Desaturation after Fontan procedure due to systemic venous collateral and improvement after closure with embolization
Abstract
Key Clinical Message
Systemic to pulmonary venous collaterals (SPVCs) are common findings in patients with Fontan and may be responsible for desaturation in this group of patients. In selected cases, percutaneous closure of SPVCs with coils or vascular plugs could be offered as a safe and effective treatment modality for these patients.
A 27-year-old female patient who had operated primarily with Glenn operation and she underwent later a lateral tunnel Fontan operation. After 5 years, she presented with desaturation due to significant systemic to pulmonary venous collateral development, and a decision was made to proceed with interventional occlusion. Afterward, the arterial saturations increased.
Fontan circulation is a well-established palliation in patients with functional single ventricles. The absence of a sub-pulmonary pumping chamber creates a unique physiology in which blood flow is mainly guided by negative intrathoracic and elevated central venous pressures. Various pulmonary anatomic or pathophysiologic changes can jeopardize optimal Fontan circulation. Long-term survival of patients who have undergone the contemporary total cavopulmonary connection is satisfactory.
The Fontan physiology chronically increases systemic venous pressure. Systemic to pulmonary venous collaterals (SPVCs) are common findings in patients with Fontan and assumed that embryological structures “recanalize” due to the chronic elevation of central venous pressure.1 SPVCs usually originate from IVC or superior vena cava (SVC), from the innominate vein, or from the azygos and hemiazygos system, and are in connection with pulmonary veins or common atrium.
We present a case of a 27-year-old female patient who had operated initially with Glenn operation (primary diagnosis was double outlet right ventricle with rudimentary left ventricle), and later, she underwent a lateral tunnel Fontan operation completed with fenestration and the later was closed with a Starflex device (Figure 1A).
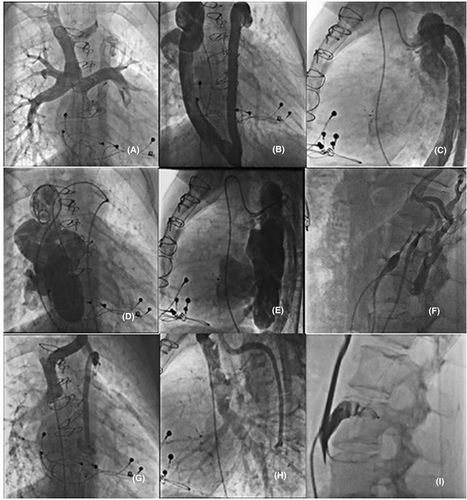
During the years, the patient developed arrhythmias and sinus node disease with tachy-brady arrhythmias and treatment with b blockers resulted in symptomatic pauses greater than 3 s. An epicardial pacemaker with tachyarrhythmia software was then implanted (Figure 1B). After 5 years, she presented with desaturation and SO2 76%–78%.
Catheterization revealed a huge systemic-pulmonic collateral from the embryologically left branciocephalic and superior cardinal vein to hemiazygous–azygous system that with helicoid course opened to pulmonary vein and the common atrium (Figure 1B–E).
A second collateral vessel from inferior vena cava to azygous with the same drainage was imaged in angiography (Figure 1F). The measured pressure at the Fontan was 12–13 mmHg.
A decision was made to proceed with closure of it with the AGA plug system Amplatzer 9 -ΑVP2- 14mm and 09-AVP 12mm, respectively (Figure 1G–I). After occlusion, the arterial saturations increased to 90%.
Large SPVCs often produce systemic arterial de-saturation with secondary erythrocytosis. Percutaneous closure of SPVCs with coils or vascular plugs has been described mostly as case reports. No procedural complications have been described; however, interventional cardiologist should be aware of thoracic duct anatomy and potential increase in central venous pressure. A recognized threshold circuit pressure of 18 mmHg has been set for embolization, as 50% of deaths after embolization occurred in patients with Fontan pressure >18 mmHg.2, 3
AUTHOR CONTRIBUTIONS
Alexandros Tsoutsinos: Investigation; writing – original draft. Felicia Kakava: Investigation. Meletios Kanakis: Investigation; methodology; visualization; writing – original draft. George Samanidis: Investigation; visualization; writing – original draft. Stefanos Despotopoulos: Investigation. George Vagenakis: Investigation. Sotiria Apostolopoulou: Investigation. John Papagiannis: Investigation. Spyridon Rammos: Investigation.
FUNDING INFORMATION
None.
CONSENT
Written informed consent was obtained from the parent of children to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available upon request from the corresponding author.




