Internet Published Policies Regarding Liver Transplant Eligibility and Substance Use in United States Transplant Centers
Supported by the Wisconsin Partnership Program, Middleton VA Hospital, and School of Medicine and Public Health (to the Preventive Medicine Residency Program).
Potential conflict of interest: Dr. Lucey received grants from AbbVie, Gilead, and Pharmasolutions. The other authors have nothing to report.
Corrections added on October 28, 2020, after first online publication: In Abstracts section, the sentence “This study aims to define the availability and content of liver transplants.” has been corrected to “This study aims to define the availability and content of liver transplant centers' publicly available Internet policies regarding eligibility criteria for liver transplant.”.]
Abstract
Liver transplant centers in the United States retain great autonomy in determining eligibility criteria for a liver transplant. This study aims to define the availability and content of liver transplant centers' publicly available Internet policies regarding eligibility criteria for liver transplant. Three trained undergraduate students performed a structured pilot-tested assessment of official websites of the United Network for Organ Sharing-registered liver transplant centers. All 141 liver transplant centers had an accessible website. Some account of eligibility criteria was provided by 53% of centers, while 32% of centers discussed substance use. Only 17% discussed their policy regarding alcohol use in candidates with underlying alcohol use disorder, and only 2% stipulated that 6 months of abstinence was required. While exclusion based on substance use or age was discussed infrequently, insurance coverage requirements, the need for social support, and the need for adherence to medical care were mentioned in 21%, 37%, and 23% of centers, respectively. Conclusion: In 2018, half of liver transplant centers provided some information on their official websites regarding eligibility criteria for liver transplant. Detailed information regarding substance use disorders and social health requirements was rare. The Internet is infrequently used by liver transplant centers as a means to publicly share information regarding selection criteria.
Abbreviation
-
- UNOS
-
- United Network for Organ Sharing
Liver transplantation is the standard of care for the treatment of patients with end-stage liver disease, hepatocellular carcinoma, and acute liver failure. With limited deceased donor organ availability and over 13,400 patients currently on the liver transplant waiting list,(1) defining patient selection criteria for transplantation is crucial. Current guidelines and guidance recommend performing a standard medical evaluation while also ensuring adequate social support, financial approval, insurance support, as well as a thorough psychosocial evaluation, including substance abuse or other psychosocial issues.(2, 3) With regards to alcohol-related liver disease, guidelines discuss inclusion of an addiction specialist and treatment plan. Importantly, 2019 practice guidance states candidate selection for liver transplantation should not be based solely on a fixed interval of abstinence(4) given its inconsistent ability to predict relapse rates after a liver transplant.(5) Although helpful, such publications provide only general recommendations, permitting liver transplant centers great autonomy and flexibility in determining their specific selection policies.
Variations in candidate selection practices have also been reported,(6-8) although the true landscape of selection variability concerning the myriad of issues and controversies surrounding liver transplant selection remains uncertain. Furthermore, a recent study discovered significant knowledge gaps in patients’ understanding of center-specific options while also revealing that transplant candidates value such information given its impact on their decisions and access to transplant.(9) Many also believe that considering more than one transplant program is reasonable.(10) Thus, there is a need to provide accessible, transparent, patient-centered information regarding transplant center-specific selection policies and practices to enhance patient decision making.
In recent years, the internet has become both a popular and important source of medical information for patients and families with known benefits and limitations.(11, 12) It is estimated that 82% of U.S. adults use the internet, of which 72% say they have looked online for health information during the preceding year.(12) The Scientific Registry of Transplant Recipients is one such online resource that reports program-specific information regarding transplant program performance. Although this resource is continually refined in an effort to provide relevant and understandable data to patients, providers, and the general public,(13) it does not include program selection policies. Thus, the official websites of liver transplant centers may be the only internet resource to publicly find such information, although it is unknown how often or how completely it is published.
This study aims to define the availability and content of liver transplant centers’ internet published policies by direct assessment of the institutions’ websites regarding eligibility criteria for liver transplantation, particularly regarding exclusions based on substance use of any kind, age, medical diagnoses, insurance coverage requirements, social support requirements, and medical nonadherence. We hypothesize that liver transplant programs infrequently use the internet to publicly share their selection policies because of the prevalence of various forms of stigma associated with these exclusion factors.(14)
Materials and Methods
We first designed a simple pro forma for use in the assessment of access and quality of content regarding center-specific policies on eligibility for liver transplantation, as published on the internet. The assessment tool is shown in Supporting Appendix S1.
In April 2018, three undergraduate college students (the “reviewers”) who were unconnected with any liver transplant program were recruited to assist in the study. Each reviewer was between the ages of 19 and 20 years old, was currently enrolled in a 4-year undergraduate institution, reported being fluent in English, and felt either comfortable or somewhat comfortable using the internet. The reviewers were trained by three of the authors (M.N.G., J.L.E., D.A.T.) on the use of the assessment tool. The reviewers were coded so that the authors were blinded to their identities when reviewing the study data. In the case of negative searches, the reviewers were allotted a maximum of 15 minutes per institution to find the relevant information. Specific instructions were provided to standardize the way in which each reviewer searched for the institution’s information. They were advised to begin their search in google.com by typing “[institution name as listed on the website of the United Network for Organ Sharing (UNOS): www.UNOS.org] + liver transplant eligibility policy.” They were then instructed to choose the most appropriate link they felt would lead them to the correct information. If an appropriate link was not identified, they were advised to go to the institution’s website and search “liver transplant eligibility policy” in the search bar. If the above two methods did not yield the appropriate information, they would then navigate the internet freely until the desired information was found or until 15 minutes elapsed. For each institution, the reviewers noted if they found eligibility criteria for liver transplantation. If criteria for selection were identified within 15 minutes, the full assessment was completed without time restrictions, otherwise it was deemed a negative search. Each reviewer received a small stipend for their participation.
The UNOS website(1) was accessed in July 2017 to determine the number of available liver transplant centers. The authors compiled a list of all 141 UNOS-registered liver transplant centers, including both adult and pediatric liver transplant centers. As of July 2017, a total of 4,082 liver transplants were performed across all centers during 2017 and 7,879 were performed across all centers during 2016. In addition to deceased donor liver transplants, 102 of the centers performed living donor liver transplants. Of the 141 UNOS-registered centers, 54 performed liver transplantation for pediatric recipients in 2016, accounting for 573 (7%) of liver transplants performed during the same year.
The reviewers accessed the official websites of the UNOS-registered liver transplant centers from April 8, 2018, through April 30, 2018. Each of the three reviewers received 47 unique liver transplant centers, randomized by the authors. Ten programs were randomly selected and evaluated by all three reviewers to determine interobserver reliability; this demonstrated 93% agreement for availability of eligibility criteria.
In centers for which the website provided some information on eligibility criteria, the reviewers were instructed to search whether or not the available policy mentioned the transplant selection policy in relation to substance use of any kind by a candidate or more specifically substance use disorders, such as alcohol, alcohol dependence (alcohol use disorder), use of tobacco, marijuana, illicit drugs (e.g., cocaine, heroin, methamphetamine), or misuse or abuse of prescription drugs (e.g., opioids, benzodiazepines). If any of the above were mentioned, the reviewers recorded the information separately in relation to each of the above substance use topics and noted if a period of abstinence or therapy was required to be eligible for liver transplantation. The assessment further evaluated whether the available policies discussed exclusions based on age or certain diagnoses or disorders, insurance coverage requirements, social support requirements, or a discussion of medical nonadherence.
Results
All 141 liver transplant centers had an accessible website at the time of assessment. Some description of selection criteria for liver transplantation was identified in 74 centers (52.5%). Of the centers that made their selection policies available to the public through their website, 45 (31.9% of all 141 centers) included a discussion in some fashion of substance use or substance use disorders. Twenty-six centers (18.4%) discussed their selection policy regarding a history of alcohol use in so far as these applied to every candidate. Six of those centers (4.3%) required a 6-month period of abstinence for every patient, whereas two centers (1.4%) had a case-by-case application of a required period of abstinence. Information regarding substance use was mentioned as follows: tobacco use (13 centers, 9.2%), illicit drug use (e.g., cocaine, heroin) (13 centers, 9.2%), marijuana use (three centers, 2.1%), prescription drug use (two centers, 1.4%), and prescription misuse or abuse (e.g., opioids, benzodiazepines) (five centers, 3.5%) (Table 1).
| Topic | Any Information Regarding Selection | Some Interval of Abstinence Is Required | 6 months of Abstinence Required | Eligibility Determined on a Case-by-Case Basis | Addiction Therapy Is Required |
|---|---|---|---|---|---|
| Alcohol (every patient) | 26 (18%) | 6 (4%) | 6 (4%) | 2 (1%) | |
| Alcohol (alcohol use disorder) | 24 (17%) | 6 (4%) | 3 (2%) | 7 (5%) | 12 (9%) |
| Tobacco | 13 (9%) | 1 (1%) | 1 (1%) | 3 (2%) | 3 (2%) |
| Marijuana | 3 (7%) | 0 (0%) | 0 (0%) | 1 (1%) | 0 (0%) |
| Illicit drugs | 13 (9%) | 6 (4%) | 5 (3%) | 2 (1%) | 5 (3%) |
| prescription use | 2 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Prescription misuse/abuse | 5 (3%) | 1 (1%) | 0 (0%) | 1 (1%) | 2 (1%) |
- Data show number (percentage).
Twenty-four centers (17.0%) discussed their selection policy regarding alcohol use by potential candidates with alcohol use disorder. Six centers (4.3%) required a period of abstinence, ranging from 3 to 24 months (median 6 months), while selection criteria in seven centers (5.0%) were on a case-by-case basis. Twelve centers (8.5%) stated that they required therapy for alcohol use disorder before that candidate could become eligible for liver transplantation; however, in no case was the type of therapy explicitly stated (Table 1).
Exclusion based on age was discussed in 13 centers (9.2%), and a specific upper and lower age threshold was mentioned in nine. Specifically, six centers noted exclusion of patients younger than age 18 years, whereas three centers excluded patients over the age of 60 years. One center each specified exclusion of liver transplantation in patients over the ages of 70, 72, and 75 years. One center reported the age cutoff to be on a case-by-case basis. Twenty-nine (20.5%) centers stated that they review a patient’s insurance coverage as a criterion for eligibility for liver transplantation, with eight (5.7%) of those centers noting that insurance companies must agree to pay for the cost of the medications and transplant before evaluation and liver transplantation. When discussing social support requirements, 52 centers (36.9%) discussed the need for general social support while 21 (14.9%) made specific social support requirements. For instance, one transplant program noted that the “support system [must] understand the risks of liver transplants” and that “they are committed and compliant with what is needed before and after transplant.” Medical nonadherence was mentioned in the websites of 22.6% of centers and would lead to exclusion from liver transplantation at 11 centers (7.8%) (Table 2).
| Variable | Review | Specific Requirements | Case-by-Case |
|---|---|---|---|
| Insurance | 29 (21%) | 8 (6%) | 15 (11%) |
| Social support | 52 (37%) | 21 (15%) | |
| Noncompliance | 32 (23%) | 11 (8%) |
- Data show number (percentage).
Exclusion based on particular diagnoses or disorders was discussed in 53 centers (37.5%). Briefly, some of the etiologies discussed that would preclude a patient from undergoing liver transplantation included cancer outside the liver (24, 17%), tuberculosis (19, 13%), severe heart disease (17, 12%) and lung disease (12, 9%), unspecified psychiatric disorder (9, 6%), anxiety and depression (2, 1%), human immunodeficiency virus positive (6, 4%), acquired immune deficiency syndrome (6, 4%), severe obesity (7, 5%), and portal vein thrombosis with or without mesenteric vein thrombosis (5, 4%) (Table 3).
| Diagnoses/Disorders* | Centers that Exclude† |
|---|---|
| Cancer outside the liver | 24 (17%) |
| Tuberculosis | 19 (13%) |
| Severe heart disease | 17 (12%) |
| Severe lung disease | 12 (9%) |
| Unspecified psychiatric disorder | 9 (6%) |
| Severe obesity | 7 (5%) |
| Human immunodeficiency virus positive | 6 (4%) |
| Acquired immune deficiency syndrome | 6 (4%) |
| Portal vein thrombosis with or without mesenteric vein thrombosis | 5 (4%) |
| Anxiety/depression | 2 (1%) |
- * n = 53 centers (38%).
- † Out of all 141 centers.
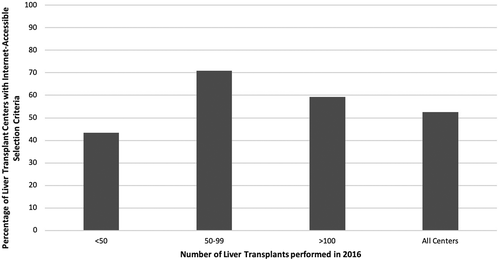
Because the reviewers accessed the UNOS website in July 2017, we used the total number of liver transplant numbers performed in 2016, encompassing a full calendar year, to evaluate internet policy variability associated with liver transplant centers’ yearly transplant volume. Of the 141 centers that performed liver transplants in 2017, 27 (19%) performed more than 100 transplants in 2016, 31 (22%) performed between 50 and 99 transplants in 2016, and 83 (59%) performed less than 50 transplants in 2016. Of the largest centers (those performing ≥100 liver transplants in 2016) and medium-sized centers (those performing 50-99 liver transplants in 2016), 59% (16 centers) and 71% (22 centers), respectively, provided publicly accessible information regarding their selection criteria for transplantation. In contrast, smaller centers (performing <50 liver transplants in 2016) were less likely to have publicly available liver transplant eligibility criteria, with only 36 centers (43%) publishing some account of their selection practices (Fig. 1).
Discussion
In 2001, the Institute of Medicine’s white paper Crossing the Quality Chasm(15) listed “effective use of information technologies” as one of its redesign imperatives. It stated that “patients should be given the necessary information and opportunity to exercise the degree of control they choose over health care decisions that affect them.” The internet has become one of the principle sources of information for the general public regarding health information.(11) Almost 60% of American adults looked online for health information over a 1-year period, most frequently searching for information regarding a specific disease, medical problem, particular medical treatment, or procedure.(12)
The present study is an investigation of the nexus of information technology and the public, including patient (and patient’s family) access to center-specific information regarding selection criteria for liver transplantation. We sought to study this nexus through a structured pilot-tested assessment of the websites of UNOS-listed U.S. liver transplant centers. We were specifically interested in information regarding selection criteria. Our hypothesis that transplant programs infrequently use the internet to publicly share their selection policies was correct. Roughly half of the programs provided some information on their selection guidelines. Thirty-two percent of all centers discussed substance use of any kind in general, and few programs offered specifics of the policy surrounding selection and management of substance use disorders.
We also noted that larger centers (those performing more than 50 liver transplants in 2016) were more likely than smaller centers to have publicly available liver transplantation selection criteria. While there was some regional distribution between UNOS centers that had available information versus those that did not (data not shown), this was extremely variable. For instance, while more than 70% of centers in regions 7 and 10 (representing the midwestern states) had eligibility criteria found on the internet, the northeast regions of the country were much less consistent, ranging from 29% to 71% in the availability of eligibility criteria.
We speculate several reasons for the paucity of information provided by the transplant centers. One possibility is stigma attached to alcohol use disorder and other substance use disorders, culminating in fears that publicizing transplants for patients with such conditions will reflect negatively on the program or more generally on support for liver transplantation. Specifically with regards to alcohol-related liver disease, one form of stigma may include “a perceived injustice in granting such a scarce resource to a patient who, it is believed, bears at least some personal responsibility for their liver disease.”(16) These patients may therefore be viewed as “less deserving” of a liver transplant. A second form of stigma includes concern for the medical suitability and risk of posttransplant relapse.
Overall, however, it appears liver transplantation for patients with alcohol-related liver disease is becoming more acceptable to the public. An online survey of 503 participants in 2015 noted that 82% of respondents had at least a neutral attitude toward early transplantation for patients with any form of alcohol-related liver disease.(17) Alcohol-related liver disease has become the most common indication for liver transplantation in the United States.(18) The survival of patients receiving a transplant for alcohol-related liver disease, including those with severe alcoholic hepatitis, is similar in the first 5 years to those receiving liver transplants for other indications, although there may be a decline in the second 5 years, particularly for patients who are cigarette smokers.(19-21) Thus, with careful selection of patients, liver transplantation for alcohol-related liver disease may not be as controversial as previously thought. Similar outcome and interventional studies focusing on substance use disorders beyond alcohol as well as other controversial factors surrounding liver transplant selection are likely to further shape practice and public opinion.
A second possibility may be that some centers and patients believe that the internet is not the optimal or only medium for such pertinent and in certain situations complex information and multidisciplinary decision making to be effectively communicated to all. Although patients’ use of the internet surrounding choosing a liver transplant center is currently unknown, a 2019 study examining how patients choose kidney transplant centers found only a small number of patients had used online resources to identify and evaluate a particular center, citing limited internet access, computer literacy, and concerns regarding the trustworthiness of online information.(22) Other national assessments have also found those with higher levels of health literacy were more likely to use digital resources for health information.(23) Furthermore, current medical and surgical society health care websites are designed for health care professionals and not patients.(24) The internet also has been found to act at times as a platform for advertisement and a “revenue provider” rather than communicating with patients and providing evidence-based health information.(25) Despite these concerns, Schaffhausen et al.(9) recently created an internet-based tool to aid patients in understanding variations in recipient and donor characteristics across liver transplant centers to ultimately select a center. Importantly, this tool received positive feedback from patients undergoing a liver transplant. Thus, many of the concerns surrounding use of the internet, including inequalities in health information accessibility,(26) may be ameliorated by patient-centered focuses.
A third possibility is a lack of consensus among transplant providers and managers in a particular program, leading to an absence of clear center-specific policies, as found by Secunda et al.(7) in a national survey of U.S. transplant providers’ opinions. The same study further found that less than half of centers had written policies regarding transplantation eligibility, which was further confirmed by our study with regards to internet publication. Program policies regarding alcohol and marijuana use are inconsistent, as demonstrated by a survey in 2018.(27) Less than half of programs required a specific period of abstinence before liver transplantation for alcohol-related liver disease, while only one quarter of programs enforced the 6-month abstinence policy. Marijuana use, particularly for medicinal purposes, was also more accepted.(27) Similarly, policies toward chronic opioid and opioid substitution therapy use in liver transplant candidates vary significantly among centers, and a majority of programs admittedly lack a written policy regarding this topic.(28) Some centers may avoid written policies completely to avoid “pigeonholing” themselves amid a continually evolving landscape of transplant practices. We also must acknowledge the potential for paternalism, concealment, and patient disempowering throughout the entire liver transplant process.(29)
We acknowledge that our study has several limitations. First, liver transplant centers may elect to use alternative forms of documentation and communication to define and disseminate selection policies to patients. These may include handbooks, in-person consultation, or other forms of publication, some of which may only be accessible to institution members or discussed during a visit with a clinician or hospital resource center. None of these were reviewed or included in this study and therefore would have been missed. In addition, our search criteria may not reflect what patients and their families might use when searching for this information. We also did not assess whether any of the websites included languages other than English. Our data do not elucidate the manner by which internet-published information affects patient or referring provider actions or whether individual programs abide by the policies they publish. Finally, our reviewers may not reflect the educational background and experience of those who might be searching for this type of information.
Despite these limitations, there are several strengths to our study. Every UNOS-listed liver transplant center that performed liver transplants in 2017 was evaluated for the presence of a website and eligibility criteria. The reviewers performing the assessment were nonmedical professionals with their identities blinded to the authors, although they may have been more literate than the general population and were all English speakers. However, this is more likely to bias the study toward finding rather than obscuring transplant information on the internet.
Our evaluation indicates that transplant programs infrequently employ the internet to provide prospective patients, their families, and referring providers information regarding selection policies for liver transplantation. In an era when patients are increasingly seeking health information both within and outside the clinic, the liver transplant community should work diligently to optimize multiple resources, including the internet, to provide all patients with accurate, complete, and patient-friendly information. We suggest that all liver transplant programs make clear statements regarding the following on their websites: (1) evaluation including urgency, age, medical comorbidities, and a history of medical nonadherence to determine medical suitability for transplantation; (2) insurance coverage to ensure financial support; (3) assessment of social support; (4) an evaluation of substance use in all patients, especially those with substance use disorders, including the need for abstinence, counseling, or other treatment; and (5) any other reasons for exclusions. Such statements should reflect the certainty of the program’s policies and practices regarding each issue and can include case-by-case assessments, highlighting the often complex multidisciplinary decision making and the use of the internet as an adjunct, not a substitute, for other transplant information sources. With this transparent patient-friendly information in hand, prospective patients and families will have the tools needed to be engaged and active participants in their health care.




