Unexpected Pneumothorax During Painless Flexible Bronchoscopy Under Remimazolam Sedation: Two Case Reports and a Literature Review
Funding: This work was supported by the Scientific Project of Hunan Health Commission (B202304116531).
ABSTRACT
The timely recognition of pneumothorax during painless flexible bronchoscopy (PFB) can be challenging. This report describes two consecutive cases of pneumothorax following PFB, both of which were promptly identified and successfully treated. A sudden decrease in heart rate, combined with hypoxemia, is highly effective for detecting pneumothorax in patients undergoing PFB, with subcutaneous emphysema serving as a key auxiliary diagnostic sign. Remimazolam may provide significant clinical benefits in emergency situations during PFB by allowing patients to be quickly awakened to assist with diagnosis.
Summary
- This report delineates two consecutive occurrences of pneumothorax following painless flexible bronchoscopy performed under remimazolam sedation.
- The prompt identification and management of pneumothorax are essential for optimizing patient prognosis.
Abbreviations
-
- ASA
-
- American Society of Anesthesiologists
-
- CT
-
- computerized tomography
-
- FB
-
- flexible bronchoscopy
-
- MDT
-
- multi-disciplinary treatment
-
- PFB
-
- painless flexible bronchoscopy
-
- PSA
-
- procedural sedation and analgesia
-
- SpO2
-
- peripheral oxygen saturation
1 Introduction
Flexible bronchoscopy (FB) is a vital clinical procedure for diagnosing and treating various pulmonary diseases [1]. Due to the significant discomfort associated with the procedure, the British Thoracic Society guidelines recommend the use of moderate sedation [2]. By administering hypnotic and/or analgesic medications, anesthesiologists can ensure the adequate performance of diagnostic or therapeutic procedures while closely monitoring patients for potential adverse effects [3]. Short-acting or ultra-short-acting sedatives and analgesics are preferred because, after the procedure, patients can quickly regain consciousness and be safely discharged from the hospital [4].
Remimazolam is rapidly hydrolyzed into the nearly inactive zolpidem propionate by tissue esterase in the blood, resulting in fast onset and elimination [5]. After the administration of flumazenil, patients can quickly recover from remimazolam-induced sedation. Pneumothorax can arise from various etiologies [6]. During FB, it is most commonly observed following transbronchial lung biopsies [7]. Pneumothorax and tension pneumothorax following FB are considered rare occurrences [8]. It has been reported that the incidence of pneumothorax during bronchoscopy is 2.4% [9]. However, performing the procedure under deep sedation can make it difficult to quickly diagnose pneumothorax or tension pneumothorax, significantly increasing the risk of fatal outcomes. Recognizing pneumothorax during painless flexible bronchoscopy (PFB) in outpatients is particularly challenging due to the absence of typical symptoms such as sudden pain or dyspnea. Herein, we present two consecutive cases of tension pneumothorax and pneumothorax occurring during FB under remimazolam sedation and discuss the potential clinical benefits of remimazolam in facilitating rapid recovery from deep sedation.
2 Case Reports
2.1 Case 1: Case History
2.1.1 Tension Pneumothorax During Painless Flexible Bronchoscopy
A 49-year-old male (height: 165 cm, weight: 60 kg) underwent a tracheal stent placement due to stenosis caused by tumor compression. After carefully evaluating his airway and major organ function, he was given nasal catheter oxygen (2 L/min), intravenous lactated Ringer's solution, and his upper airway was anesthetized with lidocaine. Meanwhile, sedation and analgesia were achieved with 7 mg of remimazolam and 5 μg of sufentanil as induction, followed by continuous infusion of remimazolam at 25–40 mg/h to maintain deep sedation. The patient maintained spontaneous breathing throughout the entire PFB procedure.
2.2 Case 1: Methods
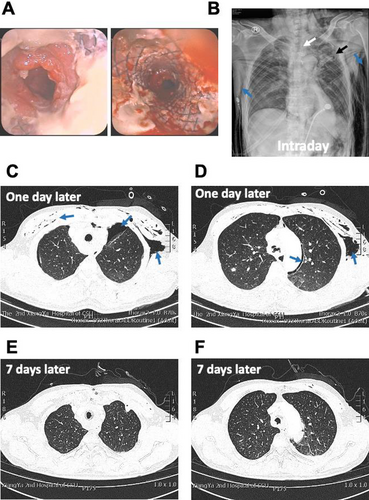
While the pulmonologist was completing the basic examination, we suddenly observed a significant decrease in the patient's heart rate from 85 bpm to approximately 38 bpm. The pulmonologist informed us that he was cleaning necrotic tissues from the main airway at that time. We immediately administered 0.5 mg of atropine, which restored the heart rate. However, following the heart rate drop, the patient's peripheral oxygen saturation (SpO2) gradually declined. Despite attempts to open the airway by raising the jaw and increasing oxygen flow through the nasopharyngeal airway, SpO2 did not return to the baseline level of 98%. Oxygen was administered via the bronchoscope, but the results were unsatisfactory. The patient's vital signs became unstable, and the anesthesiologist was unable to determine the cause immediately. We decided to halt the procedure and wake the patient by administering 0.5 mg of flumazenil. Within 30 s, the patient was responsive and could answer questions about his name and location. He reported no pain or discomfort but appeared agitated and experienced dyspnea. The anesthesiologist promptly conducted a respiratory examination, noting distension of the left thorax, a drum-like sound upon percussion, and absent breath sounds in the left lung on auscultation. Furthermore, signs of subcutaneous emphysema were observed in the face, neck, and thoracic wall. Tension pneumothorax was immediately diagnosed, and a left thoracic puncture was performed. Intubation was initiated to maintain an open airway. After 30 min of mechanical ventilation assistance, the patient regained consciousness and appeared calm.
2.3 Case 1: Outcome and Follow-Up
The patients was then transferred to the intensive care unit for further observation. Figure 1 illustrates the FB images, the thoracic X-ray taken the day after drainage placement, and thoracic CT scans conducted one and 7 days post-treatment.
2.4 Case 2: Case History
A 48-year-old female patient (height: 158 cm; weight: 55 kg) with ASA I classification was diagnosed with a foreign body in the right lower lung. Given the small size (5 × 3.6 mm) and challenging location of the foreign body, a multi-disciplinary team (MDT) consisting of pulmonologists, thoracic surgeons, and an anesthesiologist recommended attempting removal via PFB. The patient was induced with 8 mg of remimazolam and 5 μg of sufentanil, and anesthesia was maintained with 30–40 mg/h of remimazolam. The patient maintained spontaneous breathing throughout the entire PFB procedure.
2.5 Case 2: Methods
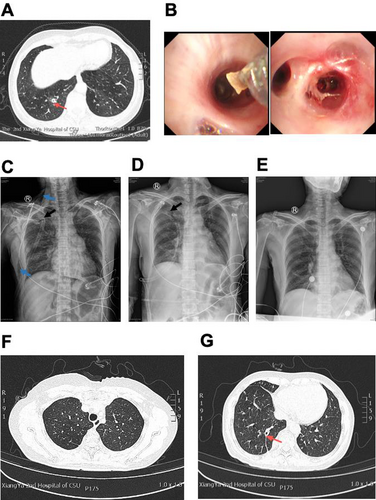
The patient's vital signs remained stable until she suddenly experienced a transient decrease in heart rate from 90 bpm to approximately 35 bpm, which recovered within 30 s. Simultaneously, her SpO2 dropped rapidly from 100% to 70%. The oxygen flow rate was increased to 5 L/min and the jaw was lifted, which improved SpO2 to around 94%. However, several minutes later, SpO2 decreased again to approximately 70%. The pulmonologist immediately halted the bronchoscopy procedure, and the anesthesiologist initiated mask ventilation, which raised SpO2 to 94%. Based on prior experience, the anesthesiologist suspected pneumothorax and administered 0.5 mg of flumazenil for recovery. The patient regained consciousness within a minute and reported right chest pain and difficulty breathing. Extensive subcutaneous emphysema was observed on her face, eyelids, and neck, and absent breath sounds were noted on auscultation of the right lung. Pneumothorax was diagnosed, and thoracic drainage was promptly performed, resulting in SpO2 recovering to about 94% with spontaneous breathing and alleviating dyspnea.
2.6 Case 2: Outcome and Follow-Up
The patient was then transferred to the respiratory ward for further observation. Figure 2 displays the chest X-ray and chest CT images taken before discharge and after PFB therapy, along with images showing the placement of the drainage.
3 Discussion
During PFB, prompt detection and treatment of pneumothorax are crucial to prevent fatal outcomes [10]. In conscious patients with spontaneous breathing, symptoms of pneumothorax include chest pain (52.3%, characterized as pleuritic, sharp, severe, and radiating to the ipsilateral shoulder), dyspnea (38.4%), and shortness of breath (31.4%), among others [11]. Tension pneumothorax may present with additional symptoms such as tachycardia (exceeding 134 bpm), hypotension, jugular venous distension, cyanosis, respiratory failure, and cardiac arrest [12]. However, respiratory symptoms, pain perception, and emotional reactions, including agitation, may be absent in unconscious patients. Pneumothorax during general anesthesia may present as nonspecific vital signs, such as arterial hypotension, arrhythmias, and hypoxia [13]. Arrhythmias are prevalent in patients with pneumothorax, especially tension pneumothorax. The most common initial arrest rhythm in tension pneumothorax is reported to be pulseless electrical activity [10], which can lead to cardiac arrest. In the two cases described, both patients, despite having no history of heart disease, experienced a transient and significant decrease in heart rate, followed by hypoxia. This strongly suggests that a sharp reduction in heart rate combined with hypoxemia may be highly effective for recognizing pneumothorax in patients undergoing painless endoscopy. If these symptoms are observed, pneumothorax should be suspected, and subcutaneous emphysema and respiratory examinations should be conducted for further diagnostic assessment.
Another clinically relevant aspect of the two cases is the benefit of remimazolam for patients undergoing PFB with spontaneous breathing, particularly for therapeutic purposes. Remimazolam effectively sedates patients during PFB, and its sedative effects can be rapidly reversed by flumazenil [14]. Emergent events, such as severe hypoxemia caused by respiratory depression, can occur during PFB with spontaneous breathing. In many cases, differentiating the causes of these events can be challenging, potentially delaying treatment. Therefore, the ability to quickly reverse the effects of remimazolam becomes crucial in such situations. In the two cases presented, when pneumothorax was suspected, flumazenil was promptly administered to reverse the sedation. Both patients transitioned from moderate sedation to full consciousness within 1 min and could answer questions, which was crucial for assisting in diagnosis. This was particularly beneficial in the first case, whereby the patient regained consciousness but initially became agitated and gradually lost consciousness. This helped rule out anesthesia as the cause of the heart rate decrease and hypoxemia, allowing for a shift in focus to other pathological factors. The effective differential diagnosis and rapid recognition of pneumothorax, especially tension pneumothorax, contributed to favorable outcomes for both patients.
In conclusion, a sudden and pronounced decrease in heart rate accompanied by hypoxemia can be valuable indicators for identifying pneumothorax in patients undergoing PFB. Moreover, the ability to swiftly reverse remimazolam-induced deep sedation with flumazenil offers significant clinical advantages in emergency situations, where prompt awakening of patients for diagnostic assessment is crucial during PFB.
Author Contributions
Cong Luo: data curation, visualization, writing – original draft, writing – review and editing. Ru-Yi Luo: conceptualization, writing – original draft, writing – review and editing.
Acknowledgments
The authors have nothing to report.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data and materials described in the manuscript will be freely available for non-commercial purposes.