Anti-PL-12 anti-synthetase syndrome manifesting with multiple digital ischemia: Case report & review of the literature
Abstract
Key Clinical Message
Acute digital ischemia is a rare manifestation of anti-synthetase syndrome in the absence of Raynaud's phenomenon. A high index of suspicion may result in early diagnosis and better clinical outcomes.
A 61-year-old male patient was admitted to the hospital for worsening arthralgias with morning stiffness lasting hours, as well as left sided headaches, and jaw pain while eating. He had significant weight loss and subjective fever at home. Multiple fingers and toes were noted to be ischemic. His laboratory workup was pertinent for significantly elevated inflammatory markers, and mild Creatinine kinase elevation. Chest imaging and later lung biopsy were notable for organizing pneumonia. Conventional angiogram showed evidence of significant digital disease without collaterals. Subsequent autoimmune screening tests with extended myositis-specific and myositis-associated panels revealed a strongly positive anti-PL-12 antibody and moderately positive anti- SSA-52KD IgG ab. After ruling out infectious etiologies and malignancy, anti-synthetase syndrome (ASyS) diagnosis was considered in the presence of ischemic digits, organizing pneumonia, polyarthralgia, constitutional symptoms, increased inflammatory markers and positive antibodies. The patient was treated with high dose prednisone and mycophenolate mofetil along with amlodipine and sildenafil for digital vasodilation. Acute digital ischemia may be the first manifestation of ASyS with ILD. A high index of suspicion is warranted for early diagnosis and better outcomes.
1 INTRODUCTION
Idiopathic inflammatory myopathies (IIM) are a heterogeneous group of autoimmune myopathies that share several overlapping clinical features. Anti-synthetase syndrome (ASyS) is a subtype of IIM with a distinct serological profile characterized by autoantibodies directed against aminoacyl-tRNA synthetase (ARS). The estimated worldwide prevalence of ASyS is 1–9 per 100,000 with females affected nearly twice as often as males.1
Interstitial lung disease (ILD) is a hallmark of ASyS, but phenotypic characteristics of ASyS based on its serological profile also exist. The clinical manifestations with variable prevalence include myositis, peripheral symmetrical arthritis, mechanic's hands, skin rash, panniculitis, pulmonary hypertension, and rarely myocarditis.2 The 10 specific anti-ARS antibodies with a defined clinico-serological entity of ASyS consist of Anti-Jo1, Anti-PL7, Anti-PL12, Anti-OJ, Anti-EJ, Anti-KS, Anti-Zo, Anti-SC, Anti-JS, and Anti YRS. Anti-Jo-1, first recognized and named after the incident patient “John P” in 1982 having features of ILD and myositis, is the most common type of ASyS with a more favorable prognosis.3 Non-Anti-Jo-1 ASyS, in particular anti PL-7 and anti PL-12, portend a worse prognosis. They are associated with rapidly progressive or severe forms of ILD.3 The presence of digital ischemia or gangrene in ASyS is an extremely rare phenomenon. We report a case of Anti-PL12 ASyS presenting with ILD, polyarthralgia, and digital ischemia without Raynaud phenomenon as its initial presentation, a diagnostic challenge given the paucity of such an association found in the literature.
2 CASE HISTORY/EXAMINATION
Sixty-one-year-old male patient with past medical history of hypertension, diabetes mellitus type II, left eye blindness following cataract surgery, glaucoma, and bipolar disorder, was brought to the emergency department (ED) due to worsening of his chronic pain in the hands and feet. The patient reported having arthralgias in the shoulders and hips with morning stiffness lasting hours, as well as left sided headaches, and jaw pain while eating. He had significant weight loss and subjective fever at home. He also reported recurrent falls. He denied any family or personal history of rheumatic diseases. He quit smoking 15 years ago, however reported occasional marijuana use.
In the ED, the patient's vital signs were temperature of 97.8 F, respiratory rate of 20 per minute, oxygen saturation of 98% on room air, blood pressure of 157/92 mmHg and HR 111 bpm. On physical exam, the patient was noticed to be in mild distress. He was alert and oriented to time, place, and person, however mildly somnolent. His head and neck examinations were unremarkable for lymphadenopathy, however the patient had temporal wasting, tenderness over his left temporomandibular joint and had a loose tooth with poor dentition. On chest auscultation, he had reduced breath sounds given poor inspiratory effort. Cardiac and gastrointestinal examinations were unremarkable. He had palpable radial and brachial pulses but weak dorsalis pedis pulses. His right hand was edematous with the fingers being cool to touch and with ischemic changes in the 2nd, 4th, and 5th fingers with diffuse tenderness to palpation. He also had multiple toes with ischemic changes as well (Figure 1). His right shoulder range of motion was limited due to pain. Motor power was 4/5 all over without focal weakness. The skin examination revealed no rash or other lesions.

3 METHODS (INVESTIGATIONS, DIFFERENTIAL DIAGNOSIS, AND TREATMENT)
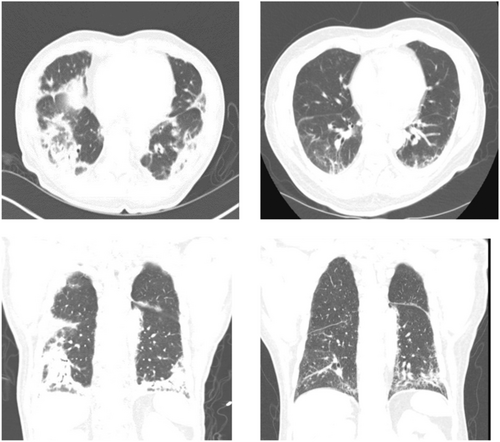
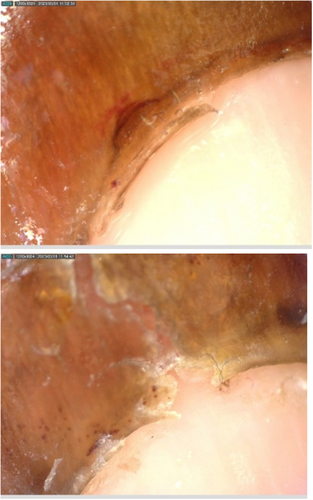
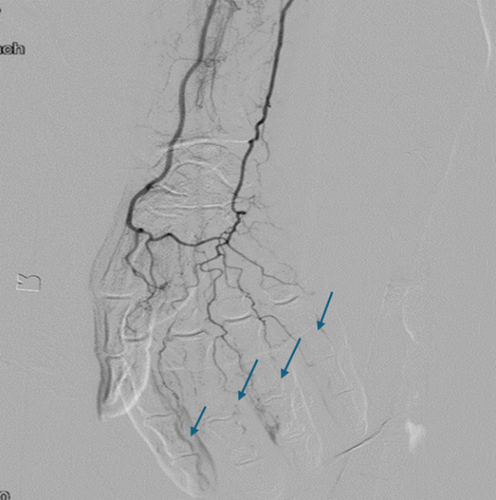
Initial labs (summarized in Table 1) complete blood count showed a white blood cell count of 12.1 (k/cmm) with 90.2% neutrophils, hemoglobin of 12.6 (g/dL) platelet 213(k/cmm). His AST was 40(U/L), albumin 2.4 (g/dL), CK 539(U/L) that normalized with hydration, CRP 153(mg/L), ESR >130(mm/hr), hbA1C of 10.7%, glucose 445, creatinine 1.1 (mg/dL), ferritin of 538(ng/ml), rheumatoid factor of 225(IU/ml), Anti-CCP <0.54(negative), ds DNA, ANA, ANCA, MPO, PR3, C3, C4, TSH, hepatitis B ag, core ab &hepatitis C ab, HIV, syphilis screen, QuantiFERON TB, cryoglobulin, were all negative or within normal limit. Anti-phospholipid antibodies were negative except for minimally elevated IgA ab 11(PL units) (reference range 0–10). SPEP was negative for M-spike with presence of chronic inflammation, factor V leiden mutation, prothrombin gene 20,210 mutation, and homocysteine level were normal. Urine was without blood or protein. Urine toxicology screen was positive for cannabinoids. Blood cultures were negative. Vitamin C was decreased 0.1 mg/dL (0.4–2.0). He had an echocardiography done that did not reveal any vegetations. Xray of the shoulders, hands, hips, and feet did not show inflammatory changes, however, revealed degenerative changes of the hips and shoulders. CTA of the chest showed patent thoracic aorta, without aneurysms or dissection, and bilateral lower lobe infiltrates. (Figure 2) PET-CT revealed multiple mildly enlarged lymph nodes in the bilateral axilla that were mildly FDG-avid, nonspecific, likely inflammatory, with minimal uptake in the patchy infiltrates of the bilateral lower lungs otherwise no malignancy or vasculitis. MRA brain was without evidence of vasculitis. Vascular studies of the arms were with evidence of mild bilateral atherosclerotic disease, multiphasic pedal waveforms, and evidence of significant digital disease bilaterally. He had a right-sided temporal artery biopsy (TAB) given his headache and jaw pain that was negative for arteritis. His Capillaroscopy (Figure 3) revealed a few spots of capillary drop out, microhemorrhages, and dilated capillaries in some digits and a conventional angiogram showed evidence of significant digital disease without collaterals. (Figure 4) The patient also had a bronchoscopy which showed fragments of well-aerated lung parenchyma with focal organizing pneumonia. It was negative for granuloma or neoplasia. Bronchoalveolar lavage cultures for bacteria and fungi were negative. He had 90% mononuclear cells.
| Test | Result on admission | 3 week follow up |
|---|---|---|
| White blood count (k/cmm) | 12.1 | 6.8 |
| Hemoglobin (g/dL) | 12.6 | 10.4 |
| Platelet (k/cmm) | 213 | 286 |
| Albumin (g/dL) | 2.4 | 3.2 |
| AST (U/L) | 40 | 29 |
| ALT (U/L) | 35 | 62 |
| Creatinine (mg/dL) | 1.1 | 0.7 |
| CPK (U/L) | 539 | 76 |
| CRP (mg/L) | 153 | 0.23 |
| ESR (mm/h) | >130 | 23 |
| Ferritin (ng/ml) | 538 | NA |
| Glucose (mg/dL) | 445 | 237 |
| Rheumatoid Factor (IU/ml) | 225 | NA |
| Citrulline antibody | <0.54 (Negative) | NA |
| ANA | Negative | NA |
| ANCA | Negative | NA |
| Cryoglobulin | Negative | NA |
| C3 (mg/dL) | 156 | 119 |
| C4 (mg/dL) | 12 | 28 |
| Hepatitis B antigen | Nonreactive | NA |
| Hepatitis Core total | Nonreactive | NA |
| Hepatitis B antibody | 28.63 | NA |
| Hepatitis C | Nonreactive | NA |
| HIV | Nonreactive | NA |
Upon presentation, there was a suspicion for giant cell arteritis based on the initial clinical presentation and elevated inflammatory markers, hence the primary team started the patient on 1 mg/kg of prednisone.
Subsequent autoimmune screening tests with an extended myositis-specific and myositis-associated panels revealed a strongly positive anti-PL-12 antibody (anti-alanyl t-RNA synthetase) (reference range: negative) and moderately positive anti- SSA-52KD IgG ab 42 units(reference range < 20).
Therefore, after ruling out infectious etiologies and malignancy, ASyS diagnosis was considered in the presence of ischemic digits, organizing pneumonia, polyarthralgia, constitutional symptoms, increased inflammatory markers and positive antibodies.
Mycophenolate mofetil was added at 500 mg twice daily and was later increased to 1 g twice daily. He was also started on amlodipine and sildenafil for digital vasodilation.
4 OUTCOME AND FOLLOW UP
At 3 weeks follow-up in the clinic, he continued to have gradual improvement of his symptoms and his inflammatory markers normalized with CRP down to 0.23 mg/L & ESR 23 mm/hr. His albumin improved to 3.2 g/dL and repeat CT chest showed overall improved aeration within the lower lobes. He later underwent right 2nd and left 1st and 2nd toe amputation that was complicated by pseudomonas aeruginosa osteomyelitis, and he also had dry gangrene in the 2nd and 4th fingers distally in the right hand on follow up. (Figure 5).

5 DISCUSSION
The etiology of digital ischemia is broadly categorized into atherosclerotic, thromboembolic, vasculitic, vasospastic, traumatic, or compressive factors. Digital gangrene is a known complication of many rheumatic diseases like systemic sclerosis (SSc), antiphospholipid syndrome, systemic lupus erythematosus, vasculitis,4 juvenile dermatomyositis and other interferonopathies like STING-associated vasculopathy with onset in infancy (SAVI).5 Mechanisms for ischemia include intense vasospasm, severe atherosclerosis, endothelial inflammation, intimal fibrosis, and/or hypercoagulability or overlap of these conditions.4 Digital gangrene has been seldom reported with inflammatory myopathies such as ASyS in the absence of other co-existing rheumatic diseases. In review of the literature, we found nine cases of ASyS without overlap with another autoimmune disease.6-14 Anti-PL7 and anti-PL12 were the most common anti-synthetase antibodies seen in these cases. Anti-PL12 has previously been described as having higher rates of Raynaud's phenomenon and vascular involvement compared to those with Anti-Jo-1 antibodies.6 Of the reported cases, only one case described the development of digital gangrene as the first presenting symptom with later manifestation of ILD and other typical syndrome findings.6 Another report described an initial presentation of classic signs of myalgia and weakness with Raynaud's phenomenon and the subsequent development of digital ulceration and gangrene later in the course.8 Patients' characteristics, disease manifestations, and type of ASyS previously reported have been summarized in Tables 2 and 3. Our patient's acute digital ischemia is likely related to ASyS with polyarthralgia and findings of organizing pneumonia, a subtype of ILD. He had no evidence of cardiac arrhythmias or structural heart disease with normal findings on echocardiography. Medium to large vessel vascular disease was ruled out with normal computed tomographic angiography (CTA) and conventional angiogram showed evidence of significant digital disease without collaterals as previously reported in a few cases of ASyS.10-12 Several reports of cannabis induced arteritis have been published over the years.15 The exact mechanism, although partially understood, is believed to be a subtype of thromboangitis obliterans (TAO) which is a chronic, non-atherosclerotic, nonimmune inflammatory arteritis of the extremities. Our patient did report occasional use of cannabis but the acute presentation of ischemia with concomitant finding of biopsy proven noninfectious organizing pneumonia, positive serology for ASyS, and the lack of characteristic imaging appearance of TAO that is often seen with cannabis arteritis strongly suggests anti-synthetase syndrome as the underlying etiology of the digital ischemia.
| Author reference | Age/Gender | Comorbidities | Antibody | Clinical presentation | Nail Capillaroscopy | CT chest/ Angiography | Immunosuppression/Vasodilator |
|---|---|---|---|---|---|---|---|
| 14 | 39/F | None | Anti-PL12 | Arthralgias in both knees, Raynaud's phenomenon, muscle weakness, shortness of breath | Dilated blood vessels and hemorrhaging in periungual and cuticular bleeding | Bilateral interstitial pulmonary infiltration/ None | Prednisolone/none |
| 6 | 77/F | Coronary artery disease, diverticulosis, hypertension | Anti-Ro, Anti-PL12 | Painful, blue discoloration in her bilateral fingertips and occasional fever, bilateral pulmonary infiltration | Not performed | Florid interstitial lung disease /None | Cyclophosphamide/none |
| 7 | 69/F | None | Anti-PL12 | Malaise, anorexia, weight loss, ILD | flame shaped hemorrhages and dilated capillaries at proximal nail folds | interstitial lung disease/None | Cyclophosphamide/vosentan |
| 8 | 71/M | None | Anti-PL12 | General malaise, muscle pain and weakness, fever | No changes | Interstitial pneumonia/None | Prednisolone/ limaprost alfadex |
| 11 | 50/F | Interstitial lung disease | Anti-PL12 | Fever, myalgia, chilblains-like lesions, cough | Pericapillary edema, dilated loops, microhemorrhages, and disorganization of capillary architecture with a nonspecific pattern. | Subpleural ground-glass opacities, compatible with interstitial lung disease/None | Methotrexate, Steroid/none |
| Author Reference | Age/Gender | Comorbidities | Antibody | Clinical presentation | Nail Capilloscropy | CT Chest/Angiography | Immunosuppression/Vasodilator |
|---|---|---|---|---|---|---|---|
| 10 | 60/M | Type II Diabetes Mellitus, tuberculosis, lymphadenitis | Anti-PL7 | ILD, painful digits | Dilated nail-fold capillaries; bleeding, ragged, hyperkaratotic cuticles | Diffuse ground glass opacities in the bilateral lower lobes/ distal occlusions at the bilateral 2nd to 5th MCP joints, no proximal arterial occlusions were found | Mthylprednisolone, cyclophosphamadie |
| 12 | 61/F | Hypertension, Vitiligo, Major Depressive Disorder, Interstitial Lung Disease | Anti-PL7 | Finger pain in distal interphalangeal joints, dry cough, ILD, no arthritis or myositis | Not performed | Ground-glass opacities consistent with ILD were seen in bilateral lower lobes/ bilateral fixed occlusive vasculopathy of the digital arteries | Prednisone + MMF |
| 13 | 66/F | Ischemic Heart Disease, Cardiomyopathy, Celiac disease, Obstructive Sleep Apnea, Dermatitis Herpetiformis | Anti-EJ-1 | Dyspnea, fever, dry cough, proximal muscle weakness, cryptogenic organizing pneumonia | Not performed | Bibasilar predominant reticular thickening with subpleural involvement, evidence of honeycombing and traction bronchiectasis in keeping with a usual interstitial pneumonia (UIP)/none | Prednisone + MMF + Induction Rituxmab |
| 9 | 33/F | None | Anti-Jo1 | Ulceration and pain in the digits, chills, numbness of the fingers, discoloration of the hands, arthralgia, morning stiffness up to 1 hours, fever, weakness in muscles, increased fatigue and insomnia | Not performed | Bilateral opacities/none | Steroids, cyclophosphamide, mepolizumab, IVIG, rituximab, nintedanib / vasoprostane, iloprost, doxazosin, sildenafil |
The immunopathogenesis of ASyS is partially understood. ARS are enzymes responsible for the pairing of tRNA messenger with their cognate amino acids for protein synthesis. In vitro studies have shown the noncanonical function of histidyl-tRNA synthetase (JO-1) with chemokine properties that attract lymphocytes, activated monocytes and dendritic cells into the target organs.16 There is some evidence that ARS are secreted out of cells (aaRSs, HisRS, ThrRS, GlyRs, TyrRs, and AsnR) during tissue damage, angiogenesis, and in some cancers. Neutrophil extracellular trap (NET) formation has been a proven immune mechanism for generation of autoantibodies.16 Increased levels of LL-37, a biomarker of NET-osis, have been detected in patients with ASyS, suggesting a role of such a mechanism for autoantibody formation against these enzymes. Finally, the crosstalk between innate and adaptive immunity has been shown to illicit the immune response triggered by the extra-cellular presence of ARS.17-19 However, the pathological role of autoantibodies directed against ARS remains elusive.
The hypothesis of endothelial inflammation, microangiopathy, or intense vasospasm in the digital arteries of patients with ASyS as previously reported11 is derived from mechanisms seen in other rheumatic diseases associated with digital ischemia. Most of the patients with digital ischemia and dermatomyositis are associated with scleroderma (SSc) overlap,12, 19 which is a type-1 interferonopathy. The presence of nail-fold capillary changes seen in some of the cases closely mimics SSc like patterns. In a systematic review of digital ischemia reported in ASyS patients, a total of 9 out of 19 cases either had a scleroderma phenotype or DM/Ssc overlap.20 Moreover, the higher interferon signature was not elucidated in ASyS compared to other types of inflammatory myopathies in a few studies,21 whereas other investigators showed that immune complexes containing anti-Jo-1 with their target RNA may act as inducers of type I IFNα in ASyS.22 It is noteworthy that some of the reported ASyS patients had digital ischemia without preceding history of cutaneous ulcers or Raynaud's phenomenon (RP)11 similar to our patient. A large multicenter cohort study by Sebastiani et al. showed that the presence of anti-Jo-1 was positively associated with the presence of SSc-like features on nail capilloroscopy.23 Interestingly, no significant correlation between the presence of SSc-like pattern and RP was shown. These findings argue in favor of different microangiopathic phenotypes of ASyS along with different mechanisms responsible for RP, and possibly digital ischemia in these patients.
Given this rare association, the management of digital ischemia in ASyS is largely clinician or center based. The use of imaging and conventional angiograms is not frequently utilized. The findings of imaging and therapeutic utilization are summarized in Tables 2 and 3. The most common immunosuppression used in these patients was high dose prednisone in combination with cyclophosphamide or mycophenolate mofetil owing to the presence of severe ILD. The use of various vasodilators such as calcium channel blockers, phosphodiesterase five inhibitors, prostacyclin agonists, and endothelin antagonists were reported with variable success in these cases. These treatments are often administered for progressive or refractory Raynaud's phenomenon with a threatened digit. The immediate use of anticoagulation was also not reported in the majority of cases prior to ruling out thrombosis on imaging. Our patient had well demarcated gangrene without evidence of Raynaud's phenomenon. After ruling out thrombosis, we used a combination of amlodipine with sildenafil and mycophenolate in addition to high dose steroids for his ILD. Patient had improvement in the digital pits on the contralateral hand without any progression of his well-demarcated digital gangrene (Figure 1).
This case emphasizes the heterogeneous nature of serological subtypes of ASyS with the involvement of various organ systems, and very rarely the digital vasculature, which can pose a great diagnostic challenge for clinicians. The underlying immunopathogenesis in ASyS is an evolving field and future studies may address the mechanisms responsible for digital ischemia in these patients. ASyS maybe suspected in patients presenting with acute digital gangrene in the absence of another diagnosis in order to foster early intervention with immunosuppression and vasodilators.
6 CONCLUSION
Acute digital ischemia may be the first manifestation of ASyS with ILD. A high index of suspicion is warranted for early diagnosis and better outcomes.
AUTHOR CONTRIBUTIONS
Sarah Abi Doumeth: Conceptualization; data curation; formal analysis; writing – original draft. Emily Petrinec: Writing – original draft. Haseeb Chaudhary: Conceptualization; data curation; formal analysis; methodology; supervision. Maya Mattar: Conceptualization; supervision; validation.
FUNDING INFORMATION
This study was funded by the OHIOLINK CY24 - Case Western Reserve University.
CONFLICT OF INTEREST STATEMENT
None.
CONSENT
A written informed consent was obtained from the patient to publish this case report. Patient gave permission to use the clinical information and photographic material. All patient identifiers have been removed.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.




