Emergence of SARS-CoV-2 variants KP.2 and KP.3 sparks concerns: What should we do?
Graphical Abstract
SARS-CoV-2 continues to evolve and circulate globally. In recent weeks, variants such as KP.2 and KP.3 have been rapidly increasing in many countries. Prevention strategies such as receiving updated COVID-19 vaccines, wearing masks when recommended, washing hands frequently, getting tested if symptoms appear, and staying home when sick can help protect individuals and others from COVID-19.
Abbreviations
-
- COVID-19
-
- Coronavirus disease 2019
-
- INSACOG
-
- Indian SARS-CoV-2 Genomics Consortium
-
- SARS-CoV-2
-
- Severe acute respiratory syndrome coronavirus 2
-
- USA
-
- the United States of America
-
- WHO
-
- World Health Organization
1 INTRODUCTION
The first case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported in Wuhan, China, in December 2019. The virus spread worldwide within a few weeks of its outbreak, resulting in coronavirus disease (COVID-19) [1, 2]. In March 2020, the World Health Organization (WHO) declared the COVID-19 outbreak, a global pandemic. The pandemic has killed half a million people in India and close to 7 million globally (accessed https://data.who.int/dashboards/covid19/cases on May 24, 2024) [3]. The COVID-19 pandemic has had profound global impacts on health systems, economies, and societies, leading to disruptions in healthcare services, education, travel, and daily life. SARS-CoV-2 serves as a reminder of the interconnectedness of global health and the importance of robust public health infrastructure, international cooperation, and preparedness in combating infectious diseases in this century [4].
2 EMERGING VARIANTS
SARS-CoV-2 has undergone genetic changes and continues to evolve, leading to the emergence of new variants with increased severity and potential evasion of immunity [5, 6]. The WHO is currently tracking several SARS-CoV-2 variants and has classified them as variants of concern, variants of interest, and variants under monitoring [7]. While many variants do not necessarily increase the severity of COVID-19 illness, some have been associated with high disease severity or increased risk of hospitalization. For example, the delta variant has been noted for causing more severe illness compared to earlier strains [8]. The latest addition to the global COVID-19 variants list is KP.2 and KP.3, which are the descendants of JN.1 that gained attention in 2024. WHO declared it as “variants under monitoring” on May 3, 2024 [7, 9]. SARS-CoV-2 KP.2 variant, bearing mutation S: R346T, S:F456L and S:V1104L, has been reported in 38 countries, with cases in India, United Kingdom, Canada, Singapore, Australia and the United States of America [10]. The KP.2 variant was responsible for the increasing number of cases in multiple regions in April/May 2024 and became a predominant variant in the USA [11]. KP.2 variant made up just 4% of infections in late March 2024 but was responsible for over 28% as of May 24, 2024, marking a significant shift and highlighting the need for continued vigilance [12, 13]. Singapore reported a surge in the number of cases, with over 25,900 cases reported in 1 week (May 5 to May 11, 2024). More than two-thirds of COVID-19 cases in Singapore are attributed to the KP.1 and KP.2 variants. As of now, no travel restrictions or mandatory testing requirements have been imposed. However, the Singapore Ministry of Health advises wearing masks, practicing good hygiene, and maintaining social distance [14]. According to the Indian SARS-CoV-2 Genomics Consortium (INSACOG) data, India has confirmed 299 cases of the KP.2 variant in several states, with the numbers of the cases growing every day. As of June 22, 2024, Maharashtra reported the highest number of cases (156), followed by West Bengal (36), Gujarat (23), Rajasthan (21), Odisha (17), Uttarakhand (17), Goa (12), Uttar Pradesh (8), Karnataka (4), Haryana (3), and one each in Delhi and Madhya Pradesh [15].
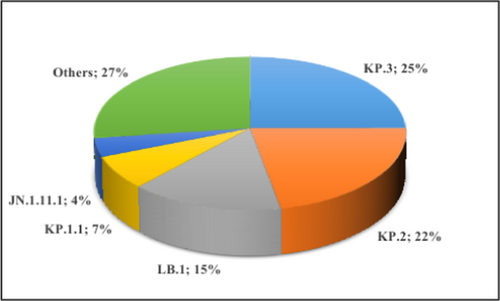
Recently, KP.3, bearing mutation S: F456L, S: Q493E and S: V1104L, has rapidly spread and overtaken KP.2 within weeks, becoming the most prevalent strain in the USA (as of June 20, 2024). KP.3 now represents approximately 25% of cases in the USA, up from about 9% in early May. Following KP.3, the next most prevalent variant is KP.2, which now constitutes around 22% of cases (Figure 1) [7, 12]. This variant has been detected in at least 29 countries [10]. India has confirmed 69 cases of the KP.3 variant so far (INSACOG data as of June 20, 2024) [15]. Thus far, affected individuals have not exhibited any unusual symptoms. The symptoms resemble typical COVID-19 symptoms similar to those reported in other variants of the virus.
3 KP.2 AND KP.3: COULD IT BE THREAT?
Unfortunately, preliminary evidence indicates an increased immune resistance ability in the KP.2 variant. However, the data on KP.2 and KP.3 are still very limited, limiting the conclusions that can be drawn [16]. While KP.2 and KP.3 transmissibility is concerning, these variants seem to cause milder illness so far. However, research is warranted to determine the vaccine efficacy of currently available vaccines against these emerging variants. It is expected that these variants might cause a surge in the number of cases in the coming months; however, no major hospitalization, unusual symptoms, high severity, or death have been reported until now. Unvaccinated groups, immunocompromised individuals, and elderly people are most vulnerable to severe infection. Staying up to date with vaccination could reduce the disease severity and lower the risk of hospitalization and death [17]. Currently, there is no evidence to prove that these variants are more likely to cause severe disease or mortality, and scientists are studying cases to understand this better. It is not uncommon for viruses to mutate; SARS-CoV-2 is no exception. There is considerable uncertainty about the emergence of new SARS-CoV-2 variants. There is a possibility that new variants will continue to emerge, which could potentially make vaccines less effective or cause more severe infection. We have seen SARS-CoV-2 variants outcompete each other and become dominant earlier as well during the pandemic. The delta variant outcompeted all the other variants in May 2021; then omicron outcompeted delta in early 2022 [18, 19]. Given the uncertainty, countries should ensure resilience by upholding contingency capabilities to address various potential scenarios.
The approach to control SARS-CoV-2 transmission is the same, regardless of the variant. Vaccines are crucial for providing good protection against severe disease and hospitalization associated with emerging variants [20]. Though vaccines do not offer complete protection against emerging new variants, they are the best line of defense. The administration of booster doses could provide better protection. Currently, most of the population has stronger protection due to vaccination campaigns, immunity through natural infection, and access to antivirals [21]. The rising immunity levels will likely prevent the serious illness caused by the emerging variants among communities. Those at high risk and most vulnerable to COVID-19 should get eligible booster doses [17]. Monitoring vaccine effectiveness is vital for SARS-CoV-2 variants surveillance. Global and local governments should ensure the equitable access to updated COVID-19 vaccines to all nations to reduce the risk of the emergence of new variants [22]. Furthermore, global authorities should closely track emerging variants and monitor the situation to avoid case upsurges and COVID-19 waves globally. Researchers should investigate the potential for immune escape (the ability of the pathogen to evade the immunogenic response of a host) of new variants and understand their evolution. It is essential to maintain vigilance and multi-sectoral collaboration to navigate this challenge effectively.
4 PUBLIC HEALTH RESPONSE AND RECOMMENDATIONS
Preventing the spread of SARS-CoV-2 variants requires a multifaceted approach that combines public health measures, surveillance, vaccination strategies, and international cooperation [23]. State and central governments should invest in robust genomic surveillance programs to monitor the emergence of new SARS-CoV-2 variants by regularly sequencing infected samples to detect the mutations that may affect the virus's characteristics. Regular data sharing through international collaboration among the public health departments helps track the global circulation of variants. Implementing rapid public health response to new variants, including contact tracing, updating diagnostic kits, adjusting vaccine antigen composition, accelerating vaccination campaigns, and administering booster doses for vulnerable populations, enhances immunity, particularly against emerging variants. Furthermore, reinforcing public health measures such as mask mandates and improving ventilation in indoor spaces remains critical. These measures could help mitigate the transmission risks, particularly in settings where variants could circulate more easily or during potential super spreader events.
Coordinated efforts to develop variant-specific vaccines or vaccine modifications to ensure continued efficacy against emerging variants are also critical to mitigate the impact of infections [24]. A new vaccine [25] based on JN.1 or other subvariants is expected to be available this year, offering better protection against circulating and potentially emerging variants. All countries and international organizations should ensure vaccine equity for new vaccines by implementing fair distribution based on public health needs [26]. By implementing these policy recommendations, governments and health authorities could effectively mitigate the spread of emerging SARS-CoV-2 variants, reduce the burden on healthcare systems, and protect global public health. Adaptation and flexibility in response strategies will be crucial as the virus continues to evolve, ensuring that interventions remain effective against emerging variants.
5 CONCLUSION
In conclusion, to prevent and control the spread of new variants, it is essential for the public to comply with the precautionary measures and statutory warnings issued by government authorities. Following safer behaviors such as getting vaccinated, wearing a face mask in crowded places, staying home if unwell, and practicing good hygiene can reduce the risk of infection [27]. Overall, effective preparedness against new variants requires a combination of proactive measures such as strengthening surveillance, real-time transparent data sharing, risk assessment, capacity building, vaccination strategies, updating vaccine antigen composition for increased effectiveness against circulating strains, and adhering to preventive measures can help mitigate its impact on public health.
AUTHOR CONTRIBUTION
Balamurugan Shanmugaraj: Conceptualization (lead); Data curation (lead); Investigation (lead); Writing—original draft (lead); Writing—review & editing (lead).
ACKNOWLEDGMENTS
The author is very thankful to Karpagam Academy of Higher Education for the support.
CONFLICT OF INTEREST STATEMENT
The author declares no conflict of interest.
ETHICS STATEMENT
Not applicable.
INFORMED CONSENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable – no new data generated.