Isolated unilateral ptosis as a complication of sinusitis: A case report and literature review
Abstract
Key Clinical Message
Ptosis associated with rhinosinusitis may indicate orbital or cavernous sinus involvement, typically accompanied by various other symptoms. However, isolated ptosis is a rare occurrence. This explains the diverse treatment approaches found in this literature review, ranging from conservative management to surgery. Imaging plays a crucial role in diagnosis and treatment planning.
Isolated upper lid ptosis is a rare manifestation of acute rhinosinusitis, typically occurring without other neuro-ophthalmological or orbital signs. This report presents a case of unilateral isolated ptosis in an adult male with acute rhinosinusitis. A 30-year-old male with asthma and bipolar disorder, and recent intranasal drug use, presented with nasal congestion, facial pressure, headache, and left eye droopiness. Neurological examination found left ptosis as the only abnormality. Lab results were normal, and COVID-19 PCR was negative. Imaging showed pansinusitis without complications. The patient received IV antibiotics and steroids, followed by oral antibiotics and steroids. Ptosis resolved within 3 days and did not recur at three-month follow-up. Only seven cases of isolated ptosis with rhinosinusitis have been reported, all in males, most recovering with medical therapy alone. This is the first case treated with high-dose steroids in addition to antibiotics. Isolated ptosis may be due to inflammation of the oculomotor nerve's distal branch or related muscular structures. Isolated ptosis in rhinosinusitis has a favorable prognosis. Imaging is crucial to exclude severe complications. The role of steroids needs further evaluation, and the timing for considering surgery remains to be defined.
1 INTRODUCTION
Orbital manifestations of acute sinusitis can range from mild preseptal cellulitis to cavernous sinus thrombosis posing significant risk of vision loss, stroke, or death. These complications typically present with a variety of neuro-ophthalmological symptoms, including pain, fever, vision changes, and restricted eye movements. However, it is exceedingly rare for upper lid ptosis to occur in isolation without any accompanying neuro-ophthalmological findings or other orbital signs, such as proptosis or ophthalmoplegia.1 In this report, we present a unique case of a 30-year-old male who developed unilateral isolated upper lid ptosis in the context of acute rhinosinusitis. This case is particularly noteworthy due to the absence of other symptoms commonly associated with orbital involvement in sinusitis, highlighting the need for careful clinical and radiological evaluation in similar presentations.
2 CASE HISTORY/EXAMINATION
Our case subject is a 30 years old male patient with a history of asthma and bipolar disorder. He admits recent intranasal drug use. He presented to the emergency room for 2 days history of nasal congestion, facial pressure and headache as well as left eye droopiness.
Neurologic exam by a neurologist found the left ptosis to be the only cranial nerve abnormality.
3 DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS, AND TREATMENT
The differential diagnosis included orbital and intracranial complications of rhinosinusitis.
Labs were within normal, WBC = 8.95 k/uL and 71.9% neutrophils.
COVID PCR test was negative.
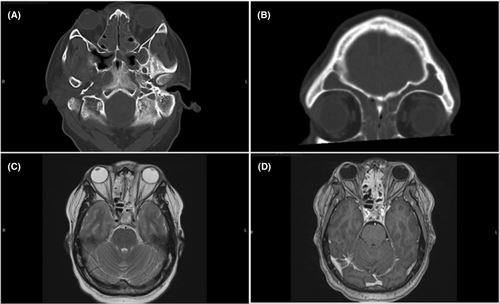
CT scan of the sinuses showed pansinusitis without orbital complications. MRI showed no evidence of intracranial or orbital extension and normal cavernous sinus (Figure 1). No abnormality seen along the course of the left oculomotor nerve.
The patient was admitted for IV Ampicillin-Sulbactam 3 g once followed by 1.5 g q6h and Dexamethasone 10 mg IV stat followed by 4 mg, one tablet every 6 h.
4 OUTCOME AND FOLLOW-UP
The next day there was improvement in the left ptosis. The patient was discharged on Augmentin 875/125 mg twice daily for 7 days and PO Prednisone 40 mg tapered over 1 week. He received in total during hospitalization four doses of Ampicillin-Sulbactam, one dose of IV Dexamethasone and three tablets of PO Dexamethasone.
Ptosis resolved completely 3 days after the initial presentation. No recurrence or additional symptoms reported on a 3 months follow-up.
5 DISCUSSION
To the best of our knowledge there is only seven cases of isolated ptosis in the setting of imaging confirmed rhinosinusitis. Patient's characteristics and outcome are summarized in Table 1. Interestingly, all of them are males. Six recovered completely within 3–26 days of the onset of ptosis with medical therapy alone (case 1–4; 6–7). Five patients received antibiotics (Case 1,3,4,5, and 7). One did not (case 6) and there is no mention of treatment in one case report (case 2). One patient showed improvement 2 weeks after sinus surgery, it is not clear if the recovery is partial or complete (case 5).
| Case number | Authors | Year | Age/Sex | Associated symptoms | Imaging | AB Treatment | Systemic steroids | Time to improvement | Time to recovery |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Coker et al.3 | 1996 | 15/M | Eye pain | pansinusitis | ceftriaxone | None | NA | 3 days |
| Erosion of superior wall of MS | |||||||||
| Swelling of SR and LPS | |||||||||
| 2 | Arat et al.1 | 2013 | 44/M | Flu like symptoms | Maxillary sinusitis | NA | None | NA | 26 days |
| Eye pain | |||||||||
| 3 | Korkmaz et al.1 | 2017 | 27/M | NasaL AND PND | Ipsilateral pansinusitis | Vancomycin | None | NA | 5 days |
| Eye pain | Ipsilateral enhancement of the optic nerve and cavernous sinus | Metronidazole | |||||||
| 4 | Wilbanks et al.1 | 2018 | 9/M | Nasal congestion | Pansinusitis | NONE | NA | 14 days* | |
| Eye pain | Edema of the superolateral extraconal space of the orbit | Amoxicillin clavulanate | |||||||
| Contralateral AOM | Enhancement of the orbital bony plate | ||||||||
| 5 | Kim et al.5 | 2020 | 15/M | Headache | Pansinusitis | Broad-Spectrum | None | 14 days** | NA |
| 6 | Larcombe et al.4 | 2021 | 64/M | Nasal congestion |
ipsilateral maxillary, ethmoid and frontal sinusitis |
None | None | NA | 7 days |
| Frontal headache | |||||||||
| IPSILateral mydriasis | |||||||||
| 7 | Mirza et al.1 | 2023 | Mid-20s/M | Headache |
Bilateral ethmoid sinusitis Ipsilateral maxillary sinusitis |
Amoxicillin Clavulanate | None | NA | 3 days |
| Pungent odor | |||||||||
| Recent COVID | |||||||||
- Abbreviations: AOM, acute otitis media; LPS, levator palpebrae superioris; MS, maxillary sinus; NA, not available; SR, superior rectus.
- * Complete recovery documented with a photo sent after completion of a 14 days course of Amoxicillin Clavulanate, the specific day on which complete recovery occurred could not be documented.
- ** 14 days after surgical intervention.
Our case subject is the first in the literature to be treated in addition to antibiotics with high dose steroids. The additional benefit over antibiotics alone is not clear. We believe that the isolated ptosis in the context of rhinosinusitis is secondary to inflammation of the distal branch of the superior division of the oculomotor nerve.1 The latter course in the superior orbital fissure and enters the orbit below the origin of the superior rectus muscle where it measures 1.0 ± 0.34 mm before providing it with 2–6 innervating motor fibers. More distally before innervating the levator palpebrae superioris with 2–4 branches on average, it measures 0.68 ± 0.15 mm.2 The reason for this isolated neurologic deficit remains unclear but one can speculate that low grade inflammation is probably happening in a larger segment of the superior division of the CN3 and the smaller diameter of its distal portion make it more vulnerable. Coker et al. documented inflammation of the Superior Rectus/Levator Palpebrae Superioris complex on imaging offering another potential explanation for the isolated ptosis, that being an isolated muscular instead of neurologic injury.3 It is not clear why the case subject by Mirza et al. was complaining of olfactory dysfunction.1 However, this could be related to the recent COVID infection. Although the ptosis is usually isolated, one case subject developed mydriasis within 24 h. An extensive neurologic work-up showed no abnormalities and the patient recovered completely with only topical intranasal treatment.4
6 CONCLUSION
This case demonstrates an unusual orbital complication of rhinosinusitis. The prognosis of isolated ptosis in this setting seems favorable. It is not clear if recovery is spontaneous or due to antibiotic therapy. The use of steroids needs to be decided on a case-by-case basis since the benefit may not outweigh the harm. It is reasonable to obtain appropriate imaging to rule out cavernous sinus and orbital globe involvement. The time frame between initiation of medical therapy and consideration for surgery when improvement is lacking is yet to be defined.
AUTHOR CONTRIBUTIONS
Youssef El Sayed Ahmad: Conceptualization; data curation; formal analysis; methodology; writing – original draft. Mohammad Abraham Kazemizadeh Gol: Conceptualization; funding acquisition; methodology; resources; supervision; validation; writing – review and editing.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
The authors received no funding for this work.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interests to declare.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Not applicable. All data (of the patient) generated during this study are included in this published article.