Diagnostic uncertainties in congenital syphilis: A case report
Key Clinical Message
Congenital syphilis is a forgotten disease, and often misdiagnosed. It can present with a myriad of clinical features, mimicking various other conditions therefore posing difficulty in diagnosis. Patient may be born preterm with low birth weight, failure to thrive with hemolytic anemia, thrombocytopenia, and leukocytosis. It is a treatable condition, commonly treated with penicillin or ceftriaxone.
1 INTRODUCTION
Congenital Syphilis is caused by organism Treponema pallidum which is transmitted in newborns vertically from their mothers or through maternal lesion at the time of delivery. Untreated syphilis during pregnancy has a transmission rate close to 100% and causes fetal or perinatal death in 40% of affected infants.1 Recent estimates indicate that congenital syphilis is the second leading cause of preventable stillbirths worldwide.2 This condition can have numerous and complex symptoms that resemble other diseases. With the presentation often mimicking other conditions like skin rash, hemolytic anemia, paralysis of limbs, neurological manifestations.2 After the advent of penicillin treatment in the 1940s, the incidence of syphilis had shown dramatic decrease. However, according to recent WHO report, the incidence of congenital syphilis is rapidly increasing all over the world with 700,000–1.5 million cases reported annually between 2016 and 2023.3 However due to widespread antenatal screening programs and penicillin treatment of mothers, the cases of congenital syphilis in rarely suspected and confirmed these days.
We report a case of congenital syphilis in hospital delivered newborn with adequate maternal antenatal checkup and presented with unusual hematological presentation along with skin lesion.
2 CASE PRESENTATION
2.1 Case history/examination
An infant, born at 31 weeks of gestation with a birth weight of 2250 gm, presented at 43 days of life with bilateral lower limb swelling for 10 days and peeling of skin on the lower limbs and buttocks for 8 days. The baby was born to 26 years old apparently healthy women with proper antenatal checkup and was delivered at a maternity hospital in Nepal. There was no redness or decreased limb movement and the swelling spontaneously subsided after 2 days. The infant was on exclusive breastfeeding but was unable to gain weight. Rather, his weight had decreased to 1700 g for which baby was taken to a nearby hospital where he was investigated for sepsis and found to have a positive septic screen and dilated bowel loops on x-ray abdomen. The infant had significantly hemoglobin of 5.9 g/dL and received two pints of blood transfusion. He was started on meropenem and vancomycin and was referred to our center with a provisional diagnosis of necrotizing enterocolitis with late onset neonatal sepsis.
2.2 Method (Differential diagnosis, investigation, and treatment)
When baby arrived to our center, he had ichthyic skin on the lower limbs with swelling of limb (Figure 1) and palpable liver 2 cm below the coastal margin. Blood tests showed anemia (Hb:8.3). The total leucocyte count was 40,000/mm3 with neutrophilic predominance, and Thrombocytopenia (Platelets: 70,000) was also present. His corrected reticulocyte count was 8% with a positive direct Coombs test (DCT). Peripheral blood smear showed anisocytosis, normocytic normochromic RBC with hypochromic red cells. Liver enzymes were also elevated.

As baby was preterm, low birth weight and was failing to thrive with hemolytic anemia, thrombocytopenia, TORCH infection was suspected. TORCH ELISA and RPR (Rapid Plasma Reagin) screen were sent, revealing a reactive RPR titre (1:64). Due to unavailability of crystalline penicillin, treatment with ceftriaxone was started.
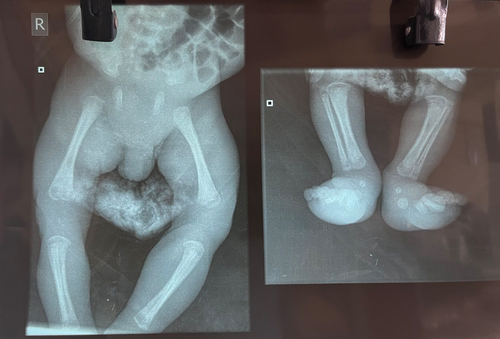
CSF analysis was normal and CSF VDRL was negative. (Table 1) An x-ray of bilateral lower limbs revealed diffuse peri osteitis involving bilateral femur, tarsals, and metatarsals with destruction in evaluations were normal (Figure 2) The parents were treated accordingly with benzathine penicillin. After 2 weeks of treatment, the infant showed symptomatic improvement along with normal counts. (Table 2).
| Test | Value | |
|---|---|---|
| RPR | Reactive (1:64) | Carbon particle flocculation |
| TORCH IgM ELISA | ||
| Toxoplasma gondii | Negative | |
| Rubella virus | Negative | |
| Cytomegalo virus | Negative | |
| Herpes simplex virus I | Negative | |
| Herpes simplex virus II | Negative | |
| TORCH IgG ELISA | ||
| Toxoplasma gondii | Negative | |
| Rubella virus | Negative | |
| Cytomegalo virus | Negative | |
| Herpes simplex virus I | Negative | |
| Herpes simplex virus II | Negative |
| Test | Value | Ref range |
|---|---|---|
| TLC | 16,000 | 4000–11,000/cmm |
| Neutrophil | 65 | |
| Lymphocyte | 29 | |
| Monoctye | 05 | |
| Eosinophil | 01 | |
| Basophila | 00 | |
| Hemogolobulin | 8.3a | 12–18 g/dL |
| PCV | 24.8a | 36–54 |
| RBC | 2.48a | 4.5–5.5 million/cc |
| Platelets | 70,000a | |
| MCV | 100 | 82–92 fl |
| MCHC | 33.47 | 27–42% |
| MCH | 33.47 | 27–32 pg |
| AST | 149 | 0–5 |
| ALT | 57 | 0–50 |
| Alkaline phosphatase | 139 | 30–120 |
- Note: Bold values indicates high levels.
- a Indicates lower level.
3 DISCUSSION
Recognition of congenital syphilis is often challenging as clinical features are non-specific and variable. Most infants are asymptomatic at birth and may present only after several weeks to months of life.4 Negative VDRL report of mother during antenatal screening might be deceptive many a times. In our case also, the mother had been screened negative for serological evaluation of HIV, Hepatitis and RPR test during her first Antenatal Care (ANC) visit. Hence, we could not consider syphilis in our list of differentials during the initial assessment of the patient. Similar case reports of near miss of diagnosis due to first trimester screening being negative has been reported.5 With our case it has been further highlighted that physician need to be aware that syphilis can also be acquired at a later stage after antenatal screening. In areas of high incidence, a three-time points testing has been recommended: at the first visit, in the third trimester and at delivery by Center for Disease Control and Prevention (CDC). CDC recommendation also includes testing for syphilis in all women with fetal death after 20 weeks of gestation.6
Syphilis often has variable consequences during pregnancy and in the post-natal period affecting different systems of the body. Untreated syphilis during pregnancy has a transmission rate close to 100% and causes fetal or perinatal death in 40% of affected infants3 While there were few classical points in favor of congenital syphilis in our case, some of the presentations were contrary to the usual clinical picture. The points contrary to the usual findings were, the DCT being positive in our case. The usual findings are that of DCT negative hemolytic anemia. The positive DCT was more suggestive of autoimmune causes of hemolytic anemia and hepatomegaly. While autoimmune hemolytic anemia is rare after neonatal period, there has been reports of autoimmune hemolytic anemia in early days of life, with preceding infection.5 The patient presented to us during the coldest days of the year, making paroxysmal cold hemoglobinuria (PCH) another possibility. PCH is a complement mediated intravascular hemolysis, where antibody attaches to red cells at colder temperatures and causes red cell lysis when blood recirculates to warmer temperatures. The condition has also been associated with young children after a viral illness and congenital too.6, 7 However, the diagnosis of PCH could not be confirmed due to unavailability of Donath Landsteiner antibody test which is considered as pathognomic for the diagnosis.
While there have been reports of peeling of skin in association with congenital syphilis in few reports, the more common skin manifestation is that of maculopapular rash with small, initially red or pink spots8 These lesions found on the back, buttocks, posterior thighs, palms, and soles. These rashes usually persist for 2–3 weeks and then desquamate and forms crust. It fades to becomes copper color. Our patient present with desquamation without the initial maculopapular rash. While congenital syphilis was among our differentials, we did not conclude the case after the positive RPR report in the patient. Since the clinical scenario was also suggestive of autoimmune causes, with hemolytic anemia and deranged liver function, we speculated that the positive RPR could be false positive due to autoantibody as neonatal lupus.9 Only after positive results in the mother was the definite diagnosis of congenital syphilis made. The gold standard treatment of congenital syphilis is with penicillin. Ceftriaxone is an alternative especially in cases with allergy to penicillin.4 Due to unavailability of crystalline penicillin, we decided to start treatment with ceftriaxone to complete a 14-day course.
4 CONCLUSION
Syphilis involves most part of the body, with numerous and complex manifestations making diagnosis difficult. As has been reiterated with our case, syphilis is indeed “the Great Imitator.” Untimely diagnosis can have grave neurological and developmental consequences and thus congenital syphilis has to be one of the differentials in an infant with active infection and unidentified skin lesion.
AUTHOR CONTRIBUTIONS
Niharika Khanal: Writing – original draft. Jasmine Shakya: Supervision. Vivek Karn: Supervision. Srijana Basnet: Conceptualization. Daman Raj Paudel: Supervision. Sunita Tamang: Supervision.
FUNDING INFORMATION
No funding received.
CONFLICT OF INTEREST STATEMENT
Authors have no conflict of interest to declare.
ETHICS STATEMENT
Ethical approval does not imply to case reports from institutional IRB.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
All the data was available in the manuscript itself.