 41.1 ± 8.2 | 0.160a |
| Identified cervical length <20 mm | 5 (0.5) | 11 (1.5) | 0.048 c | 2 (5.4) | 1 (1.7) | 0.557d |
| Offered vaginal progesterone | 4 (0.4) | 9 (1.2) | 0.071c | 0 (0) | 1 (1.7) | 1.00d |
| Used vaginal progesterone | 4 (0.4) | 7 (0.9) | 0.233d | 0 (0) | 1 (1.7) | 1.00d |
| Spontaneous preterm delivery or PPROM with PTD | 39 (4.2) | 44 (6.0) | 0.106c | 10 (27.0) | 11 (18.6) | 0.334c |
| Medically indicated preterm birth | 42 (4.5) | 41 (5.5) | 0.348c | 6 (16.2) | 11 (18.6) | 0.762c |
- Note: Data are presented as mean ± SD, median [P25, P75], or No. (%). Bold indicates p < 0.5.
- a Student's t test.
- b Mann Whitney U test.
- c Pearson Chi-Square.
- d Fisher's Exact test.
4 DISCUSSION
Our study suggests that in an academic, tertiary care center, with an ultrasound unit run by MFM sub-specialists, there is no difference in ability to detect short cervix between universal transvaginal cervical length screen, as compared to universal transabdominal cervical length screening was performed, with reflex transvaginal ultrasound measurement if transabdominal measurement was <35 mm or was unable to be obtained. There was no difference in the detection rate of cervical length less than 20 mm or spontaneous preterm delivery rates in the year using universal transabdominal cervical length screening compared to that in the year using universal transvaginal cervical length screening. Mean cervical length although statistically different, was clinically equivalent in the two groups. There were higher rates of offering vaginal progesterone, 10 (1.3%) compared to 4 (0.4%) patients (p = 0.049), in the universal transvaginal ultrasound screening group.
There was no difference in spontaneous preterm birth rate in the pre-transition/transabdominal year as compared to the post-transition/transvaginal year (5.1% vs. 6.9%, p = 0.111). This is important note, as our demographics had a higher rate of history of preterm delivery in the post-transition/transvaginal year (7.4% compared to 3.8%). Patients declined transvaginal ultrasound 20% of the time in the post-transition/transvaginal year. In the post-transition/transvaginal year, cervical length less than 20 mm was identified in 1.5% of cases, compared to 0.7% of cases in the pre-transition/transabdominal year (p = 0.114) (Table 1). Vaginal progesterone was offered to 1.3% of patients in the post-transition/transvaginal year compared to 0.4% of patients in the pre-transition/transabdominal year (p = 0.049). Vaginal progesterone was declined by two of the patients in the post-transition year.
The similarity in detection rates of cervical length less than 20 mm suggests that universal transabdominal cervical length screening is a reasonable alternative to universal transvaginal ultrasound screening in our population, particularly if universal transvaginal ultrasound is a significant burden on resources within a practice. In the pre-transition/transabdominal year, transvaginal ultrasound was used to confirm cervical length if the transabdominal cervical length measurement was less than 35 mm. In our study, transvaginal ultrasound only needed to be performed in 3.3% of cases during the pre-transition/transabdominal year, despite our cut-off being on the conservative side. Previous studies have investigated optimal cut-offs to transition from transabdominal cervical length measurement to transvaginal cervical length measurement, which have ranged from 29 to 36 mm [20-23].
During the timeframe of this study (both in the pre-transition year and the post-transition year), vaginal progesterone was offered if a cervical length less than 20 mm was identified, in alignment with ACOG recommendations at that time. Our results showed no difference in detection rate of cervical length less than 20 mm (0.7% pre-transition year vs. 1.5% post-transition year; p = 0.114). Since this timeframe, there has been a change in ACOG recommendations regarding the use of vaginal progesterone in patients with cervical length <25 mm without a history of previous preterm delivery. Because during the timeframe of the study 20 mm was the cut-off of interest at which clinical management would change, it is difficult to make conclusions about a different cut-off which is now used in clinical management.
There is still controversy regarding whether transabdominal ultrasound or transvaginal ultrasound should be used for the routine assessment of cervical length [24, 25]. Some studies have suggested difficulty with obtaining reliable transabdominal cervical length images [26]. A recent pre–post study in France found that implementation of a universal transvaginal ultrasound screening protocol decreased the risk of the preterm delivery [27]. Our study did not duplicate these findings. Of note, in the French study, cervical lengths were only obtained in 28.9% of scans in the pre-period and in 52.9% of scans in the post-period [27]. This differs from our clinic practice in which cervical length is obtained in virtually 100% of scans. Another study in the U.S. found that introduction of transvaginal ultrasound cervical length screening did decrease the risk of preterm delivery in patients without a prior history of preterm birth [28]. In addition, a large meta-analysis of transvaginal cervical length ultrasound showed that with universal transvaginal cervical length screening, as compared to no screening, there was a reduction in spontaneous preterm delivery [29]. Our study is different because it clearly compares two different methods of cervical evaluation, instead of no screening of the cervical length. There remain challenges to transvaginal cervical length imaging, with financial questions, patient preference for less invasive methods and sonographer experience required to perform the proper imaging [30]. Further data is needed to assess how this protocol and its use could be expanded to outside clinics, as well as how the recent change in recommendation to use of vaginal progesterone for cervical length <25 mm for women without a history of preterm delivery affects these patterns. Additionally, more research examining the cost effectiveness of universal transvaginal screening is needed.
The strengths of this study include performance in a large, academic medical center with a dedicated MFM ultrasound team and interpretation by MFM physicians. The counseling of patients was performed by four MFM physicians based on a division specific protocol, to ensure patients were treated appropriately. Our study had few patients that were lost to follow-up, given our large population of internal referrals. The major limitations of this study are those inherent to the pre-post design and retrospective data collection. Data collection of clinical history was limited to that available in the ultrasound report and delivery report. This was an observational study and thus was not powered to be able to detect any specific differences in outcomes. This type of pre-post study assumes that the patient population and underlying risk of spontaneous preterm birth are equivalent in the pre-transition and post-transition years, which may not be true due to either shifts in patient populations served by the institution or due to changes in overall population health. Causality cannot be assumed in a pre-post study. The similar rates of spontaneous preterm delivery and medical indicated preterm delivery (Table 1) suggest that the two groups were overall similar in risk. This study was conducted in an ultrasound unit with skilled MFM sonographers, with imaging read immediately by MFM physicians, so the study results will not be valid in all ultrasound units.
Our study shows that with the transition to a universal transvaginal cervical length screening program, 80% of patients agreed to the intervention. Our study also shows that there was no clinical difference in mean cervical length measurement or the ability to detect a cervical length <20 mm, when comparing the pre and post groups.
5 CONCLUSIONS
In this pre-post study, introduction of a universal transvaginal cervical length screening did not decrease spontaneous preterm delivery rates or detection of short cervix <20 mm, compared to a protocol of universal transabdominal cervical length screening with reflex to transvaginal for measurement <35 mm.
AUTHOR CONTRIBUTIONS
Emily Holthaus: Data curation (equal); formal analysis (equal); validation (equal); writing—original draft (equal); writing—review & editing (equal). Layan Alrahmani: Methodology (equal); supervision (equal); writing—review & editing (equal). Nicole Sprawka: Conceptualization (equal); methodology (equal); validation (equal); writing—review & editing (equal). Jean Ricci Goodman: Conceptualization (equal); methodology (equal); project administration (equal); supervision (equal); writing—review & editing (equal). Ann Lal: Conceptualization (equal); formal analysis (equal); investigation (equal); methodology (equal); project administration (equal); supervision (equal); validation (equal); writing—original draft (equal); writing—review & editing (equal).
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
This study was approved by the Institutional Review Board at the Loyola University Medical Center, approval number IRB# 213872, approval date 7/16/2020.
INFORMED CONSENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.