Fatal scenario following dental extraction in middle-aged man with history of acquired hemophilia: Employment of surgical tracheostomy and use of FFP and cryoprecipitate to gain patent airway
Key Clinical Message
Acquired hemophilia A can upshot in a life-threatening hemorrhage and airway obstruction. Airway bleeding is a weighty emergency in hemophilia care, necessitating the immediate start of effective hemostatic therapy (porcine factor VIII, the factor eight inhibitor bypassing activity and recombinant factor VIIa) and the decision to undertake proper airway control, such as tracheal intubation and tracheostomy. However, due to the dearth deficiency of effective hemostatic measures we relied upon the use of fresh frozen plasma and cryoprecipitate to gain control of the bleeding despite the precarious threat of infectious disease transmission associated with their use.
1 INTRODUCTION
Hemophilia A is the most common bleeding diathesis, affecting one in every 5000 males and accounting for 80% hemophilia cases.1 Hemophiliacs are 13% more likely to succumb to airway mishaps triggering oropharyngeal hemorrhage with an 8% likelihood of fatal outcome.1, 2
Acute upper airway obstruction is a potentially fatal spectacle. Life-threatening airway loss is seldom stated as a serious ailments of coagulation disorders. Using standard methods like direct video laryngoscopy and flexible fibreoptic intubation to secure an airway may turn futile due ongoing bleeding and airway swelling. Acquired hemophilia is a scarce coagulopathy induced by antibodies to Factor VIII. Acquired hemophilia, like other coagulation diseases, prompts easy bruising, joint, muscle hematoma, and severe bleeding during dental procedures. Airway bleeding is a noteworthy crisis in hemophilia management and demands the immediate transfusion of deficient factor replacement as well as the necessity to execute proper airway control, such as early cricothyrotomy and tracheostomy.1-5
We describe a case of life-threatening upper airway obstruction due to hematoma after tooth extraction in patient with acquired hemophilia A. Despite swiftly developing an airway obstruction and cardiac arrest due to asphyxia, we were able to perform instant airway control and salvage the patient life.
2 CASE HISTORY AND EXAMINATION
A 45-year-old male with history of acquired hemophilia presented to our emergency room with acute shortness of breath and facial swelling for 12 hours following dental extraction by a local paramedic. He is employed as a school teacher and has no other known co-morbidities.
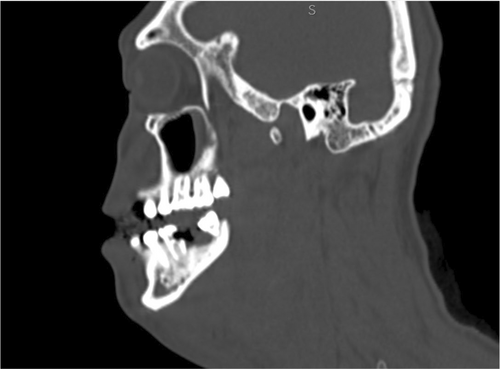
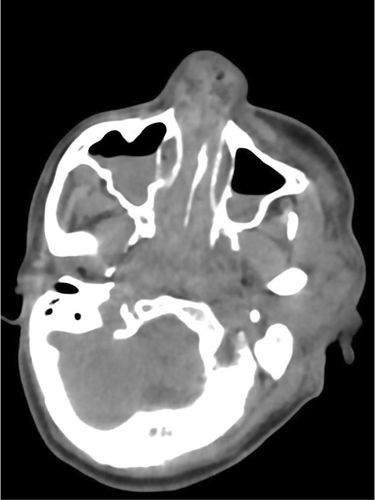
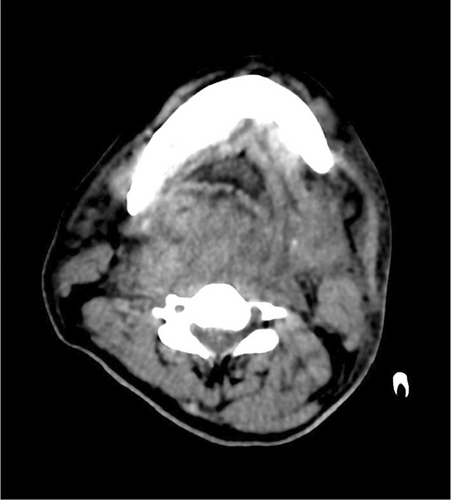
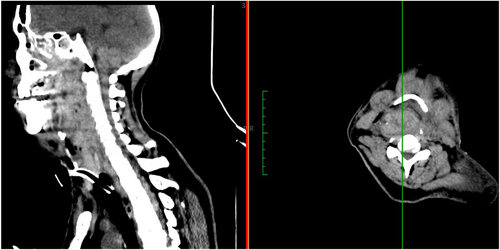
Five minutes after his arrival, while we were evaluating him, he collapsed precipitously and became unresponsive. Carotid was not palpable and cardiopulmonary resuscitation was started immediately, and advanced cardiac support guidelines were followed. Return of spontaneous circulation was evident within 3 minutes with normal sinus rhythm evident in ECG tracings. Mask ventilation was difficult due to the presence of woody hard facial swelling and very minimal mouth opening (Figure 1). Urgent surgical tracheostomy was performed by expert otorhinolaryngologist while patient was being ventilated through mask via self-inflating manual resuscitator bag.

3 INVESTIGATIONS
4 MANAGEMENT
The patient was shifted to intensive care and kept on mechanical ventilation (7 mm cuffed tracheostomy tube). To prevent further expansion of hematoma fresh frozen plasma (FFP) and cryoprecipitate were used due to unavailability of factor VIII. In addition, desmopressin (nasal spray) and tranexamic acid were also administered. Along with hemostatic treatment the patient received broad spectrum antibiotics and supportive measures.
5 OUTCOME
The patient was gradually weaned off the ventilator, resolution of oropharyngeal swelling was almost complete after 12 days of admission. There were no signs of sepsis and the aPPT value fell back to 37 s. He was decannulated on day 14 and shifted out of the ICU after one more day. On discharge, consultation, and follow-up with hematologist was advised.
6 DISCUSSION
Dental extraction can invite potential asphyxiation in hemophiliacs. The hazards of extraction are well recognized by the clinicians and numbers of fatal consequences are recorded in the literature. Death following dental extraction due to respiratory embarrassment in 35-year-old hemophiliac, was published in British medical journal in 1941 by team of Eddicott CL.6 54 h following the extraction, the patient developed stridor and impending respiratory arrest. Tracheostomy was immediately performed to salvage the airway. However, patient succumbed to death due to numerous complications.6 Likewise, death from respiratory obstruction in hemophilia has also been stated by Edmonds AR in medical journal of Australia in the year 1951.7
Severe sublingual and paratracheal hemorrhage in a hemophiliac child during a course of upper respiratory infection was reported by Baird KH in the journal of pediatrics in 1943. The child developed respiratory distress and was recovered following tracheostomy.8 A case of airway obstruction in a hemophiliac patient was documented by Macdonald AC in British medical journal. The case management comprised of blood transfusion, nasotracheal intubation, and submental incision.9
Roderick et al. described a case of hemophilia with factor VIII inhibitors in a 15-year old boy, which culminated into life threatening oro-pharyngeal bleeding. He was managed successfully with porcine factor VIII.10 Similarly, spontaneous onset compressive retropharyngeal hematoma in a 23-year old hemophiliac male has also been outlined in literature by Benhammou et al. Hematoma expanded into floor of mouth resulting into dyspnea, dysphagia, and dysphonia. The patient received proper and effective medical treatment.11
The three approaches for treating the early bleeding in acquired hemophilia A are: porcine factor VIII, the factor eight inhibitor bypassing activity (FEIBA) and recombinant factor VIIa (most effective).3 Treatment with emicizumab has also been suggested in episodes of life-threatening bleeding.2 However, due to unavailability of above-mentioned treatment options, we relied upon the use of fresh frozen plasma, cryoprecipitate, tranexamic acid, desmopressin, and hydrocortisone.
The oral and maxillofacial region comprise a complex anatomy and is highly vascular. Hemorrhage in oral cavity is potentially grave because it induces airway obstruction. In associated scenarios like hemophilia, hemorrhage in airway could result in devastating outcome.4
Failure to achieve control of the airway ensues cardiac arrest due to asphyxia. The crucial management in hemophilia is the early institution of hemostatic measures and airway control.5
In the majority of published cases, impending respiratory arrest resulting from bleeding into the airway in hemophiliacs is managed with tracheostomy and supported by medical management.6, 8 Whereas in some situations with mild degree of airway compromise, only medical management was successful.10, 11 Nasotracheal intubation technique in such scenario is also described by Mcdonald AC.9 In our case, we immediately deployed tracheostomy to rescue airway because of inadequate mouth opening and imminent cannot ventilate and cannot intubate circumstance.
The hemostatic intervention carried in our case differed from the currently accepted standard in management of hemophilia due to economic constraint regarding its acquisition in our set-up. According to study done by Rahaman et al. FFP and cryoprecipitate both are efficacious can be used to correct factor deficiency in hemophilia in resource poor settings. Cryoprecipiate allows rapid correction of factor coagulation factor deficiency and minimizes chances of volume overload, while FFP is easily available and affordable.12
Percutaneous dilatation tracheotomy (PDT) allows intensivists to perform tracheotomies at the victim's bedside and if guided by ultrasound, complications can be reduced. PDT is a modern tracheotomy procedure that is garnering significant popularity on chosen patients, as opposed to the conventional surgical tracheostomy. Ultrasound has a benefit of identifying the crico-thyroid membrane and choosing the location for tracheal puncture when the tracheal anatomy is not immediately perceptible. It also includes details about the structure of the pre and paratracheal region. Ultrasound further helps to identify aberrant vessels, thyroid gland, skin to tracheal distance, and allows selection of appropriate tracheostomy tube. This technique requires significant training and expertise and can be performed by anesthesiologists. If otolaryngologist is not immediately available, intensivist can secure a tracheostomy and may possibly be able to salvage the airway.13
Our article discusses an exceptionally uncommon example of a patient who entirely recovered from cardiac arrest due to asphyxia following tooth extraction. Usual standard routes of intubation (oral and nasal) may be deemed impossible in bleeding airway due to difficulty in visualization of anatomical structures and non-compliant submental, submandibular, retropharyngeal, and parapharyngeal space resulting from hematoma. To gain control of the airway, techniques such as cricothyrotomy and tracheostomy should be performed immediately without hesitation.
7 CONCLUSION
We described our experience treating a hemophilia A patient who developed airway obstruction after dental extraction. Massive airway swelling resulted to asphyxiation and cardiac arrest which was reverted with cardiopulmonary resuscitation. In hemophiliacs hematoma advances drastically, therefore quickly maintaining the airway by tracheotomy under adequate hemostatic therapy must be undertaken. To ensure optimum level of care, collaboration of anesthesiologists otolaryngologists and hematologists is indispensable.
In resource limited areas (unavailability of tests to estimate factor VIII levels, antibody titre, scarcity of specific blood products), the condition can be managed with fresh frozen plasma, cryoprecipitate, and pharmacological agents. FFP and cryoprecipitate carries the potential risk infectious (hepatitis B, hepatitis C, and HIV) disease transmission and is not a standard of care therapy in situation involving serious bleeding in acquired hemophilia.
Amongst poorly developed countries where quackery is still prevalent, cases like ours is not a new surprise. In our case tooth extraction was done in local medical hall by a paramedic. This article emphasizes the importance of history taking, and timely referral to expert.
AUTHOR CONTRIBUTIONS
Sunil Bhatta: Conceptualization; formal analysis; investigation; resources; validation; writing – original draft. Sukriti Pandit: Resources. Sabin Nepal: Resources. Pratik Chaudhary: Resources.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interests.
ETHICS STATEMENT
Ethical approval of case reports is not needed in accordance with local ethical guidelines.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data described to support the findings is openly accessible in the article.




