Retrospective matched cohort study of incidence rates and excess length of hospital stay owing to pressure injuries in an Asian setting
Abstract
Background
Little is known about stage 1 and 2 pressure injuries that are health care-acquired. We report incidence rates of health care-acquired stage 1 and stage 2 pressure injuries, and, estimate the excess length of stay using four competing analytic methods. We discuss the merits of the different approaches.
Methods
We calculated monthly incidence rates for stage 1 and 2 health care-acquired pressure injuries occurring in a large Singapore acute care hospital. To estimate excess stay, we conducted unadjusted comparisons with a control cohort, performed linear regression and then generalized linear regression with a gamma distribution. Finally, we fitted a simple state-based model. The design for the cost attribution work was a retrospective matched cohort study.
Results
Incidence rates in 2016 were 0.553% (95% confidence interval [CI] 0.55, 0.557) and 0.469% (95% CI 0.466, 0.472) in 2017. For data censored at 60 days’ maximum stay, the unadjusted comparisons showed the highest excess stay at 17.68 (16.43-18.93) days and multi-state models showed the lowest at 1.22 (0.19, 2.23) days.
Conclusions
Poor-quality methods for attribution of excess length of stay to pressure injury generate inflated estimates that could mislead decision makers. The findings from the multi-state model, which is an appropriate method, are plausible and illustrate the likely bed-days saved from lowering the risk of these events. Stage 1 and 2 pressure injuries are common and increase costs by prolonging the length of stay. There will be economic value investing in prevention. Using biased estimates of excess length of stay will overstate the potential value of prevention.
Abbreviations
-
- CI
-
- confidence interval
-
- EUR
-
- Euro
-
- GLM
-
- generalized linear model
-
- SD
-
- standard deviation
-
- USD
-
- United States Dollars
1 INTRODUCTION
The epidemiology of health care-acquired pressure injury has likely changed in recent decades. Serious pressure injuries graded as stages 3 and 4 now arise less frequently during a patient's admission [1] and this is likely owing to the establishment of patient safety programs in many settings [2-4].
Our knowledge of incidence rates and the associated costs, by stage of pressure injury, is incomplete. A recent systematic review and meta-analysis that included evidence from 2008 to 2018 [5] found the overall rate of health care-acquired pressure injuries to be 8.4% (95% confidence interval [CI] 7.6%–9.3%). When stage 1 injuries were excluded, this declined to 5.1% (95% CI 4.6%–5.6%). Evidence from a 2020 Singapore-based study showed health care-acquired stage 3 and 4 pressure injuries only arose among 1 or 2 patients per 10,000 admitted between 2016 and 2020 [6]. A reproducible review of the literature for the period 1980−2014 [7] found 26 studies that reported information about the incidence of pressure injury. Only one of these studies reported data for incidence rates according to stage of pressure injury, [8] with stage 1 accounting for 3.1%, stage 2 for 3.2%, stage 3 for 0.1%, and with no stage 4 injuries. A systematic review of health care-acquired pressure injuries in pediatric populations [9] found that the cumulative incidence was in the range 3.7%−27% and the attributable length of hospital stay was between 0.9 and 14.1 days, with costs estimated between USD 894 and USD 98,730. An Australian study regarding the impact of health care-acquired pressure injuries on acute hospital length of stay reported 4.31 excess days for all grades of pressure injury [10]. An Iranian study on the incidence and costs of pressure injuries among intensive care units found 8.9% of patients developed pressure injury and the treatment costs varied from USD 12 for stage 1 to USD 66,834 for stage 4. The authors of a systematic review of cost-of-illness studies for all chronic injuries [11] concluded that there was variability in the methods, perspectives, cost components, and jurisdictions, making the interpretation of costs difficult. Nevertheless, those authors concluded that the 1-year cost for a pressure injury was USD 15,400, but no estimates were made for the different stages of injury. Another systematic review on the cost of pressure injury prevention and treatment in an adult population [12] reported that the costs of pressure injury prevention per patient per day was in the range of EUR 2.65 (USD 2.64) to EUR 87.57 (USD 85.11), with treatments per patient per day between EUR 1.71 (USD 1.7) and EUR 470 (USD 467.49). The authors warned of heterogeneity among the methods used and found differences in the perspectives and costs included. Finally, a cost modeling study from Australia found that the annual costs to the hospital sector for pressure injuries was AUD 1.6 billion (US 1.03 billion) and AUD 14 million (USD 9 million) in the residential care setting. The vast majority of hospital costs were attributed to excess bed-days to treat serious pressure injuries at stage 3 or 4 [13].
Different analytic methods are used to assess the excess length of stay and costs of health care-acquired events such as pressure injury [14-16]. One challenge in the analysis is that length of stay as an outcome is generally characterized by skewed distributions [17, 18]. Another challenge is that pressure injury is a time-varying exposure that can arise at any point during hospital admission [19-22]. We propose that the extent to which the analytic method chosen can accommodate these challenges will have a large impact on the conclusions. A range of factors other than pressure injury are thought to explain variation in the length of stay, particularly the presence of health care-acquired infection and other adverse events, other admissions during the previous 12 months, age, multiple comorbidities, fecal incontinence, and use of a feeding tube [10].
There are two distinct but complementary objectives of this paper. The first is to report data on the incidence of health care-acquired stage 1 and stage 2 pressure injuries with the aim to shed light on the epidemiology of these events. The second aim is to estimate the impact of these events on length of stay outcomes using competing analytic methods. Our findings will reveal how often stage 1 and stage 2 health care-acquired pressure injuries occur and the costs incurred as determined using bed-days. We demonstrate how much the results vary using different analytic methods and we discuss the merits of different approaches.
2 METHODS
2.1 Setting
The data are from Singapore General Hospital, a tertiary care teaching hospital that provides 20% of the inpatient public beds in Singapore [23]. The hospital provides cardiothoracic surgery, bone marrow transplantation, and solid-organ transplantation and it is the regional referral center for the management of major burns. In 2019, there were a total of 80,817 patients discharged, the emergency department saw 128,660 patients, and there were 724,480 visits to outpatient clinics.
2.2 Data
All admissions to the wards managed by medical and surgical specialty departments of Singapore General Hospital were eligible to be included in a nurse-led monitoring system for pressure injuries. This database has been used for quality improvement over time. The information used in this analysis was from January 2016 to May 2018. Values are available for variables that described the demographic features of patients; the source of injury as either community- or health care-acquired; the clinical specialty department admitting the patient; important dates, such as hospital admission and discharge and staging of the wound; features of the wound, such as stage and dimensions; and, patient risk factors for pressure injury and interventions during admission. Braden scores [24] were also available, which a recent meta-analysis concluded had moderate predictive validity for pressure injury [25]. Braden score assessment was completed by specialized wound nurses, and the responses were added to the data set.
2.3 Data analyses
The main exposure was the presence of stage 1 or 2 pressure injury and the definitions used have been previously published [6]. Monthly incidence rates were calculated for pressure injuries that are categorized as “health care-acquired,” defined as “not present on admission.” Annual incidence rates were estimated by dividing the number of health care-acquired pressure injuries staged during a year by the total admissions to the corresponding hospital wards for that year.
To estimate the excess length of stay arising from pressure injury, a control cohort was identified using the hospital patient information system. Individuals were matched for key variables thought likely to explain variation in the length of stay to create a matched cohort design. The variables used for matching were 5-year age group; sex; admitting specialty, either medical or surgical, and Braden score on admission. The outcome of interest was the length of hospital stay, which was counted as the number of days between the admission date and the discharge date. Continuous variables are summarized as their respective mean and standard deviation and categorical variables are presented using number and percentage.
Four competing methods were used to assess the length of stay and costs for the pressure injury cohort and the control cohort. First, to examine the unadjusted difference in length of hospital stay between the two groups, namely, “cases” versus “controls,” we performed a two-sample t-test on the outcome. Second, multiple variable linear regression was performed on length of stay, with baseline covariates included to account for variation in the outcome. Third, to accommodate skewness in the outcome variable of length of stay, we performed a generalized linear model with gamma distribution and the included baseline covariates. Finally, to account for time-varying exposure of pressure injury, we developed an empirical transition probability matrix based on a simple multi-state model, shown in Figure 1.
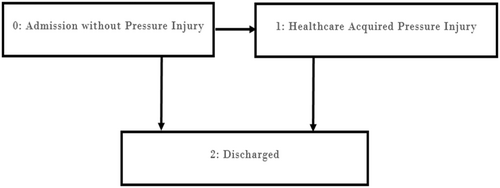
This approach describes a process in which an individual might move from one state to another state over time, and the events are the transitions between states. In this case, there are three states: no pressure injury (assigned 0), pressure injury (assigned 1), and discharge (2). An individual can only move from state 0 to state 1 and then state 2 or from state 0 to state 2 directly. We calculated the transition probabilities using sample proportions from the data (see Appendix B).
We then fitted a Cox proportional hazards model to see the effect of health care-acquired pressure injury on the time to discharge from the hospital. Statistical analysis was performed using R version 3.4.4. These four competing methods were chosen as they are often reported in the literature. These vary in complexity and, to a greater and lesser extent, they address important sources of bias in making estimates for prolonged length of stay.
3 RESULTS
Figure 2 reveals the incidence rates for stage 1 and 2 health care-acquired pressure injuries per 1000 admissions to the hospital for the period 2016−2018.
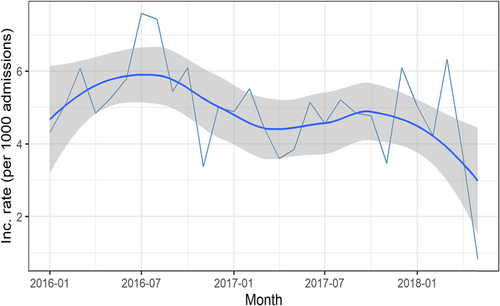
Monthly rates are shown as fluctuating points; the relatively steady line is the trend over time and the 95% CI is shown in gray shading. The incidence rates for 2016 were 0.553% (95% CI 0.55−0.557); for 2017, these were 0.469% (95% CI 0.466−0.472) and for the time in 2018 until 8 May, the rate was 0.181 (95% CI 0.178−0.183). Extrapolating for the rest of 2018 based on the first 127 days gives an annual rate of 0.52%. Nearly all (99.5%) pressure injuries were stage 2.
A total of 9620 patients were included in the two cohorts (Table 1). A total of 1032 individuals developed health care-acquired pressure injury during hospitalization (case cohort) and a total of 8588 patients did not develop any pressure injury (control cohort) during the whole study period. Some observations had incorrect or missing data, and removing these enabled statistical analyses of 809 cases and 8588 controls. There were approximately eight control patients for every patient with a stage 1 or 2 pressure injury. Age, proportion of women, and ethnicity were similar between cohorts. The risk of pressure injury according to Braden score was generally higher for cases, but the proportion “at-risk” was comparable. For age and length of hospital stay, we used a two-sample t-test and for sex, ethnicity, and Braden score, we used a χ2 test.
| Case cohort (n = 1032) | Control cohort (n = 8588) | p Value | |
|---|---|---|---|
| Age (year) (mean ± SD) | 69.09 ± 14.37 | 72.25 ± 14.75 | <0.01 |
| Min = 17 | Min = 24 | ||
| Max = 102 | Max = 106 | ||
| Gender (n %) | <0.01 | ||
| Male | 549 (53.2) | 3897 (45.38) | |
| Female | 483 (46.8) | 4691 (54.62) | |
| Race (n %) | <0.01 | ||
| Chinese | 773 (74.90) | 6686 (77.92) | |
| Indian | 81 (7.85) | 685 (7.98) | |
| Malay | 132 (12.79) | 756 (8.81) | |
| Others | 46 (4.46) | 454 (5.29) | |
| Braden Score (n %) | <0.01 | ||
| No risk | 42 (4.07) | 4194 (48.84) | |
| At risk | 396 (38.37) | 3441 (40.07) | |
| Moderate risk | 324 (31.40) | 540 (6.29) | |
| High risk | 225 (21.80) | 335 (3.90) | |
| Very high risk | 45 (4.36) | 78 (0.91) | |
| Length of hospital stay (days) (mean ± SD) | 48.72 ± 58.03 | 35.53 ± 64.02 | <0.01 |
| Min = 2 | Min = 1 | ||
| Max = 535 | Max = 507 |
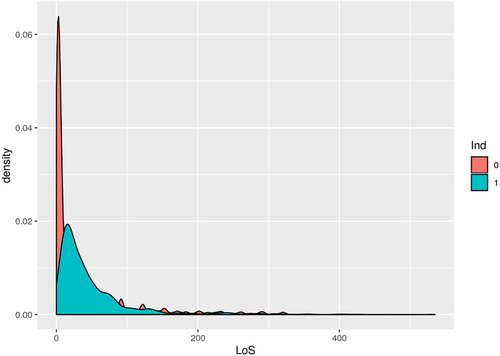
The distributions of the outcome variable length of stay are shown in Appendix A. Owing to the very long tails of length of stay more than 500 days for the outcome variable, we performed sensitivity analyses informed by censoring at different maximum lengths of stay. All analyses were subsequently conducted for patients with maximum lengths of stay less than 30, 60, 100, 200, and 300 days; an analysis of uncensored data is shown. Table 2 shows the impact of this censoring on the number of cases and controls included in the analysis and the results of an unadjusted comparison between cases and controls.
| Where censoring occurs | Number of cases | Number of controls | Difference in days length of stay, cases less controls, mean (95% CI) |
|---|---|---|---|
| 30 days | 359 | 6182 | 10.22 (9.49−10.97) |
| 60 days | 588 | 6803 | 17.68 (16.43−18.93) |
| 100 days | 706 | 7546 | 19.41 (17.60−21.23) |
| 200 days | 775 | 8181 | 18.40 (15.65−21.15) |
| 300 days | 799 | 8515 | 15.95 (12.22−19.67) |
| no censoring | 809 | 8581 | 17.80 (13.28−22.32) |
- Abbreviations: CI, confidence interval; SD, standard deviation.
The results of multiple linear regression on length of stay with model covariates are shown in Table 3.
| Regression coefficients (SE) | ||||||
|---|---|---|---|---|---|---|
| Covariate | 30 days | 60 days | 100 days | 200 days | 300 days | No censoring |
| Age | 0.03 (0.005)* | −0.01 (0.01) | −0.03 (0.02) | −0.03 (0.03) | −0.06 (0.04) | −0.06 (0.05) |
| Gender | 0.19 (0.137) | 0.13 (0.27) | −0.13 (0.51) | −0.99 (0.87) | −2.81 (1.22)* | −2.57 (1.33) |
| Braden Score | −0.37 (0.024)* | −0.46 (0.05)* | −0.54 (0.09) | −1.06 (0.16) | −1.31 (0.22)* | −1.37 (0.28)* |
| Pressure Injury | 8.76 (0.317)* | 15.73 (0.5)* | 16.97 (0.99) | 13.82 (1.69) | 10.45 (2.36)* | 12.03 (2.58)* |
| Race | 0.5 (0.255)* | 0.52 (0.6) | 0.91 (0.95) | 1.09 (1.62) | 1.02 (2.26) | 2.13 (2.47) |
- * Indicates p < 0.05.
- Abbreviation: SE,standard error.
The largest estimate of excess days (12.03 days) was when no censoring was done and the smallest estimate (8.76 days) was when the data were censored at 30 days' duration of admission.
The results of the generalized linear model with a gamma distribution that included the available covariate information are shown in Table 4. We reported adjusted rate ratios for each individual covariate with their respective standard errors.
| Regression coefficients (SE) | ||||||
|---|---|---|---|---|---|---|
| Adjusted rate ratio | 30 days | 60 days | 100 days | 200 days | 300 days | No censoring |
| Age | 1.00 (0.001)* | 0.99 (0.001) | 0.99 (0.001) | 1 (0.001) | 0.99 (0.001) | 0.99 (0.001) |
| Gender | 1.03 (0.027) | 0.99 (0.031) | 0.97 (0.033) | 0.96 (0.03) | 0.92 (0.033) | 0.93 (0.035) |
| Braden Score | 0.93 (0.004)* | 0.94 (0.005)* | 0.97 (0.006)* | 0.96 (0.006) | 0.96 (0.006) | 0.96 (0.006)* |
| pressure injury | 2.37 (0.141)* | 2.56 (0.159)* | 1.99 (0.130)* | 1.47 (0.09) | 1.26 (0.089) | 1.29 (0.092)* |
| Race | 1.07 (0.051) | 1.06 (0.075) | 1.06 (0.066) | 1.06 (0.07) | 1.04 (0.07) | 1.05 (0.07) |
- * Indicates p < 0.05.
- Abbreviation: SE,standard error.
The findings revealed that the presence of pressure injury for the “censored at 30 days” analysis increased the length of stay by 2.37 times. According to this finding, in Table 5, we report the mean length of stay for controls and cases and show the expected difference in length of stay owing to the presence of pressure injury.
| 30 days | 60 days | 100 days | 200 days | 300 days | No censoring | |
|---|---|---|---|---|---|---|
| Mean Length of stay for controls | 5.24 | 8.22 | 14.80 | 24.69 | 33.28 | 35.51 |
| Mean Length of stay cases | 12.42 | 19.48 | 35.08 | 58.52 | 78.87 | 84.16 |
| Difference in Length of stay (95% CI) | 7.18 (7.13−7.23) | 11.26 (10.7−11.82) | 20.28 (19.26−21.29) | 33.83 (32.12−35.52) | 45.59 (43.31−47.87) | 48.65 (46.22−51.08) |
- Abbreviation: CI, confidence interval.
The results of the multi-state model are presented in Table 6. We report the excess length of stay for pressure injury and the hazard rates for remaining in the pressure injury state and not being discharged, after adjusting all baseline covariates like age, sex, ethnicity, and Braden score. Health care-acquired pressure injury decreases the hazard of discharge for all censored data.
| 30 days | 60 days | 100 days | 200 days | 300 days | No censoring | |
|---|---|---|---|---|---|---|
| Excess Length of stay for pressure injury (95% CI) | −0.68 (−1.38 to 0.01) | 1.22 (0.19−2.23) | 9.95 (8.77−11.13) | 23.41 (21.58−25.24) | 35.24 (32.37−38.12) | 36.22 (32.42−40.01) |
| Adjusted HR (95% CI) | 0.27 (0.24−0.31) | 0.29 (0.26−0.31) | 0.36 (0.33−0.39) | 0.42 (0.39−0.45) | 0.44 (0.40−0.47) | 0.43 (0.4−0.47) |
- Abbreviations: CI, confidence interval; HR, hazard ratio.
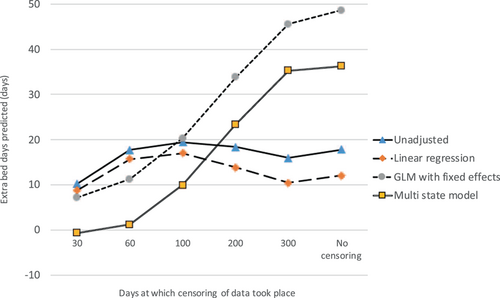
We present a graphical summary of all findings in Figure 3.
4 DISCUSSION
We show that stage 1 or 2 health care-acquired pressure injury occurred in approximately 0.5% of all newly admitted patients. The only other estimate of incidence rates for less serious health care-associated pressure injuries was published in 1999 in the United States [8] and revealed rates of 3.1% for stage 1% and 3.2% for stage 2. It is plausible that rates of all health care-associated pressure injuries have declined since then, given the increased awareness for patient safety and quality of services; our results support this.
Excess length of stay and cost outcomes were heterogeneous and varied according to the point at which individuals were censored and the analytic method used to estimate the outcome. The “unadjusted comparison of cases against controls” and the “linear regression” results followed a similar pattern as the censoring changes. Estimates of excess length of stay initially increased as more patients with long stays were included; the estimates of excess stay were then somewhat reduced. The findings revealed that the maximum difference between cases and controls in terms of length of stay arose when patients were censored at 100 days' stay in the hospital. We suspect that very long patient stays were owing to social issues, such as having no suitable place of discharge so patients remained in the hospital for an extended time. The characteristics of patients with long stays are central to these analyses. It is likely that social determinants and other underlying diseases were potentially influential; not having this information included in the analyses is a study limitation.
We are confident that pressure injury is not the cause of very long stays. These results are likely not useful as they fail to address the two major challenges in the data, namely, that length of stay is an outcome generally characterized by skewed distributions, and that pressure injury is a time-varying exposure that can arise at any point during hospital admission.
The gamma GLM method that accommodates skewness in the data showed that excess stay owing to pressure injury occurred more frequently as more long-staying patients were included. However, at each point, these estimates comfortably exceeded findings from the multi-state model. Use of the multi-state model is the best approach to estimating this outcome as it appropriately captures the timing of the onset of pressure injury. This method explicitly addresses both time and length bias that affect estimates of excess stay owing to time-varying exposures [19-22]. For these reasons, we suggest that results from the multi-state model are the most likely to be valid. Yet the estimates reported are between 0 excess days for 30 days' censoring and 36 days when the entire set of information is used.
As the censoring was relaxed, more patients were included in the analysis and the chance of bias from selecting outpatients owing to their long stays in the hospital was reduced. This is a positive feature, yet there might be problems with not censoring these data. By including patients with long stays, such as those with stays over 100 days, there is a good chance that we are observing patients who do not need to be in the hospital for acute care. Indeed, we believe that many long-stay patients are simply unable to be discharged to the community because they cannot care for themselves at home and no places are available in a residential care facility. Hence, these patients become long-term residents in an acute care hospital.
With this in mind, we focused on findings from the multi-state model for patients whose stay did not exceed 60 days. We observed an excess stay of 1.22 days (95% CI 0.19−2.23), which is plausible and makes clinical sense. Stage 1 and 2 pressure injuries are not very serious and can be managed with standard techniques and good quality care; assigning an excess stay of 1.22 days is a reasonable outcome. The clinical team might monitor a stage 1 or 2 injury or provide some simple education to patients and their families to reduce the chance of the injury becoming worse after discharge.
The potential for large bias from other analytic methods is obvious. For 60-day censoring, the unadjusted comparison was 17.68 days; linear regression yielded 15.73 days and the gamma GLM model yielded 11.62 days. It is difficult to understand how any of these results are plausibly caused by the treatment and health burdens from stage 1 or 2 pressure injuries. Another consideration is the direction of causality between the risk of pressure injury and length of stay. Prolonged stays have been shown to increase the risk of other health care-associated complications, such as infection [26]. Additionally, any endogenous relationship could violate a requirement of the linear models [27]. However, the use of state-based models has been shown to reduce the associated biases of time and length of stay [28].
With 0.5% of admitted patients experiencing these events, the potential for this problem to be costly in terms of added bed-days at system level is considerable. The utility of these findings is that programs designed to reduce the risk of pressure injury can claim a cost savings in terms of bed-days saved. This information can be synthesized for economic evaluation or cost-effectiveness models designed to improve the allocation of scarce resources for health services. Using inflated or biased estimates will either dissuade decision makers if they do not believe the proposed cost savings are real or they will lead to an inappropriately large investment in risk-reducing programs.
To monetize any of the present results requires a cost estimate for each bed-day in the Singapore health system; the best estimate identified was SGD 823 (95% CI USD 817–USD 829) per bed-day [29]. Simply multiplying the number of bed-days by this estimate will provide some indication of the monetary costs, but care should be taken when interpreting costs that emerge from accounting methods as they are unlikely to reflect economic opportunity costs of the resources used in providing the bed-days [30].
There are further limitations to this study. The data are retrospective and arose from a nursing-led monitoring system that collects information from electronic medical records. We cannot rule out issues such as under-reporting, data accuracy, and incorrect wound staging, which may reduce the reliability and validity of the data analyzed. However, wound nurses usually assess and grade pressure injuries so the data are likely to be reliable. There was also a limited set of control variables available for the analysis, and more information that correlates with variation in length of stay outcomes may have led to lower estimates of excess length of stay.
Future research should model the expected change in total costs and health benefits arising from additional programs that reduce the risk of health care-acquired stage 1 and 2 pressure injuries.
5 CONCLUSION
We conclude that stage 1 and 2 pressure injuries are quite common and increase costs. There may be modest value to investing in prevention programs. Using biased estimates of excess length of stay will overstate the potential value of prevention. We therefore recommend that appropriate statistical methods be used to accurately attribute the cost outcomes to pressure injuries.
AUTHOR CONTRIBUTIONS
Nicholas Graves and Raju Maiti devised the methods and conducted the analyses. Fazila Abu Bakar Aloweni and Ang Shin Yuh provided data and expert advice. Ng Yi Zhen and Priya Bishnoi provided wound-specific inputs for the analyses. Tze Tec Chong, David Carmody, and Keith Harding provided clinical interpretations. All authors drafted and reviewed the manuscript.
ACKNOWLEDGMENTS
The Wound Care Innovation for the Tropics (WCIT) Program and Wound Care Registry teams supported this work. This research is supported by the Agency for Science, Technology and Research (A*STAR) under its Industry Alignment Fund—Pre-Positioning Program (IAF-PP) grant number H1X/01/a0/OX9 as part of the Wound Care Innovation for the Tropics (WCIT) Program.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
Submission was made to the SINGHEALTH CENTRALISED INSTITUTIONAL REVIEW BOARD (CIRB) (CIRB ref no: 2019-2954). The decision was that the application did not require further ethical deliberation as the study used deidentified data. This study was exempted by the NUS Institutional Review Board (NUS-IRB) (NUS human ethics ref: LN-20-029E). The Occurrences and Costs of Chronic Wounds in Singapore: The review board noted that the research participants cannot be identified, directly or through identifiers linked to the research participants.
INFORMED CONSENT
The need for consent by participants was therefore waived by each ethics board. Group Chief Nurse, A/Prof Tracy Carol Ayre gave approval to use the data for this project. All methods were carried out in accordance with relevant guidelines and regulations
APPENDIX A
Figure A1.
APPENDIX B
| From\to | 0 | 1 | 2 |
|---|---|---|---|
| 0 | 0 | 0.086 | 0.914 |
| 1 | 0 | 0 | 1 |
| 2 | 0 | 0 | 0 |
- Note: From means from state i to means to state j.
- Abbreviation: LoS, length of stay (days).
| Item No | Recommendation | ||
|---|---|---|---|
| Title and abstract | 1 | (a) Indicate the study's design with a commonly used term in the title or the abstract | Title page |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | P1 | ||
| Introduction | |||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | P2&3 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | P3 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper | P4&5 |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | P4 |
| Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up | P4 |
| (b) For matched studies, give matching criteria and number of exposed and unexposed | P5 | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | Tables 1−6 |
| Data sources/measurement | 8a | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | P4&5 Table 1 |
| Bias | 9 | Describe any efforts to address potential sources of bias | P4−6 |
| Study size | 10 | Explain how the study size was arrived at | P4 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | P4−6 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | P4&5 |
| (b) Describe any methods used to examine subgroups and interactions | N/a | ||
| (c) Explain how missing data were addressed | P7 | ||
| (d) If applicable, explain how loss to follow-up was addressed | N/a | ||
| (e) Describe any sensitivity analyses | P8 | ||
| Results Participants | |||
| 13a | (a) Report numbers of individuals at each stage of study—for example, numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed | P7 | |
| (b) Give reasons for nonparticipation at each stage | P7 | ||
| (c) Consider use of a flow diagram | N/a | ||
| Descriptive data | 14a | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | Table 1 |
| (b) Indicate number of participants with missing data for each variable of interest | P7 | ||
| (c) Summarize follow-up time (e.g., average and total amount) | P6&7 | ||
| Outcome data | 15a | Report numbers of outcome events or summary measures over time | Figure 2 |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95% confidence interval). Make clear which confounders were adjusted for and why they were included | Tables 2−6 |
| (b) Report category boundaries when continuous variables were categorized | N/a | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | N/a | ||
| Other analyses | 17 | Report other analyses done—for example, analyses of subgroups and interactions, and sensitivity analyses | Table 2−6 |
| Discussion | |||
| Key results | 18 | Summarize key results with reference to study objectives | P11 |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | P12−14 |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | P14 |
| Generalizability | 21 | Discuss the generalizability (external validity) of the study results | P14 |
| Other information | |||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | P14 |
- Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available at http://www.plosmedicine.org/, http://www.annals.org/, and http://www.epidem.com/). Information on the STROBE Initiative is available at http://www.strobe-statement.org.
- a Information provided separately for exposed and unexposed groups.
Open Research
DATA AVAILABILITY STATEMENT
The datasets generated and/or analyzed during the current study are not publicly available owing to preferences of the data custodians. The data were collected for internal audit purposes by the hospital and we obtained permission to use the data for research purposes, but we did not obtain permission to share these data publicly. The hospital does not wish to release audit data for public consumption. Research data are not shared.




