Lumbosacral tuft of hair as a key stigma for early detection of occult spinal dysraphism: A case report of diastematomyelia with tethered cord in a newborn
Key Clinical Message
Early detection of occult spinal dysraphism, such as diastematomyelia with tethered cord, is vital to prevent neurological damage. Though rarely diagnosed in the neonatal period, cutaneous stigmata can aid early identification. Utilizing neonatal ultrasound enables timely management and multidisciplinary intervention.
1 INTRODUCTION
Spinal dysraphism includes a broad spectrum of congenital malformations resulting from defects in the complex development of the fetus along the spinal axis between the second and sixth weeks of gestation. The lumbosacral region is the most common site for these spinal abnormalities. Spinal dysraphism is categorized into two types: closed and open. In the closed type, the neural elements are covered by intact skin, known as occult spinal dysraphism. Diagnosing occult spinal dysraphism in the neonatal period is challenging from a clinical perspective, as it is less apparent at birth.1
In some cases, the identification of various cutaneous stigmata on the spine, such as abnormal hair tufts, sinus openings, or skin hemangiomas, may prompt suspicion of occult spinal dysraphism.2 Early detection of spinal dysraphism is crucial to prevent irreversible consequences like neurological damage. The presence of cutaneous stigmata enables the early identification of spinal dysraphism.3, 4 Diastematomyelia is a rare congenital malformation of the spinal cord characterized by the division of the spinal cord into two parts, and it is classified within the occult spinal dysraphism group. The divided cord is separated by a septum, and diastematomyelia is considered a neuro-orthopedic syndrome. Clinical manifestations of diastematomyelia include neurological disorders such as back pain, muscle atrophy, loss of sensation, paresthesia, bowel and bladder dysfunction, paralysis, or orthopedic disorders. This condition is typically diagnosed in childhood or adulthood.5, 6 Diastematomyelia is rarely linked with tethered cord syndrome, a condition in which the spinal cord is abnormally attached to tissue within the spinal canal instead of being free-floating.7
Neuroimaging of the spinal axis plays a crucial role in the diagnosis and classification of spinal dysraphism abnormalities.1 We present a case of occult spinal dysraphism in a newborn with a tuft of hair in the lumbosacral region, where we successfully utilized ultrasound imaging to detect the condition and identified the simultaneous presence of diastematomyelia with tethered cord.
2 CASE PRESENTATION (CASE HISTORY/EXAMINATIONS)
A 3-day-old female patient was referred to the neonatal clinic of our institute due to the presence of a sizable hairy midline patch in the lumbar region.
The patient was delivered via cesarean section at 39 weeks of gestation to a 25-year-old mother. She weighed 3200 g at birth, measured 49 cm in length, and had a head circumference of 34 cm. She was the first child of nonconsanguineous parents. The pregnancy was uneventful, and the mother did not consume any drugs. Upon examination, a 5 × 4 cm area of hypertrichosis with dark terminal hairs was observed over the lumbosacral region (Figure 1). Further physical examinations did not reveal any abnormal findings, and the neonate's neurological examinations were within normal limits. The neonate displayed activity and alertness, with spontaneous movement observed in all four extremities.

3 METHODS (DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS AND TREATMENT)
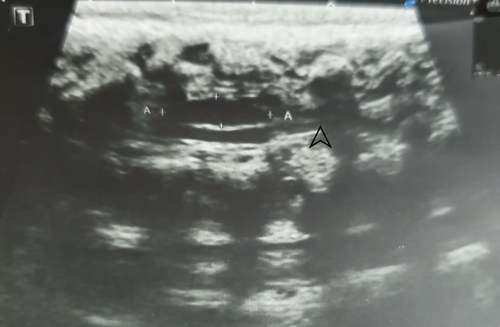
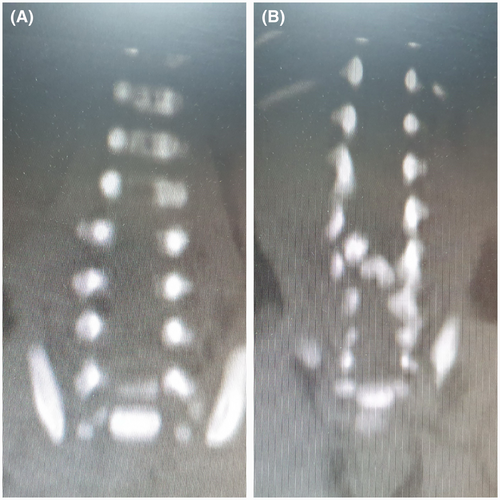
An ultrasound of the spine revealed a defect in the area of the posterior vertebrae, indicating occult spina bifida. Additionally, the ultrasound displayed a split view of the spinal cord at the L2–L3 level, suggesting diastematomyelia. The conus medullaris was observed at the level of the L2–L3 intervertebral disc, displaced dorsally, with no oscillation or movement of the spinal cord, indicative of a tethered cord (Figure 2). Brain sonography yielded normal results. An MRI of the spine was conducted to ascertain the type of split cord malformation. Diastematomyelia was identified at the L3 level, where the spinal cord bifurcated into two hemi-cords with a low-lying tethered cord (Figure 3). The diagnosis of diastematomyelia, coupled with a tethered cord, was established, and the neonate was referred to the neurosurgery department for evaluation. The neurosurgery team did not prescribe any specific treatment during the neonatal period, instead advising regular and periodic follow-ups to monitor the condition and assess the need for future interventions.
4 RESULTS (OUTCOME AND FOLLOW-UP)
It was advised to the parents of the neonate to undergo regular periodic follow-ups at a high-volume referral center with extensive experience in managing these patients.
5 DISCUSSION
Diastematomyelia refers to the vertical division of the spinal cord into two halves and is classified as a type of occult spinal dysraphism. Various theories exist regarding the embryological origins of this cord-splitting malformation. The unified theory of embryogenesis posits that all forms of spinal dysraphism stem from a shared mechanism of embryonic development, involving the formation of adhesions between the ectoderm and endoderm. These adhesions give rise to an endomesenchymal tract that divides the developing notochord.5
Spinal dysraphism is three times more prevalent in females than in males, with clinical symptoms typically manifesting between the ages of four and six.8, 9 The lumbar region is more predisposed to spinal dysraphism compared to the cervical or thoracic regions.5
Certain surface markers on the body can suggest the presence of spinal dysraphism. Localized hypertrichosis on the spine is considered one of the most reliable indicators of spinal dysraphism.5 It has been documented that vertebral, renal, rectal, and uterine abnormalities are associated with spinal dysraphism.10
In our patient, the prenatal diagnosis was overlooked, even though prenatal diagnosis is feasible and crucial for offering options such as early screening, treatment, or termination of pregnancy in the presence of other abnormalities.4 This highlights the importance of prenatal awareness regarding spinal cord anomalies.5 The fetal image is very important in early and accurate diagnosis of spinal pathologies. This makes it possible to plan for appropriate therapy, which enhances the functional results. Ultrasound is mostly used as a screening tool for evaluating the fetal spine, but MRI has become an extremely useful diagnostic tool in complicated cases due to its excellent differentiation between soft tissues and good visibility in any conditions. These methods are complimentary to each other because MRI provides more detailed information about vertebral defects in addition to associated abnormalities of brain that may not be detectable by ultrasound only.11
Following birth, the identification of lumbosacral skin hair tufts during the newborn examination served as our indicator to suspect occult spinal dysraphism. Early detection of occult spinal dysraphism can indeed help prevent irreversible neurological damage.12 Therefore, the assessment of the spine and lumbosacral region is a routine and crucial component of the physical examination of newborns.13 Nevertheless, the majority of published data on skin markers of occult spinal dysraphism originate from neurosurgery, radiology, or dermatology clinics across various age groups, rather than being documented by neonatologists or pediatricians during the neonatal period.12 This highlights the significance of observing skin markers during the examination of newborns.
Hatipoglu et al.14 documented a case involving a 2.5-year-old girl with recurrent bacterial meningitis. The girl exhibited an indeterminate tuft of hair in the occipital region, which was diagnosed as an occipital cephalocele with the uncommon presentation of a tuft of hair. Hamidi and Foladi15 documented a case involving an adult presentation of diastematomyelia and tethered cord, which was initially missed and resulted in unnecessary spine surgery.
In our case, we utilized spinal ultrasonography as the initial diagnostic modality. Ultrasonography proves to be an efficient and noninvasive method for assessing the spinal cord during the neonatal period, given the absence of ossification in the posterior elements of the spine.16 However, many indications for employing spinal ultrasound are linked to a low diagnostic yield.17 The primary limitation in occult spinal dysraphism is the feasibility of conducting ultrasound within the restricted timeframe of the first 6 months of life.1, 9 Our findings indicate that spinal ultrasound can serve as a viable option for the initial screening of newborns exhibiting high-risk back cutaneous stigmata.1 While MRI has traditionally been considered the gold standard for imaging infants with suspected spinal abnormalities, advancements in high-frequency ultrasound scanners with new generators have led to a notable enhancement in the quality of ultrasound imaging in recent times.16
When and how clinical manifestations develop or worsen in occult spinal dysraphism is unknown. There is considerable debate regarding whether surgery should be conducted before or after the potential onset of symptoms. Additionally, the surgical approach for occult spinal dysraphism is a topic of contention. Neurological, urological, and orthopedic symptoms typically manifest gradually, but the emergence of clear and symptomatic indications may signify significant deterioration, with surgical intervention offering only partial improvement. Consequently, the management of children with occult spinal dysraphism is a critical concern that extends into adulthood, aiming to prevent the advancement of clinical symptoms into irreversible conditions.3
The multidisciplinary team approach is a recognized practice for open cases of spina bifida. However, this approach does not currently include closed spina bifida due to the unclear clinical presentation and ongoing debate regarding appropriate management strategies.3, 18 The management of symptomatic split cord syndrome or tethered cord involves surgical intervention. The goal of treatment is to release the spinal cord, enabling it to move freely in conjunction with the spine's movements.5 Mahishma et al.5 reported a rare case involving diastematomyelia with a syrinx and tethered cord in a newborn; however, no details were provided regarding the type of surgery performed or the patient's outcome. Research on children diagnosed with tethered cord and later receiving adult intervention from a neurosurgical service revealed that early diagnosis and prompt intervention are crucial pillars of management. A multidisciplinary approach is considered essential for achieving favorable outcomes.7
The early detection of tethered cord and spinal cord dysraphism facilitates improved patient monitoring and early intervention prior to the onset of severe symptoms and complications. Unfortunately, the unavailability of MRI with the required technique and optimal resolution hindered our ability to ascertain the precise type of diastematomyelia. Additionally, the lack of patient referral impeded further follow-up.
6 CONCLUSION
The presence of midline cutaneous stigmata, such as tuft of hair in a newborn is a sign of spinal dysraphism and needs to be diagnosed early with accurate imaging like ultrasound or MRI. Early diagnosis of dysraphism is important to prevent sequelae especially in conditions like tethered cord syndrome which can cause neurological problems. Advanced neuroimaging especially in fetal and prenatal period including MRI is key to diagnosis and management of spinal dysraphism.
AUTHOR CONTRIBUTIONS
Roya Farhadi: Conceptualization; data curation; project administration; supervision; writing – original draft; writing – review and editing. Seyed Amir Kazemi: Data curation; resources; writing – review and editing. Farnaz Godazandeh: Data curation; investigation; visualization; writing – review and editing.
ACKNOWLEDGMENTS
The authors have nothing to report.
FUNDING INFORMATION
We received no funding for this case report.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICAL APPROVAL
Ethical approval for this report was provided by the Research Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran on 19 November 2023. (IR.MAZUMS.REC.1402.18895).
CONSENT
Written informed consent was obtained from the patient's parents.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this report are available from the corresponding author, upon reasonable request.




