The efficacy and safety of laparoscopic common bile duct exploration with primary duct closure for cholecystolithiasis combined with choledocholithiasis
Da Teng and Yue Xu contributed equally to this work.
Key Clinical Message
Cholecystolithiasis combined with choledocholithiasis represents a prevalent disease. At present, regarding the management of the common bile duct (CBD), T-tube drainage (TTD) and primary duct closure (PDC) emerge as two prominent approaches for biliary tract repair after laparoscopic CBD exploration (LCBDE). Here, retrospective analysis was conducted on the clinical records of 157 patients who underwent LCBDE at our hospital between January 2019 and January 2022. All patients were categorized into the PDC group or the TTD group based on the chosen CBD treatment approach. A comparative assessment was made across demographic factors, preoperative conditions, surgical particulars, and postoperative complications. The results showed that PDC is recommended for patients with a limited number of small stones, particularly when the CBD is in the 10–15 mm diameter range.
1 INTRODUCTION
Choledocholithiasis ranks as a prevalent disease within hepatobiliary surgery, standing as the second most common complication after acute cholecystitis.1 Statistics indicate that approximately 15% of patients with cholecystolithiasis also present with choledocholithiasis.2 Manifestations typically include abdominal pain, fever, jaundice, and various other clinical manifestations. In severe cases, patients might experience liver dysfunction, acute cholangitis, and pancreatitis.
The primary objective of choledocholithiasis is to alleviate the obstruction within the common bile duct (CBD) and restore smooth biliary tract drainage. Presently, treatment options primarily encompass CBD exploration (CBDE) and endoscopic retrograde cholangiography (ERCP), yet the optimal approach remains controversial.3 Despite ERCP being a mature method, its implementation carries an elevated risk of postoperative complications such as pancreatitis, cholangitis, bile leakage, and bleeding.4, 5 The heightened risk is attributed to the incision of the Oddi sphincter during the procedure, which can lead to papilla relaxation and contraction dysfunction,6 thereby impeding normal bile and pancreatic juice excretion and potentially increasing the probability of stone recurrence.7 Advancements in laparoscopic and choledochoscopy techniques have facilitated the introduction of laparoscopic CBD exploration (LCBDE) into clinical practice. This approach achieves comparable therapeutic outcomes to laparotomy by directly accessing the CBD, employing a flexible choledochoscope to identify obstructions and biliary tract dilation, and assessing for inflammatory changes and anatomical variations. Additionally, LCBDE offers the advantages of minimal surgical trauma and fast recovery,8, 9 because it has the advantage of avoiding papillotomy and allowing cholecystectomy to be performed in the same step. Relevant retrospective study suggests that LCBDE should be a method of choice for all patients, especially in younger ages.10 Regarding CBD management following LCBDE, two prevalent methods for biliary tract repair are T-tube drainage (TTD) and primary duct closure (PDC).11 TTD is widely used in clinical practice and deemed relatively safe and has become the standard approach for biliary tract repair after LCBDE.12 However, prolonged T-tube indwelling postoperatively might lead to electrolyte imbalances, increased pain risk, T-tube dislodgement, and hindered postoperative recovery.13 Conversely, PDC preserves CBD integrity, facilitating the early excretion of all bile into the intestine to restore normal physiological function, without necessitating T-tube placement, thereby reducing postoperative complications and promoting rapid recovery.14, 15 Nevertheless, the choice between these two methods remains controversial, lacking clear clinical guidelines and exhibiting variability across medical centers. To elucidate the perioperative differences between these two approaches following LCBDE and guide clinical practice, a retrospective study was conducted aiming to provide valuable insights into CBD repair methods.
2 MATERIALS AND METHODS
2.1 Patient data collection
This retrospective study analyzed the clinical data of patients undergoing LCBDE due to cholecystolithiasis combined with choledocholithiasis in the first ward of hepatobiliary, pancreatic, and splenic surgery at Chuzhou Hospital affiliated with Anhui Medical University, from January 2019 to January 2022. Informed consent was obtained from all patients and their families. Patients diagnosed with cholecystolithiasis and choledocholithiasis confirmed through abdominal ultrasound, computed tomography (CT) scans, magnetic resonance cholangiopancreatography (MRCP), and other imaging modalities were included in the study. Exclusion criteria encompassed patients with acute obstructive suppurative cholangitis and acute severe pancreatitis or those who received a secondary diagnosis and treatment of CBD before surgery. A total of 157 patients were ultimately enrolled. Based on the varied CBD treatment modalities, they were categorized into the PDC group or the TTD group. Among these, laparoscopic procedures were completed without conversion to laparotomy for 75 patients in the PDC group and 82 patients in the TTD group. The choice between the two approaches depends on surgeon's judgment, the patient's preoperative performance, and the patient's self-selection after informed consent. This study was approved by the research ethics committee of the Affiliated Chuzhou Hospital of Anhui Medical University (reference, 2023 Ethical Review [Bio] no. 1; date of approval: January 26, 2023).
The study collected comprehensive data encompassing preoperative, intraoperative, and postoperative data of patients. The primary outcomes included information about postoperative and complications, the secondary outcomes included the stone and CBD characteristics, information about the intraoperative. Baseline data consisted primarily of age, sex, body mass index (BMI), comorbid hypertension, diabetes, and preoperative leukocyte levels. Patients’ disease characteristics included the number of stones, the maximum diameter of stones, CBD diameter, stone removal success rate, as well as postoperative levels of total bilirubin (TBIL), direct bilirubin (DBIL), alanine aminotransferase (ALT), and aspartate aminotransferase (AST). Additionally, the study recorded the operation time, drainage volume, extubation time, duration of postoperative hospital stay, and associated hospitalization costs. Furthermore, the presence of residual stones, bile leakage, bleeding, electrolyte disorders, postoperative pancreatitis, cholangitis, biliary stricture, and recurrence were also documented.
2.2 Definitions
The CBD diameter refers to the maximum diameter of the CBD measured using ultrasonography and MRCP before surgery. Postoperative pancreatitis was characterized by the sudden onset of upper abdominal pain, abdominal distension, and vomiting, along with elevated blood and urine amylase levels, and findings of peripancreatic exudative changes on abdominal ultrasound, CT scans, or other diagnostic imaging modalities. Cholangitis was identified by the presence of upper abdominal pain, fever, jaundice, and other clinical manifestations after surgery, accompanied by elevated leukocyte and neutrophil counts in laboratory tests. Bile leakage was defined as drainage fluid bilirubin concentration exceeding three times the normal serum concentration 3 days after surgery. Residual stones were described as stones incompletely removed during the procedure. Recurrence was defined as the reappearance of stone formation 6 months after complete stone removal during the initial operation.
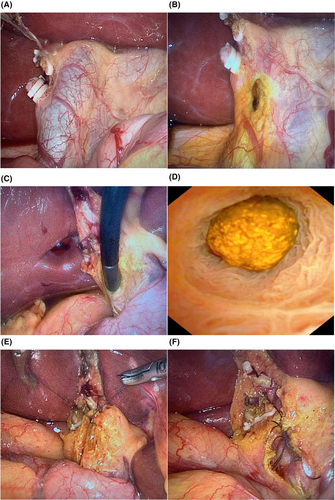
2.3 Surgical procedure
General anesthesia was administered to both groups via tracheal intubation. Once anesthesia took effect, pneumoperitoneum was established, maintaining pressure at 12–14 mmHg (1 mmHg ≈ 0.133 kPa), and the four-trocar method was employed. For laparoscopic cholecystectomy + LCBDE, the gallbladder's bottom was pulled to expose the gallbladder triangular area. The Calot triangle was flattened, and the free cystic duct and gallbladder blood vessels were cleared before disconnection. The gallbladder was then removed from its bed by electrocoagulation. The hepatoduodenal ligament was exposed, and longitudinal electrocoagulation opened the membrane structure to reveal the anterior wall of the CBD. A posterior longitudinal incision of approximately 1.0–2.0 cm was confirmed (Figure 1). A flexible choledochoscope (Olympus, Tokyo, Japan) was inserted through the operating trocar beneath the xiphoid process to explore the lower segment of the CBD, the common hepatic duct, the left and right hepatic ducts, and the secondary intrahepatic bile duct, respectively. Stones were removed using the Dormia basket. It was confirmed that all segments of the CBD were unobstructed and that the Oddi sphincter exhibited satisfactory relaxation and contraction function. In the PDC group, a 4-0 absorbable suture (Vicryl, Ethicon Inc., Somerville, NJ, USA) was used to suture the incision on the anterior wall of the CBD. Endoscopic gauze was dipped to observe for bile leakage. A drainage tube was inserted into the foramen of Winslow. If the drainage fluid was <30 mL/day, with clear coloration, no evident bile leakage or bleeding, and no fluid accumulation around the gallbladder fossa via abdominal ultrasound, the drainage tube was removed. In the TTD group, a T-tube (size: 18–22) was inserted into the CBD through the incision. A 4-0 absorbable suture intermittently secured the CBD, and the T-tube was tied and led out of the body. Normal saline (15–20 mL) was injected through the T-tube to check for bile leakage. A drainage tube was placed in the foramen of Winslow. The criteria for drainage tube removal were the same as those in the PDC group. On Postoperative Day 7, the patients were advised to attempt clamping the T-tube. If no significant abdominal distension or discomfort occurred, the T-tube remained clamped. After 6 weeks, T-tube angiography was performed to confirm the absence of residual stones and adequate sinus growth before T-tube removal.
2.4 Postoperative management
The patient was routinely given postoperative symptomatic treatment such as anti-inflammatory, analgesic, cholagogic, anti-spasmolytic, liver protection, and enzyme inhibition therapies, which take the intravenously guttae. Postoperative care pays particular attention to smooth drainage the tube of the foramen of Winslow and T-tubes. During the treatment period, the patient's vital signs were stable, resumed semi-liquid diet without obvious clinical manifestations such as abdominal pain, distension, fever, jaundice, etc. There were no abnormalities in biochemical tests and imaging examinations, and the patient was discharged from the hospital after removal of the drainage tube. Ursodeoxycholic acid capsules were taken after discharge until the first outpatient follow-up.
2.5 Follow-up
Postoperative observation and imaging examinations were used to determine the presence of complications throughout the treatment. Comprehensive follow-up was ensured via outpatient visits and telephonic consultations to evaluate clinical efficacy. All patients were followed up for a minimum of 12 months, with the follow-up period extending until January 2023.
2.6 Statistical analysis
Statistical analysis was performed using the IBM SPSS 22.0 (Chicago, IL, USA) software. The measurement data were verified for normality using the Shapiro–Wilk test.Normally distributed data were used for the t-test, expressed as the mean ± standard deviation. For skewed distribution data, represented by , the rank sum test was employed for comparison. The categorical data are expressed as the number and percentage (N [%]). The Cochran–Mantel–Haensze χ2 test or Fisher's exact test, when appropriate, was used for categorical data analysis. Statistical significance was set at p < 0.05.
3 RESULTS
Both patient groups successfully underwent the surgery without requiring conversion to laparotomy, and there were no adverse events such as perioperative death. The baseline characteristics including age ([56.48 ± 14.76 years] vs. [56.33 ± 15.59 years], p = 0.951), and BMI (23.20 [22.15–24.84] vs. 23.64 [22.80–24.58] kg/m2, p = 0.109) between the PDC and TTD groups showed no statistical differences. There were 35 (46.7%) male and 40 (53.3%) female patients in the PDC group, and 39 (47.6%) male and 43 (52.4%) female in the TTD group, with no statistically significant difference between the two groups (p = 0.911). There were 11 (14.7%) patients in the PDC group with hypertension, and 14 (17.1%) patients in the TTD group, with no statistically significant difference between the two groups (p = 0.681).There were seven (9.3%) patients in the PDC group with diabetes, and eight (9.8%) patients in the TTD group, with no statistically significant difference between the two groups (p = 0.928). There were no significant discrepancies in terms of leukocyte (7.03 [4.88–9.74] vs. 6.64 [5.20–8.66] × 109/L, p = 0.578), TBIL (54 [31.10–76.10] vs. 65.55 [31.20–105.55] μmol/L, p = 0.075), DBIL (30.20 [14.50–47.30] vs. 41.10 [12.70–66.90] μmol/L, p = 0.117), ALT (154.20 [88.40–314.90] vs. 228.10 [116.03–398.55] U/L, p = 0.109), and AST (155.33 [87.51–301.30] vs. 227.72 [94.03–377.04] U/L, p = 0.099) levels between the PDC and TTD groups.
A statistically significant difference was observed in the number of stones between the PDC and TTD groups ([1.56 ± 0.92] vs. [2.07 ± 1.16], p = 0.003), as well as in the maximum diameter of stones ([0.63 ± 0.29 cm] vs. [0.84 ± 0.43 cm], p = 0.001). Patients were further stratified into four groups based on the CBD diameter as follows: ≤8, 8–10, 10–15, and >15 mm. In the PDC group, the distribution was as follows: 3 (4%) patients with CBD diameters of ≤8 mm, 16 (21.3%) patients with diameters of 8–10 mm, 44 (58.7%) patients with diameters of 10–15 mm, and 12 (16%) patients with diameters of >15 mm. Correspondingly, in the TTD group, there were 12 (14.6%), 11 (13.4%), 30 (36.6%), and 29 (35.4%) cases in the ≤8, 8–10, 10–15, and >15 mm groups, respectively (p = 0.024, 0.189, 0.006, and 0.006).In both groups, the presence of stones was confirmed, and all stones were successfully removed (100%).Regarding preoperative biochemical findings, there were no significant differences between the PDC and TTD groups in terms of TBIL (19.60 [14.20–24.10] vs. 20 [12.25–32.90] μmol/L, p = 0.370) and DBIL (7.80 [5.10–13.40] vs. 8.45 [5.20–14.93] μmol/L, p = 0.420). However, significant differences were observed in postoperative ALT and AST levels between the PDC and TTD groups (26.10 [17.20–35.20] U/L vs. 38.70 [21.05–84.65] U/L, p = 0.002) and (25.66 [17.50–35.41] U/L vs. 32.19 [20.83–56.79] U/L, p = 0.009), respectively. In terms of surgical outcomes, the PDC group exhibited superior performance compared to the TTD group. Specifically, the PDC group had significantly shorter operation times ([85.52 ± 20.37 min] vs. [119.22 ± 42.56 min], p < 0.001), reduced drainage volumes ([24.16 ± 13.86 mL] vs. [59.20 ± 15.10 mL], p < 0.001), shorter extubation times ([5.16 ± 1.46 days] vs. [7.29 ± 1.87 days], p < 0.001), postoperative hospital stay ([8.21 ± 2.55 days] vs. [11.28 ± 2.84 days], p < 0.001), and lower hospitalization costs ([15,566.30 ± 1755.49 Yuan] vs. [20,354.24 ± 3851.00 Yuan], p < 0.001), all of which were statistically significant.
The average follow-up duration was 24.7 ± 10.9 months (range: 12–48 months). No statistically significant differences were observed between the PDC and TTD groups in terms of postoperative complications. Throughout the follow-up period, three (4%) cases of residual stones were identified in the PDC group, leading to ERCP lithotomy performed 1 month after the surgery. These patients have since exhibited satisfactory recovery during regular outpatient follow-up visits. In the TTD group, five (6.1%) patients with residual stones were successfully treated after 3 months of choledochoscopy and T-tube sinus lithotomy (p = 0.551). No incidents of bleeding were reported in either group (p = 1.000). 2 (2.7% vs. 2.4%) cases of pancreatitis after surgery were observed in the PDC and TTD group (p = 0.928), which were managed effectively with symptomatic treatments including anti-inflammatory, analgesic, cholagogic, anti-spasmolytic, and enzyme inhibition therapies. In the PDC group, three (4%) cases of bile leakage after surgeries were reported. Cholangiography and MRCP revealed bile extravasation caused by the suture needle. The negative pressure drainage tube passing through the foramen of Winslow was unobstructed, and symptomatic treatment, including anti-inflammatory, cholagogic, and anti-spasmolytic therapies, resulted in successful patient recovery. Similarly, in the TTD group, five (6.1%) cases of postoperative bile leakage were reported. T-tube angiography and MRCP examinations indicated bile extravasation around the T-tube. Endoscopic nasobiliary drainage was performed, alongside anti-inflammatory, cholagogic, and anti-spasmolytic treatments, leading to patient recovery (p = 0.551). four (5.3% vs. 4.9%) cases of cholangitis occurred in both the PDC and TTD groups (p = 0.897), with successful resolution following symptomatic treatments, including anti-inflammation, liver protection, and cholagogic therapies. No instances of biliary stricture were observed in either group (p = 1.000). Electrolyte disorder was observed in two (2.7%) cases in the PDC group and six (7.3%) cases in the TTD group (p = 0.186). These cases were effectively managed through fluid infusion to stabilize the internal environment. Throughout the follow-up period, two (2.7%) cases of recurrence were observed in the PDC group and four (4.9%) cases in the TTD group (p = 0.470). All patients experiencing recurrence were successfully treated with ERCP/endoscopic sphincterotomy (EST) lithotomy.
4 DISCUSSION
In this study, we compared the efficacy and safety of undergoing PDC with the conventional TTD method of biliary tract repair after LCBDE. It clearly demonstrates that PDC is a safe and feasible treatment with the shorter operation times, reduced drainage volume, shorter extubation times, shorter postoperative hospital stays, lower hospitalization costs, and without increasing the risk of postoperative complications, provided that the indications for the procedure are strictly adhered to.
Currently, TTD remains the primary approach for repairing the biliary tract following LCBDE. The T-tube serves a supportive function by ensuring bile drainage, thereby reducing biliary tract pressure. Once the sinus is securely formed, choledochoscopy can be employed to assess for residual and recurrence stones.16 However, the T-tube typically remains in place for approximately 6 weeks after laparoscopic surgery, and removal is contingent upon the firm establishment of the sinus as confirmed by T-tube angiography. Prolonged T-tube indwelling might diminish postoperative quality of life, elevate the risk of postoperative biliary tract infections, and even result in spontaneous T-tube dislodgement.17, 18 These considerations have prompted hepatobiliary surgeons to explore the feasibility and safety of PDC. The past clinical studies suggest that PDC outperforms TTD in terms of operation time, hospital stay, and associated costs. Moreover, there is no significant difference between the two procedures in terms of postoperative complications such as bile leakage and residual stones. Consequently, PDC offers distinct advantages and can be safely implemented.19, 20
Our findings demonstrate a significant correlation between the selection of biliary tract treatment in LCBDE and several factors, including the diameter and number of stones and the diameter of the CBD. First, it was hypothesized that flexible choledochoscopy can evaluate potential inflammatory changes such as edema and congestion due to long-term stone incarceration. Second, if a stone is excessively large, surpassing the CBD diameter and exerting significant pressure, it might pose challenges during removal, thereby increasing the risk of biliary tract mucosal damage and Oddi sphincter edema and spasm during the procedure. Furthermore, stones with a soft and fragile texture are prone to leaving residues during extraction, leading to the presence of residual stones after the procedure. Consequently, to mitigate intraoperative bile duct injury and postoperative complications, PDC typically selects cases with relatively small, fewer stones that are easily extractable, while TTD is recommended for those with larger stones and higher stone counts. The patients were categorized into four groups based on CBD diameter distribution. The PDC group exhibited a higher proportion of patients with diameters falling within the “10–15 mm” range, whereas in the TTD group, patients with CBD diameters of “≤8 mm” and “>15 mm” were more prevalent. There was no significant difference in the proportion of patients with CBD diameters falling within the “8–10 mm” range, and both groups successfully underwent surgery with manageable complications. It is believed that these findings underscore the influence of CBD diameter on the selection of surgical methods. Based on our experience, patients with CBD diameters of ≤8 and >15 mm tend to favor TTD. The presence of a T-tube can help maintain the CBD diameter and mitigate the risk of biliary stricture formation while facilitating bile drainage to reduce biliary tract pressure and minimize the risk of postoperative bile leakage. PDC is suitable for CBD diameters ranging between 10 and 15 mm, facilitating efficient exploration and stone extraction without necessitating T-tube support to uphold the CBD diameter. Following stone removal, CBD obstruction is alleviated, and with a properly functioning Oddi sphincter, smooth bile drainage is promptly restored, thereby reducing biliary tract pressure.
Based on the postoperative outcomes observed in both groups, it was believed that PDC offers similar advantages to TTD in expediting postoperative rehabilitation, reducing the duration of postoperative hospital stay and curtailing hospitalization costs. These findings align closely with the conclusions drawn from some clinical studies.21-23 A retrospective study by Dong et al shows that the operating time was much shorter in PDC than TTD ([102.6 ± 15.2 min] vs. [128.6 ± 20.4 min], p = 0.017). The length of postoperative hospital stay was longer in TTD than PDC ([4.9 ± 3.2 days] vs. [3.2 ± 2.1 days], p = 0.023).The hospital expenses in PDC were statistically lower than that of the TTD ([11,278.9 ± 479.1 Yuan] vs.[12,436.7 ± 879.3 Yuan], p = 0.041).24 Meanwhile, a retrospective study by Zhu et al. analyzed by propensity score matching concluded that: in terms of operation time ([171 ± 71 min] vs.[231 ± 79 min], p < 0.001), blood loss (20[10–30]mL vs. 30[20–50]mL, p < 0.001), postoperative hospital stay (4 [2–5] days vs.7 [5–9] days, p < 0.001), and postoperative drainage time(2 [1–3] days vs. 4 [3–6] days, p < 0.001), PDC was obviously superior to TTD.25 The above findings are similar to ours. With a special emphasis on the substantial decrease in bilirubin and transaminase levels following surgery in both groups underscores the effectiveness of both methods in alleviating biliary tract obstruction and progressively restoring liver function. Nevertheless, compared with TTD, PDC represents a more physiological approach, enabling the complete discharge of bile into the intestine. This facilitates the restoration of patients' digestive function and enhances bile acid intestinal-liver circulation, thereby accelerating the recovery of liver cell synthesis and metabolism. Consequently, the decline in transaminase levels is significantly pronounced in the PDC group.
No statistically significant differences were observed in terms of postoperative complications between the two groups, indicating that PDC did not increase perioperative risks for patients under stringent adherence to surgical indications. Notably, in our study, neither bleeding nor biliary stricture occurred following PDC. Instances of residual stones after surgery primarily correlate with the surgeon's proficiency in choledochoscope utilization and the formation of stone residues during the extraction process. Additionally, there may be small stones within the secondary biliary tract in the liver that discharge into the CBD. Remedial measures for residual stones after LCBDE can be provided through ERCP/EST.26 Regarding pancreatitis, it was postulated that prolonged stone removal due to the long-term incarceration period might lead to repeated biliary tract stimulation, resulting in duodenal papillary oedema and impaired drainage of bile and pancreatic juice. For individuals with challenging stone removal due to incarceration, prophylactic somatostatin administration after surgery, supplemented by anti-spasmodic and cholagogic therapy, is recommended. Bile leakage represents the most frequent complication of PDC and might stem from Oddi sphincter oedema and spasm, as well as increased biliary tract pressure. Additionally, it is associated with excessive CBD traction, wide suture spacing, and improper suture selection. Notably, the influence of CBD diameter on bile leakage after PDC cannot be disregarded, with relevant studies positing that slender CBD serves as an independent risk factor for such leakage.27 To prevent bile leakage, emphasis should be placed on adhering to PDC indications, mastering suture techniques, and selecting appropriate sutures. Specifically, PDC is suitable for CBD diameters ranging between 10 and 15 mm, with an absence of evident inflammatory changes in the inner wall of the biliary tract, and measures should be taken to avoid excessive tissue and blood vessel dissociation surrounding the CBD. Gentle suturing practices should be adopted, avoiding forceful pulling and clamping. It is recommended to use 4-0/5-0 absorbable sutures or unidirectional barbed sutures, with a needle distance of 1–2 mm, an edge distance of 2 mm, and 3–5 needle sutures. If bile leakage persists, additional sutures should be applied until no obvious leakage is discerned. Our study demonstrated that no significant difference between the two groups in the rate of stone recurrence, consistent with findings reported by Wang et al.28 Recurrence is believed to be influenced by patient genetics, living environment, dietary habits, and previous surgeries. In cases of stone recurrence, ERCP lithotomy is recommended.
The study possesses certain limitations that warrant acknowledgement. The number of cases included in this study is limited, and the follow-up duration is relatively brief. Moreover, being a retrospective analysis, inherent selection biases are unavoidable. Therefore, the findings derived from our study necessitate validation through extensive prospective randomized controlled studies with larger sample sizes in the future.
5 CONCLUSIONS
PDC is suitable for patients with small and fewer stones, particularly those with a CBD diameter within the range of 10–15 mm. Provided that surgical indications are meticulously adhered to, PDC offers superior perioperative outcomes over TTD, facilitating prompt recovery without increasing postoperative complications. Consequently, PDC emerges as a safe and feasible treatment approach for cholecystolithiasis combined with choledocholithiasis.
AUTHOR CONTRIBUTIONS
Da Teng: Conceptualization; formal analysis; validation; writing – original draft. Yue Xu: Conceptualization; formal analysis; writing – original draft. Qingsong Yang: Conceptualization; writing – original draft. Wenjun Zhang: Validation; writing – original draft.
FUNDING INFORMATION
The present study was supported by the Clinical Medical Research Transformation Project of Anhui Province (no. 202204295107020062), Youth Natural Science Foundation of Anhui Medical University (no. 2021xkj084), and Health Research Project of Anhui Province (no. AHWJ2022b120).
ETHICS STATEMENT
This retrospective study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the Affifiliated Chuzhou Hospital of Anhui Medical University (Chuzhou, China). Written informed consent has been obtained from the patient.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data support the current study are available from the contact author upon request.




