TLR2 signaling improves immunoregulation to prevent type 1 diabetes
Abstract
Signaling through TLR2 promotes inflammation and modulates CD4+CD25+ Tregs. We assessed mechanistically how this molecule would alter immunoregulation in type 1 diabetes (T1D). We also asked whether TLR2 may be involved in our recent discovery that viral infection can protect from autoimmune diabetes by expanding and invigorating Tregs. Treatment of prediabetic mice with a synthetic TLR2 agonist diminished T1D and increased the number and function of CD4+CD25+ Tregs, also conferring DCs with tolerogenic properties. TLR2 ligation also promoted the expansion of Tregs upon culture with DCs and ameliorated their capacity to prevent the disease. Protection from T1D by lymphocytic choriomeningitis virus (LCMV) infection depended on TLR2. LCMV increased the frequency of CD4+CD25+ Tregs and their production of TGF-β more significantly in WT than TLR2-deficient mice. Furthermore, LCMV infection in vivo or LCMV-infected DCs in vitro rendered, via TLR2, CD4+CD25+ Tregs capable of diminishing T1D. We identify novel mechanisms by which TLR2 promotes immunoregulation and controls autoimmune diabetes in naïve or infected hosts. This work should help understand T1D etiology and develop novel immune-based therapeutic interventions.
Introduction
Type 1 diabetes (T1D) is a genetic disease resulting in the destruction of insulin-producing β cells by autoreactive T cells in the pancreatic islets of Langerhans 1. The importance of additional environmental factors such as infections in the development of this disease has long been reported, but to date whether and how these might trigger or prevent T1D is not understood 2. It has been proposed that the inflammatory events induced upon anti-infectious immunity enable enhanced presentation of β-cell antigens to autoreactive T cells. Pro-inflammatory cytokines cause the up-regulation of class I MHC molecules on β cells, and may thereby “unmask” them for recognition by CD8+ T cells 3. In addition, concomitant damage to β cells and activation of APCs by the infection may promote the presentation of β-cell antigens to CD8+ T cells. This has notably been demonstrated in NOD mice using Coxsackievirus B4 4, or in RIP-LCMV mice, which transgenically express lymphocytic choriomeningitis virus (LCMV) antigens on their β cells and develop autoimmune diabetes following LCMV infection 5-7. Inflammatory signals not only promote DC and T-cell activation but might also directly cause β-cell destruction 8-10, therefore strongly contributing to T1D development.
On the other hand, studies in humans and mice suggest that infections and inflammation might play a protective role in T1D; notably, disease can be prevented in NOD mice by infection with a number of viruses 2. Antiviral immunity may increase resistance to diabetogenic infections or “distract” the immune system from their detrimental effect 11. In addition, as we reported recently 12, viral infections may shape the immune system such that diabetogenic T cells are impaired or kept under control by immunoregulatory mechanisms. We found that viral infection triggered the expansion of invigorated CD4+CD25+ Tregs that produced TGF-β and protected from autoimmune diabetes by synergizing with programmed death-ligand 1 (PD-L1). These findings indicated a beneficial role of virally induced inflammation in T1D. A number of studies in mice have underscored the capacity of pro-inflammatory agents to prevent rather than induce T1D when intervening in the absence of β-cell damage and autoantigen 13.
TLRs are usually referred to as “danger-sensing” molecules that play a central part in triggering inflammation and immunity in response to infection 14. Different TLRs, each recognizing specific molecular patterns, have been identified in humans and mice. Binding of cognate ligands to TLRs on professional APCs such as DCs triggers signaling pathways that lead notably to the production of inflammatory cytokines 15. In this way, TLR signaling might promote the development of autoimmunity. For instance, both TLR3 16 and TLR9 17 signaling can cause T1D when triggered in the presence of β-cell antigens. Similarly, TLR2 has been shown to cause APC activation upon binding to byproducts of late apoptotic β cells, and thereby contribute to the initiation of autoimmune responses in T1D 18. TLR2 binds to molecular motifs present in LPS, peptidoglycan, lipoteichoic acid, and lipoproteins/lipopeptides expressed by bacterial or parasitic micro-organisms 19-21. TLR2 also binds to endogenous ligands, such as HSP60 22 and possibly other self-antigens present within secondary necrotic cells 18 or released during antiviral immunity 23. Importantly, activation of TLR signaling is not systematically causative for T1D, as treatment with compounds that trigger TLR2 24, TLR3 25, TLR4 26, or TLR9 27 signaling, when given in the absence of β-cell antigen, has a preventive effect in autoimmune diabetes. Interestingly, previous work has shown that CD4+CD25+ Tregs, which play a crucial role in the prevention of autoimmunity, not only express different TLRs, including TLR2 28-30, but are also functionally regulated directly and indirectly through TLR signaling 31. Exposure of Tregs to LPS induces their activation and enables them to control T-cell-mediated wasting disease 28. In addition, while binding to TLR2 by endogenous antigens causes APC activation and promotes T1D 18, it was also reported to enhance the function of CD4+CD25+ Tregs 22. In fact, while activation of TLR2 signaling in CD4+CD25+ Tregs causes a transient loss of their function, it efficiently triggers their expansion 29, 30. A recent study also suggested that TLR2 (and MyD88) was dispensable for development of T1D in NOD mice 32, thereby contrasting with previous work involving this molecule in the initiation of autoimmune responses directed against β cells 18.
Using the NOD and RIP-LCMV mouse models for T1D, we thus assessed the capacity of TLR2 signaling to modulate immune regulation and alter autoimmunity in this disease. Our results indicate a role for TLR2 in enhancing CD4+CD25+ Tregs and DCs, both in a naïve context or during viral infection, to enable protection from autoimmune diabetes. Therefore, while innate pathways such as TLR2 signaling may contribute to the development of autoimmunity when β cells are damaged, they may also promote immunoregulatory mechanisms that counter autoimmune processes and prevent T1D when β cells are spared. The opposing roles of inflammation in T1D may thus be accounted for by the capacity of innate pathways to trigger both immunity (via β-cell damage) and immunoregulation.
Results
Activation of TLR2 signaling during the prediabetic phase diminishes T1D
TLR2 recognizes motifs present in LPS, peptidoglycan, lipoteichoic acid, and lipoproteins/lipopeptides 19-21. We evaluated the effect of a TLR2 agonist, the lipopetide Pam3CSK4 (P3C), on T1D development in NOD mice. P3C was administered intraperitoneally to NOD mice, twice during the prediabetic phase. We observed that P3C treatment could delay diabetes onset and diminish the incidence of the disease in NOD mice (Fig. 1A). In accordance with this observation, infiltration of the pancreatic islets by immune cells was significantly decreased at 11 and 16 wk of age in P3C-treated compared to naïve NOD mice (Fig. 1B). Of note, additional injections of P3C during the prediabetic phase did not ameliorate the protective effect of P3C on T1D (data not shown). Although the observed effect of P3C was modest, these results suggested that activation of the TLR2 signaling pathway systemically before the onset of T1D could confer some extent of protection from this disease.
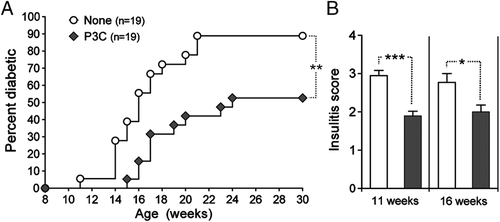
Activation of TLR2 signaling by P3C in prediabetic NOD mice diminishes T1D. (A) Cumulative diabetes incidence over time in NOD mice injected at 9 wk of age with either saline (None, white circles) or 100 μg P3C twice at 5-day intervals (P3C, black diamonds), combined from two independent studies. **p<0.005, determined using a logrank test. (B) Insulitis scoring of pancreatic islets (Mean+SEM of n=5 mice per group) from naïve (None, white bars) and P3C-treated (P3C, black bars) mice at 11 and 16 wk of age. *p<0.05, ***p<0.001, determined using an unpaired, two-tailed t-test.
TLR2 signaling in vivo increases CD4+CD25+ Treg numbers and ameliorates their tolerogenic property in T1D
We evaluated whether the capacity of P3C treatment to diminish autoimmune diabetes might be conferred by enhanced CD4+CD25+ Tregs. We treated prediabetic NOD mice with P3C and measured 21 days later the frequency and function of these cells in the pancreatic LN and spleen. We found that injection of P3C induced an increase in the percentage of CD4+CD25+ T cells in these lymphoid organs (Fig. 2A). The vast majority of CD4+CD25+ T cells expressed Foxp3 along with low levels of CD127 (Fig. 2B), indicating that they were indeed Tregs 33, 34. Consequently, the frequency of CD4+Foxp3+ T cells was also increased in the pancreatic LN and spleen of P3C-treated mice (data not shown). In order to determine whether the protective effect of P3C treatment also involved an enhancement of Treg function, we monitored diabetes development in NOD mice adoptively transferred with CD4+CD25+ T cells purified from P3C-treated donors. We found that P3C treatment conferred Tregs with the capacity to diminish the incidence of diabetes in these mice (Fig. 2C). These observations suggested that stimulation of the TLR2 signaling pathway in vivo could increase the frequency and ameliorate the tolerogenic function of CD4+CD25+ Tregs in spontaneous T1D, in a fashion comparable to viral infection 12.
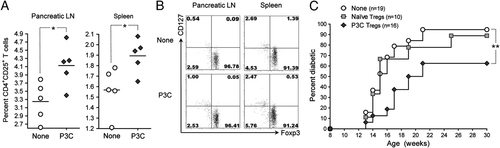
Activation of TLR2 signaling by P3C in prediabetic NOD mice increases the frequency of CD4+CD25+ Tregs and confers them with protective capacity in T1D. (A) Percentage of CD4+CD25+ T cells in the pancreatic LN and spleen of 12-wk-old NOD mice injected 21 days prior with either saline (None, white circles) or 100 μg P3C (P3C, black diamonds) twice at 5-day intervals, measured by flow cytometry. Each symbol represents one mouse; horizontal bar indicates the mean. *p<0.05, determined using an unpaired, two-tailed t-test. (B) Representative flow cytometry dot plots of Foxp3 and CD127 expression by CD4+CD25+ T cells in the pancreatic LN and spleen of individual 12-wk-old NOD mice left untreated (None) or injected 21 days prior with 100 μg P3C twice at 5-day intervals. Quadrants were defined based on isotype control stainings showing under 0.2% positive cells for each parameter analyzed. Numbers indicate the percentage of cells in the corresponding quadrants. (C) Cumulative diabetes incidence over time in NOD mice left untreated (None, white circles) or injected at 12 wk of age with 106 CD4+CD25+ Tregs purified from age-matched NOD donors injected at 9 wk of age with either saline (Naïve Tregs, gray squares) or 100 μg P3C twice at 5-day intervals (P3C Tregs, black diamonds). **p<0.005, determined using a logrank test.
Activation of TLR2 signaling in vivo confers DCs with the capacity to protect from T1D
Since DCs constitute the principal immune cell type expressing TLRs, we assessed whether stimulation of these cells through the TLR2 pathway might be able to confer them with protective function in autoimmune diabetes in vivo. We treated 9-wk-old NOD mice with P3C, and purified their DCs from the LNs 15 h later. Treatment of prediabetic mice with P3C caused the up-regulation of MHC class II but not CD80, CD86, or CD40 on the surface of DCs (Fig. 3A). While we were unable to detect cytokine production by DCs from P3C-treated mice ex vivo, we found that their exposure to P3C in vitro led to increased production of the pro-inflammatory cytokines IL-6, but also of the immunoregulatory cytokine IL-10 (Supporting Information Fig. 1A). We then adoptively transferred DCs from P3C-treated mice into age-matched, prediabetic NOD mice. We found that DCs from P3C-treated donors significantly reduced diabetes by both delaying the onset of overt disease and diminishing disease incidence, while DCs from naïve mice only had a limited effect on the disease (Fig. 3B). These observations suggested that activation of the TLR2 signaling pathway conferred DCs the ability to diminish T1D in vivo.
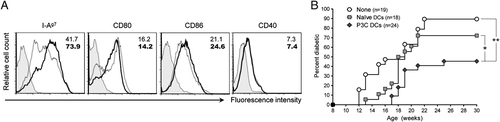
Activation of TLR2 signaling by P3C in prediabetic NOD mice confers DCs with protective capacity in T1D. (A) Flow cytometry histogram plots of I-Ag7, CD80, CD86, and CD40 expression by CD11c+ cells purified from 9-wk-old NOD mice left untreated (gray dotted lines) or injected 15 h prior with 100 μg P3C (black solid lines) (12 pooled mice per group). Filled histograms represent isotype control staining. Numbers indicate the MFI of the parameter analyzed. (B) Cumulative diabetes incidence over time in NOD mice left untreated (None, white circles) or injected at 9 wk of age with 106 CD11c+ cells purified from age-matched NOD mice injected 15 h prior with either saline (Naïve DCs, gray squares) or 100 μg P3C (P3C DCs, black diamonds), combined from two independent studies. *p<0.05, **p<0.005, determined using a logrank test.
CD4+CD25+ Tregs cultured with DCs and a TLR2 agonist efficiently protect from T1D
DCs play a crucial part in activating not only effector T cells, but also Tregs, and previous work has shown that CD4+CD25+ Tregs can be expanded with DCs in vitro and used to treat autoimmune diabetes in vivo 35, 36. Based on our results thus far, we assessed whether TLR2-mediated stimulation in vitro might expand Tregs capable of diminishing T1D in vivo. DCs and CD4+CD25+ T cells were purified from 9-wk-old NOD mice and cultured in the presence or absence of P3C. After 6 days, the DCs were depleted from the culture, and the Tregs were counted and their phenotype assessed. CD4+CD25+ Tregs cultured with DCs and stimulated through TLR2 in vitro had expanded five-fold, whereas cells cultured in the absence of P3C showed no expansion in culture (Fig. 4A). Consistent with previous observations by others 29, 30, Foxp3 expression was reduced in TLR2-stimulated Tregs, although not completely lost, and surface expression of CD25 was increased (Fig. 4B), although modestly. Expression of CD127 and most notably PD-L1 was also increased on the surface of P3C-stimulated Tregs. Addition of an anti-CD3 antibody to the culture media further promoted the expansion of the Tregs but did not affect them in terms of expression of Foxp3 or CD127 (data not shown). Interestingly, P3C-mediated expansion of Tregs was associated with IL-10 production and depended on the presence of DCs stimulated through TLR2 (either before or during culture with the Tregs) (Supporting Information Fig. 1). We then assessed the capacity of CD4+CD25+ T cells cultured with DCs and P3C to modulate T1D in vivo. While CD4+CD25+ Tregs cultured with DCs in the absence of P3C could diminish diabetes upon injection into 9-wk-old NOD mice, stimulation through TLR2 significantly ameliorated the tolerogenic function of these cells, which conferred efficient reduction of the disease (Fig. 4C). In sum, exposure of CD4+CD25+ Tregs to DCs stimulated through TLR2 promoted their expansion and markedly increased their tolerogenic function in T1D in vivo.
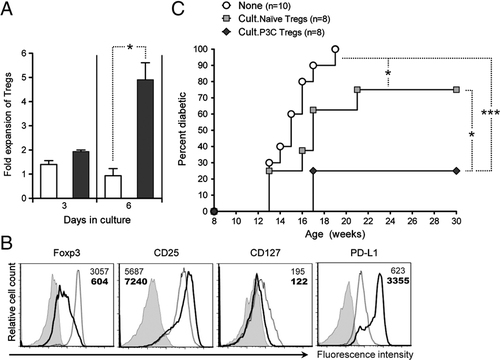
CD4+CD25+ Tregs cultured with DCs and P3C efficiently prevent T1D in NOD mice. CD4+CD25+ T cells were purified from 9-wk-old NOD mice and cultured for 6 days with DCs (CD11c+ cells purified from age-matched, syngeneic mice) and 10 U/mL rhIL-2 in either media alone (Cult.Naïve Tregs) or containing 2 μg/mL P3C (Cult.P3C Tregs). At the end of the culture, the Tregs were separated from the DCs by negative selection of MHC class-II-expressing cells. (A) Fold expansion of CD4+CD25+ T cells over the 6-day culture period in media alone (None, white bars) or containing P3C (black bars) (Mean+SEM from duplicate samples). *p<0.05, determined using an unpaired, two-tailed t-test. (B) Flow cytometry histogram plots of Foxp3, CD25, CD127, and PD-L1 expression by Tregs purified after culture with DCs in the absence (gray dotted lines) or presence (black solid lines) of P3C. Filled histograms represent isotype control staining. Numbers indicate the MFI of the parameter analyzed. (C) Cumulative diabetes incidence over time in NOD mice left untreated (None, white circles) or injected at 10 wk of age with 106 Tregs cultured with DCs in the absence (Cult.Naïve Tregs, gray squares) or presence (Cult.P3C Tregs, black diamonds) of P3C. *p<0.05, ***p<0.001, determined using a logrank test.
Virally induced activation of TLR2 signaling during the prediabetic phase diminishes T1D
Based on our results thus far and our previous observations in virally mediated prevention of T1D 12, we addressed whether TLR2 neutralization in vivo concomitant to LCMV infection of NOD mice might affect the capacity of the virus to prevent autoimmunity. Anti-TLR2 blocking mAbs were administered to prediabetic, 9-wk-old NOD mice along with LCMV and again 5 days later, and development of diabetes was monitored. We observed that LCMV delayed the onset of diabetes but failed to significantly reduce disease incidence when administered to NOD mice in the context of TLR2 blockade (Fig. 5). In a different set of experiments, treatment of LCMV-infected NOD mice with isotype control mAbs had no effect on T1D development (data not shown), indicating the selective effect of anti-TLR2 mAbs. These observations suggested that activation of TLR2 signaling during LCMV infection contributed to the capacity of this virus to diminish T1D.
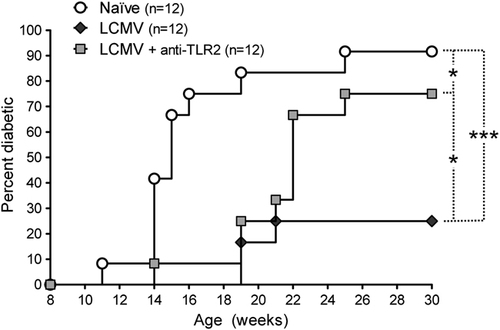
Activation of TLR2 signaling by LCMV infection in prediabetic NOD mice diminishes T1D. Cumulative diabetes incidence over time in NOD mice left untreated (Naive, white circles) or infected at 9 wk of age with LCMV and left untreated (LCMV, black diamonds) or injected simultaneously and 5 days later with 50 μg of TLR2 blocking mAb (LCMV + anti-TLR2, gray squares). *p<0.05, ***p<0.001, determined using a logrank test.
LCMV-induced CD4+CD25+ Treg frequency increase and TGF-β production are TLR2-dependent
Our previous work showed that reduced incidence of autoimmune diabetes following LCMV infection was caused by increased numbers of invigorated CD4+CD25+ Tregs producing TGF-β 12. We thus assessed whether LCMV infection would still enhance Tregs in vivo when TLR2 signaling was impaired. In order to fully disrupt TLR2 signaling, we used mice rendered deficient in TLR2 protein expression by selective mutation of the TLR2 gene (TLR2−/−), on the C57BL/6 (B6) background. We found that LCMV infection increased the percentage of CD4+CD25+ T cells in the spleen of WT B6 mice (Fig. 6A), similar to our earlier observation in NOD mice 12. However, this effect of LCMV appeared hindered in TLR2−/− B6 mice, which showed a mildly but significantly lower increase in CD4+CD25+ T-cell frequency after infection. In both WT and TLR2−/− mice infected with LCMV, the majority of CD4+CD25+ T cells expressed Foxp3 and low levels of CD127 (data not shown), indicating that these cells were indeed Tregs. In B6 mice infected 21 days prior with LCMV, a fraction of CD4+CD25+ T cells were capable of TGF-β production upon polyclonal stimulation (Fig. 6B and C), similar to our previous observation in NOD mice 12 but to a lesser extent (possibly reflecting intrinsic differences in TGF-β production in these two different genetic backgrounds). Although production of TGF-β by CD4+CD25+ T cells from WT mice challenged with LCMV was low, it was virtually absent in LCMV-immune TLR2−/− mice (Fig. 6C). Interestingly, CD4+CD25+ T cells from both WT and TLR2−/− mice infected with LCMV were capable of producing IFN-γ (Fig. 6B and D). These results suggested that the ability of LCMV infection to increase CD4+CD25+ Treg frequency and TGF-β (but not IFN-γ) production in vivo was dependent on TLR2.
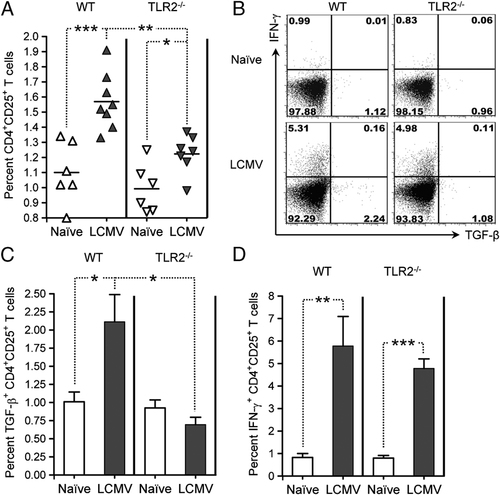
LCMV infection of TLR2-deficient B6 mice fails to enhance the frequency of CD4+CD25+ Tregs and their production of TGF-β in the spleen. (A) Percentage of CD4+CD25+ T cells in the spleen of individual age-matched WT (triangles) or TLR2−/− (inverted triangles) B6 mice left untreated (white symbols) or infected 21 days prior with LCMV (black symbols), measured by flow cytometry. Each symbol represents one mouse; horizontal bar indicates the mean. *p<0.05, **p<0.005, ***p<0.001, determined using an unpaired, two-tailed t-test. (B) Representative flow cytometry dot plots of TGF-β and IFN-γ production by CD4+CD25+ T cells in the spleen of individual age-matched WT or TLR2−/− B6 mice left untreated (Naïve) or infected 21 days prior with LCMV (four to seven mice per group), measured by flow cytometry after polyclonal stimulation. Quadrants were defined based on isotype control stainings showing under 0.2% positive cells for each parameter analyzed. Numbers indicate the percentage of cells in the corresponding quadrants. (C, D) Percentage of (C) TGF-β- and (D) IFN-γ-producing CD4+CD25+ T cells in the spleen of WT or TLR2−/− B6 mice left untreated (Naïve, white bars) or infected 21 days prior with LCMV (black bars), measured by flow cytometry after polyclonal stimulation (Mean+SEM from four to seven mice per group). *p<0.05, **p<0.005, ***p<0.001, determined using an unpaired, two-tailed t-test.
Viral infection confers CD4+CD25+ Tregs protective capacity in T1D via TLR2 and DCs
Based on these results, we assessed whether (i) similar to NOD mice CD4+CD25+ Tregs from LCMV-immune B6 mice might show a gain of function in autoimmune diabetes 12 and (ii) whether this phenomenon might be dependent on TLR2. To this aim, we used B6 RIP-GP mice 5, 6, which express the LCMV glycoprotein (GP) selectively in their pancreatic β cells and develop T1D following infection with LCMV. CD4+CD25+ T cells were purified from the spleen of LCMV-immune WT B6 mice and adoptively transferred into B6 RIP-GP mice in which autoimmune diabetes was triggered simultaneously by LCMV infection. Although the results we obtained did not reach statistical significance (p=0.0796), they showed a trend toward a protective effect of Tregs when virally modulated in WT but not TLR2-deficient mice (Fig. 7A). Based on the importance of DCs in inducing T-cell responses to LCMV 37 and enhancing Tregs in T1D 35, 36, we attempted to increase the effect of CD4+CD25+ Tregs by further exposing them in vitro to DCs from LCMV-infected mice. CD4+CD25+ Tregs purified from LCMV-immune mice were exposed in vitro to DCs obtained from mice recently challenged with LCMV, which we and others found to harbor an activated phenotype and carry LCMV particles (data not shown, and 38). After 6 days in culture, the Tregs were separated from the DCs and adoptively transferred into B6 RIP-GP mice in which autoimmune diabetes was triggered simultaneously by LCMV infection. While the capacity of LCMV-exposed, WT CD4+CD25+ T cells to protect B6 RIP-GP mice from T1D was enhanced after culture with DCs from WT LCMV-infected mice (Fig. 7B), TLR2−/− Tregs cultured with TLR2−/− DCs had no effect on disease development. These results indicated that LCMV-mediated Treg enhancement could be conferred by DCs and depended on TLR2.
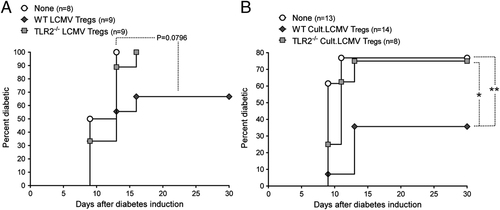
LCMV confers CD4+CD25+ Tregs with protective capacity in virally induced T1D via TLR2 and DCs. (A) Cumulative diabetes incidence over time in B6 RIP-GP mice infected with LCMV and left untreated (None, white circles) or simultaneously injected with 1.5×106 CD4+CD25+ T cells purified from WT (WT LCMV Tregs, black diamonds) or TLR2−/− B6 mice (TLR2−/− LCMV Tregs, gray squares) infected 21 days prior with LCMV. Statistical significance determined using a logrank test. (B) CD4+CD25+ T cells purified from WT or TLR2−/− B6 mice infected 21 days prior with LCMV were cultured for 6 days with DCs purified from WT or TLR2−/− B6 mice, respectively, infected 48 h prior with LCMV (Cult.LCMV Tregs). Shown is cumulative diabetes incidence over time in B6 RIP-GP mice infected with LCMV and left untreated (None, white circles) or simultaneously injected with 5×105 Tregs from WT (WT Cult.LCMV Tregs, black diamonds) or TLR2−/− (TLR2−/− Cult.LCMV Tregs, gray squares) cultures. *p<0.05, **p<0.005, determined using a logrank test.
Discussion
Our observations indicate that triggering of TLR2 in a naïve context or upon viral infection confers protection from autoimmune diabetes by promoting the expansion of invigorated CD4+CD25+ Tregs, possibly via DCs. Since P3C-induced signaling occurs through heterodimerization of TLR2 with TLR1, further studies should assess the contribution of TLR1 in induction of immunoregulation and protection from T1D. We did not observe Treg enhancement after treatment of NOD mice with Pam2CSK4 (data not shown), thus excluding a role for TLR6-TLR2 heterodimerization in this phenomenon.
TLR2 was previously shown to promote rather than hinder T1D, notably by inducing TNF-α production by APCs 18. On the other hand, a requirement for TLR2 in the development of T1D was not supported by a recent study 32. Such opposing roles of TLR2 in this disease might reflect the importance of β-cell antigen release concomitant to TLR signaling for autoimmunity to develop. TLR stimulation indeed causes autoimmune diabetes when triggered in the presence of β-cell antigens 16, 17, but otherwise prevents the disease 24-27. Our previous 12 and present findings suggest that this might be due to the capacity of immunostimulatory factors to enhance immunoregulation. Another, possibly related, important aspect might be the timing at which TLRs, and subsequent release of inflammatory cytokines, are triggered during the prediabetic phase 39. In this regard, previous studies by us and others have shown that TNF-α differentially affects the outcome of T1D depending on the time of action 10, 40, 41. TNF-α may also have opposing effects on CD4+CD25+ Tregs 41-43, which play a crucial role in T1D. Other inflammatory cytokines such as IFNs can also differentially affect autoimmune processes in T1D, as supported by our previous work 12. Finally, while TLR2 delivers pro-inflammatory signals, its engagement also causes the release of anti-inflammatory/immunoregulatory cytokines such as IL-10 44, 45. In sum, innate immune receptors like TLR2 can promote both autoimmunity and immunoregulation, and whether one or the other prevails appears to determine the outcome of T1D.
In sum, modulation of the balance between autoimmunity and immunoregulation, and thus subsequent induction or prevention of T1D, might rely on the dual function of the innate immune players involved in the disease. Depending on timing and whether β-cell antigens are present, TLR-mediated effects will differentially affect the development of autoimmunity. The opposing roles of infections in T1D, which also depend on timing and vary in terms of damage to β cells 2, may thus be accounted for by the capacity of viruses to differentially affect such innate immune factors depending on the context. For instance, TLR2 signaling, and subsequent activation of APCs/T cells and production of inflammatory cytokines, may promote autoimmune processes when β-cell antigens are present, but also appear to counter autoimmunity by enhancing and invigorating CD4+CD25+ Tregs and conferring DCs with tolerogenic properties.
Previous work has shown that TLR2 signaling enhances the function of CD4+CD25+ Tregs 22 and regulates their expansion and activity 29, 30. TLR2 was proposed to control antimicrobial immunity by transiently limiting the function of natural Tregs (thus permitting T-cell immunity) while enhancing their number (thus participating in terminating it). Accordingly, we found that acute anti-LCMV immunity coincided with ineffective activity of CD4+CD25+ Tregs (data not shown) but resulted in their increased frequency and function. TLR2 might thus act to regulate antiviral immunity, by enhancing the number and function of Tregs to control it, but impairing these cells as long as the invading virus is present. Intriguingly, to date, there is no evidence that LCMV particles can bind to TLR2. But while TLR2 is responsible for sensing components from micro-organisms, it can also recognize molecular motifs from certain endogenous ligands. In this regard, the chaperone HSP60 was shown to enhance the function of CD4+CD25+ Tregs through TLR2 signaling 22. It is thus possible that viral infection triggers the release of molecules such as HSPs, which promote the direct enhancement of CD4+CD25+ Tregs via TLR2. This might constitute a means to recognize and control potentially harmful immune processes through innate immunity. Such absence of antigenic specificity could enable control of immunity to infection not only by viruses but also bacteria or other pathogens. In particular, in the hygiene hypothesis it is proposed that a number of different infections in early life contribute to reduced susceptibility to T1D 46. The capacity of the immune system to control immunopathology independent of antigen may thus account for the ability of numerous infections or non-infectious pro-inflammatory agents to protect from T1D in experimental models for this disease 13.
While the mechanism by which TLR2 signaling conferred DCs with anti-diabetogenic properties remains to be determined, viral infection or P3C exposure may have enabled these cells to ameliorate the function of CD4+CD25+ Tregs. Activated DCs present antigens normally not presented via MHC molecules under non-inflammatory conditions, e.g. in the absence of infection. This might notably be the case for self-antigens released in the inflammatory milieu physiologically or upon immune-mediated tissue damage. A possible candidate in this regard is HSP60, which can enhance the function of CD4+CD25+ Tregs directly 22, but whose immunodominant peptide p277 bears tolerogenic properties in T1D, such that it is now evaluated in clinical studies to treat this disease 47, 48. As discussed above, endogenous molecules like HSP60 may thus be released during viral infection and confer CD4+CD25+ Treg enhancement directly via TLR2, but also indirectly via antigenic presentation by DCs. In addition, presentation of other self-antigens by DCs under inflammatory conditions might promote the recruitment of diabetogenic CD8+ T cells in the vicinity of DCs and their subsequent impairment by these cells. Such a phenomenon could occur for example through the PD-L1/programmed death-1 pathway, as suggested by our previous study 12. In this regard, our present results and data not shown indicate that lymphoid cells stimulated through TLR2 in vitro or in vivo acquire high PD-L1 expression. In sum, it is possible that the contribution of DCs in TLR2-mediated prevention of T1D is to promote Treg function while curbing autoreactive responses.
A promising alternative to the therapeutic induction or enhancement of Tregs in vivo to treat T1D is their expansion in vitro for cell-based therapy. Our results suggest that stimulation via TLR2 might be well-suited for this purpose. Strategies exist to grow human CD4+CD25+ Tregs in large numbers in culture 49, and effort is currently undertaken to develop this approach in clinical trials 50. A number of strategies consist of expanding Tregs polyclonally through stimulation via the TCR, along with co-stimulation (e.g. anti-CD3 and anti-CD28). While such expanded Tregs exhibit good preventive capacity in autoimmune diabetes, they seem to show rather limited efficacy in the reversion (as opposed to prevention) of new-onset disease. This may be due in part to their non-antigen-specific nature, but also notably to the inability of TCR-restricted stimulation to augment their suppressive function. Our results indicate that stimulation through TLR2 could be used as a means to not only increase the number of CD4+CD25+ Tregs in vitro, but also ameliorate their in vivo tolerogenic property in T1D.
We identify here a mechanism by which innate immunity, namely TLR2 stimulation, promotes immunoregulation and controls autoimmune processes in T1D. Therefore, it appears that similar phenomena account for both development and prevention of autoimmune diabetes. This suggests that the recurring occurrence of infectious events during early life might promote autoimmunity but will also drive the immune system to build increased immunoregulatory force. In this way, even in the case where autoimmune diabetes would be caused by an infection, previous encounters with other infectious agents might still prevent its development. Our results thus provide a novel mechanistic basis reconciling previous opposite observations in the field of infections and T1D. In addition, our finding that stimulation through TLR2 constitutes a well-suited means to expand CD4+CD25+ Tregs while ameliorating their tolerogenic function in T1D opens new possibilities for therapy of this disease and possibly other autoimmune disorders.
Materials and methods
Mice and virus
NOD/ShiLtJ mice, and WT or TLR2−/− C57BL/6J (B6) mice were purchased from the Jackson Laboratory. C57BL/6-RIP-GP (B6 RIP-GP) transgenic mice were described previously 5, 6. For infection, a single dose of 104 PFU LCMV Armstrong 53b was given intraperitoneally. Blood glucose was monitored using OneTouch Ultra system (LifeScan), and mice exhibiting values greater than 300 mg/dL were considered diabetic. Animal work in all studies was approved by the LIAI Animal Care Committee.
Treatments
All injections were performed intraperitoneally in 200 μL volume. Tregs, DCs, and mouse anti-mouse TLR2 mAb (Invivogen) were injected in PBS, and P3C (EMC Microcollections) was injected in DMEM (Invitrogen).
Insulitis scoring
Pancreas was collected and snap-frozen at the indicated time point after treatment. Frozen sections were stained with hematoxylin and eosin, and insulitis was scored blinded, as follows: (0) no insulitis, (1) peri-insulitis with no islet destruction, (2) severe peri-insulitis and some infiltrating insulitis, (3) infiltrating insulitis and some islet destruction, (4) infiltrating insulits and extensive islet destruction (or islet destroyed).
Flow cytometry
Cells were stained with fluorescently labeled mAbs (BD Biosciences, eBioscience, BioLegend, Caltag) as described previously 12. Samples were processed on a LSRII or FACScalibur (BD Biosciences) and results analyzed using FlowJo (Tree Star). Non-specific binding was blocked using unlabeled anti-FcγR (BD Biosciences). Intracellular Foxp3 expression was assessed using a Foxp3 detection kit (eBioscience). For intracellular staining of cytokines, CD4+CD25+ T cells were stimulated with PMA and ionomycin (10 ng/mL and 0.5 μg/mL, respectively) or anti-CD3 (5 μg/mL) in Brefeldin A (Sigma-Aldrich) buffer prior to mAb staining.
CD4+CD25+ T-cell purification
Female mice were euthanized 21 days after P3C treatment or LCMV infection, at which point virus was cleared from lymphoid tissue (data not shown). Cell suspensions were prepared from pooled spleens, mesenteric, inguinal, and pancreatic LN of 10–25 mice per group, and CD4+CD25+ T cells were purified as described previously 12. Briefly, CD4+ T cells negatively selected by magnetic separation using sheep anti-rat Dynabeads (Dynal) were stained with biotinylated anti-CD25 mAb, and CD4+CD25+ cells were purified by magnetic separation using anti-streptavidin MACS microbeads (Miltenyi Biotec). Cell purity was measured by flow cytometry and always greater than 95%.
DC purification
Mesenteric, inguinal, and pancreatic LNs were collected and pooled from 5–25 female mice. After disruption by incubation at 37°C for 30 min in HBSS (Invitrogen) containing 0.5 mg/mL collagenase D (Roche), DCs were purified by magnetic separation using anti-CD11c MACS microbeads. Non-specific binding was blocked using unlabeled anti-FcγR (BD Biosciences). Cell purity was assessed by flow cytometry and always greater than 92%.
Treg culture
For P3C cultures, CD4+CD25+ T cells purified from naïve female NOD mice were cultured for 6 days with 2 μg/mL P3C and DCs purifed from naïve female NOD mice, at a ratio of 1 DC:3 Tregs, in RPMI 1640 supplemented with 10% FCS, 2 mM L-glutamine, and 50 μM 2-mercaptoethanol (Complete RPMI), and 10 U/mL rhIL-2. For viral cultures, the CD4+CD25+ T cells were purified from female B6 mice infected 21 days prior with LCMV and cultured for 6 days with DCs purifed from female B6 mice infected 48 h prior with LCMV, at a ratio of 1 DC:3 Tregs, in Complete RPMI. At the end of the cultures, the Tregs were negatively selected using rat anti-mouse MHC class II mAbs (BD Biosciences) and Sheep anti-rat Dynabeads (Dynal).
Statistical analyses
Statistical significance was determined using a logrank test (for T1D assessment) or an unpaired, two-tailed t-test. In all experiments, differences were considered significant when p<0.05. Statistical significance is displayed in each figure for the indicated groups as follows: *p<0.05, **p<0.005, ***p<0.001.
Acknowledgements
The authors thank Malina McClure for mouse colony maintenance, Yang Chen and Tom Wolfe for technical help, and Priscilla Colby for administrative assistance. This work was supported by an NIH P01 grant AI58105-03 with the NIAID for M.G.vH, and fellowships from the JDRF and FRM for C.M.F. The authors also gratefully acknowledge support from the Brehm Coalition.
Conflict of interest: The authors declare no financial or commercial conflict of interest.




