Severe Leptospira interrogans serovar Icterohaemorrhagiae infection with hepato-renal-pulmonary involvement treated with corticosteroids
Key Clinical Message
The traditional concept of immediate antibiotic treatment in suspected leptospirosis seems to be especially important for patients up to day 4 of clinical illness. As immune mechanisms probably play a crucial role in advanced leptospirosis with presumed pulmonary hemorrhages, patients might benefit from corticosteroids or other immunosuppressive agents beside antibiotics.
Introduction
Recreational activities are more and more frequently recognized as important risk factors for acquisition of zoonoses like infections with Leptospira (L.) spp. The clinical presentation of leptospirosis may range from a nonspecific flu-like illness to a disease characterized by severe jaundice, renal failure, and meningitis. Pulmonary hemorrhages are increasingly discovered as a common feature of leptospirosis, especially in advanced cases. Here, we describe a case of severe leptospirosis due to L. interrogans serovar Icterohaemorrhagiae with hepato-renal-pulmonary involvement acquired during canoeing.
Case History/Examination
A 21-year-old male Caucasian student with kidney failure, jaundice, rhabdomyolysis, and a body temperature of almost 40°C was admitted to our department in August 2010. Two and a half weeks before, the patient started his holidays at the farmhouse of his parents near Miltenberg in Lower Franconia, Bavaria, Germany. Six days before admission, the patient developed nausea, vomiting, and watery diarrhea. Gastrointestinal symptoms were accompanied by fever, joint pain, and general body ache. Intravenous fluids and metoclopramide were administered by the family physician on day 4 of clinical illness. No other persons at the farm was affected. As the general condition of the patient deteriorated continuously over the next 2 days, he was admitted to a local hospital in the morning. In the afternoon of the same day he was transferred to our department with the presumptive diagnosis of hemolytic uremic syndrome (HUS).
On admission blood pressure was 135/85 mmHg, pulse was 110/min, respiration rate was 20/min, and temperature was 38.8°C axillary. The patient was icteric and complained about muscle ache. Chest auscultation was normal, and there was no cough or hemoptysis. Neurological examination was also normal.
Investigations
Table 1 contains pathologic laboratory parameters on admission. No fragmentocytes (“disrupted” erythrocytes) were found in the thin blood smear.
| Parameter | Value on admission | Normal range |
|---|---|---|
| C-reactive protein (CrP) | 20.67 mg/dL | <0.5 mg/dL |
| Total bilirubin (biliT) | 9.75 mg/dL | <1.00 mg/dL |
| Direct bilirubin (biliD) | 8.99 mg/dL | <0.20 mg/dL |
| Aspartate aminotransferase (AST) | 382 U/L | 10–40 U/L |
| Alanine aminotransferase (ALT) | 88 U/L | 10–50 U/L |
| Cholinesterase | 4439 U/L | 5320–12,920 U/L |
| Ammonia | 23 μg/dL | 0–94 μg/dL |
| Creatinine | 2.86 mg/dL | 0.67–1.17 mg/dL |
| Urea | 108 mg/dL | <50 mg/dL |
| Creatine kinase | 9983 U/L | 190 U/L |
| Hemoglobin | 14 g/dL | 14.0–17.5 g/dL |
| Hematocrit | 36.5% | 40.0–52.0% |
| Leukocytes | 8.1 × 103/μL | 4.4–11.3 × 103/μL |
| Differential count | ||
| Neutrophils | 85% | 50–75% |
| Lymphocytes | 4% | 25–50% |
| Eosinophils | 0% | 2–6% |
| Basophils | 0% | 0–1% |
| Monocytes | 11% | 0–14% |
| Thrombocytes | 50 × 103/μL | 140–336 × 103/μL |
| Arterial blood gases (without O2 supplementation) | ||
| pO2 | 8.53 kPa | 10.00–13.33 kPa |
| pCO2 | 3.53 kPa | 4.67–6.00 kPa |
| pH | 7.50 | 7.37–7.45 |
| HCO3− | 23.20 mmol/L | 22.00–26.00 mmol/L |
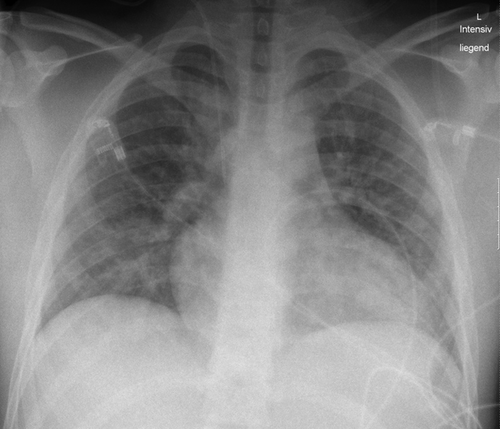
- Arterial blood gas analysis shows hypoxemia, hypokapnia, and alkalosis. The bilateral diffuse heterogeneous airspace opacities impaired the gas exchange in the lung. Reduced diffusion capacity of O2 decreased pO2. Compensatory hyperventilation lowered pCO2 and increased pH representing finally acute respiratory alkalosis, which is not compensated yet.
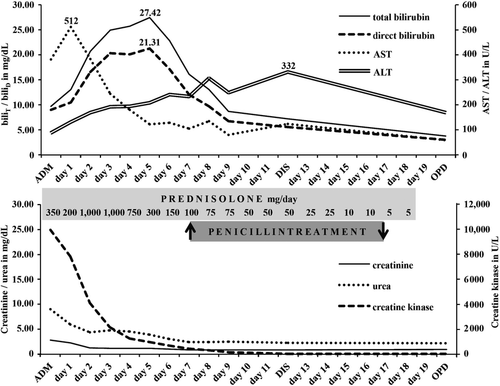
The further course of selected laboratory parameters is illustrated in Figure 1.
Hepatosplenomegaly was seen in abdominal ultrasound. The chest X-ray showed bilateral diffuse heterogeneous airspace opacities consistent with hemorrhages or pneumonic infiltrations (Fig. 2).
Differential Diagnosis
Initial differential diagnoses included HUS (thrombocytopenia), hanta virus infection (elevated creatinine), and leptospirosis (elevated creatinine, bilirubin, and creatine kinase) but also pulmo-renal syndrome due to autoimmune disorders such as Goodpasture syndrome or Wegener's granulomatosis (chest X-ray pathology, elevated creatinine).
Treatment
Due to considered autoimmune disorders it was decided to administer prednisolone intravenously 350 mg on admission and 200 mg on the following day. As HUS could not be ruled out it was decided not to prescribe antibiotics. The patient was monitored closely in the intensive care unit and received supportive therapy, which included the control of fluid and electrolyte imbalance. Blood transfusion or hemodialysis was not required.
The rapid clinical improvement, decreasing C-reactive protein (CrP) values (day 1 after admission: CrP 11.87 mg/dL; day 2 after admission: CrP 7.39 mg/dL) and improvement of the chest X-ray pathology led to the decision to continue with prednisolone 1 g/day on day 3 and 4 each, followed by 750 mg/day on day 5 and 300 mg/day on day 6. The dosage of prednisolone was then gradually reduced over the next 2 weeks to avoid secondary adrenal insufficiency (Fig. 1).
Outcome and Follow-Up
Fever reached maximum levels of 38.5°C on day 1 after admission, and 38.7°C on day 2 after admission, respectively, and then subsided with no recurrence. The chest X-ray showed an almost normal lung on day 5 after admission. The patient stayed 5 days in the intensive care unit and was then transferred to the general ward.
An in-house Leptospira-real time quantitative polymerase chain reaction (PCR) from ethylenediaminetetraacetic acid (EDTA) blood on admission performed at the Bavarian Health and Food Safety Authority (Oberschleissheim) was negative, targeting the LipL32 gene and using the IPC-ntb2 probe as an internal amplification control 1. Shigatoxin 1- and 2-genes were not detected by PCR in a stool sample either. Investigations for antinuclear antibodies, circulating immune complexes, antiglomerular basement membrane (anti-GBM) antibodies, and perinuclear/cytoplasmic-antineutrophil cytoplasmic antibodies (p/c-ANCA) yielded negative results. Further serologies were negative for hepatitis A/B/C/E virus, Epstein-Barr virus, cytomegalovirus, enteroviruses, coxsackieviruses, hantaviruses (Hantaan, Puumula, Dobrava-Belgrade virus), and Escherichia coli O157.
The result of L. interrogans serology (enzyme immunoassay) was received on day 7 after admission and yielded an IgM of 735 U/mL (normal <50 U/mL) and an IgG of 210 U/mL (normal <75 U/mL). Leptospira PCR performed from urine 1 from day 7 after admission was positive. Urine culture on semisolid Ellinghausen-McCullough-Johnson-Harris media grew leptospires after 4 weeks of incubation at 29°C. The microscopic agglutination test using standard methods 2 yielded L. interrogans serovar Icterohaemorrhagiae.
Upon receipt of the positive leptospirosis serology result on day 7 after admission, the patient was started on intravenous benzylpenicillin sodium 10 Mio. I.E. every 6 h for 3 days continued by phenoxymethylpenicillin potassium 1.5 Mio. I.E. (3 × 885 mg) orally three times a day for 7 days to prevent further urinary excretion of leptospires. Neither Jarisch-Herxheimer reaction nor fever occurred after the initiation of penicillin treatment. All laboratory parameters normalized within 5 weeks after admission.
Discussion
The clinical manifestations of leptospirosis may range from a nonspecific flu-like illness to a disease characterized by severe jaundice, renal failure, and meningitis 3, 4. In Germany, the incidence of leptospirosis increased from 0.04 per 100,000 population during the period 1992–1997 to 0.06 per 100,000 population during the period 1998–2003 5. Formerly leptospirosis was an occupational (agricultural) infection, such as the “field fever” due to the L. kirschneri serovar Grippotyphosa 4, 6; today the disease is most often linked to recreational activities with water contact and travel 5, 7.
In the case described here, the patient was admitted on day 6 of clinical illness with a hepato-renal-pulmonary syndrome and rhabdomyolysis.
Initially, HUS was considered as a very likely differential diagnosis leading to the decision not to start with antibiotics. At the time of the patient's illness (August 2010), supportive therapy was considered the most effective treatment in HUS 8. In contrast, antibiotics were regarded to worsen the prognosis 8 because of a possible induction of Shiga toxin production which may deteriorate HUS 9. Up to date, it is recommended to avoid the use of antibiotics in HUS caused by E. coli serotype O157:H7, the most commonly HUS-associated serotype 9, 10.
In our patient, HUS finally was unlikely due to the negative Shiga toxin PCR, negative E. coli O157 serology, and the absence of fragmentocytes in repeated thin blood smears.
The pathologic changes seen on the chest X-ray on admission were likewise suspicious for pulmo-renal syndrome due to autoimmune disorders such as Goodpasture syndrome or Wegener's granulomatosis. As immunosuppression with steroids is a first-line treatment option in pulmo-renal manifestation in both diseases, the decision was made to administer prednisolone. On day 1 after admission, the bilateral diffuse heterogeneous airspace opacities of the lung had already much decreased and CrP had dropped to almost half of the initial value. This rapid response seemed to confirm the supposed autoimmune disease leading to continuation of prednisolone. However, as anti-GBM antibodies and p/c-ANCA were negative, an autoimmune disease was rather improbable.
Abnormal X-ray findings in leptospirosis with and without hemoptysis were already described about 70 years ago 11. Nowadays, severe pulmonary hemorrhagic leptospirosis is increasingly being recognized 12-14. Our patient showed bilateral diffuse heterogeneous airspace opacities, possibly hemorrhages, as recently described 14, with hypoxemia and hypokapnia but without any hemoptysis. Often pulmonary hemorrhages in leptospirosis are only identified by bronchoscopy 13. There are few published cases of severe leptospirosis with pulmonary hemorrhages in which immunosuppressive treatment with corticosteroids were administered 12, 15 or cytostatic drugs were applied 16 leading to improved survival rates of the patients. Especially, advanced cases of severe leptospirosis (day 5 of clinical illness or later) may benefit from immunosuppression with steroids 17. A planned study from Brazil (ISRCTN74625030) comparing pulse therapy with methylprednisolone versus placebo beside antibiotics in all patients with pulmonary leptospirosis may provide more detailed recommendations in the future, which patients benefit most from additional corticosteroids 18.
The deposition of immunoglobulins and complement on the alveolar surface may trigger immune mechanisms leading to pulmonary hemorrhages in human leptospirosis 19. It might be that the administration of prednisolone in this patient already on admission prevented a deterioration of pulmonary function.
The clinical course of leptospirosis is often biphasic with recurrence of fever after a remission of up to 4 days 3, 4, 11. This biphasic character of leptospirosis could not be observed in the presented case possibly through the administered prednisolone. In contrast, the course of laboratory parameters in the patient followed the way that is known from classical severe leptospirosis 3, 4.
Leptospira PCR from EDTA blood on admission, day 6 of clinical illness, was negative. Culturable leptospires might be found in the blood of a patient with acute leptospirosis during the first 5 days, possibly even 7 days, after the onset of symptoms 4, 20. PCR is useful to detect leptospiral DNA in the blood over the first 10 days, in individual patients even longer 21. Leptospira interrogans serology on admission, at day 6 of clinical illness, showed already a strong antibody response supposing a short leptospiraemia and possibly a clearing of leptospires and their DNA from the blood before PCR was performed.
Urine PCR from day 7 after admission was positive and culture grew L. interrogans serovar Icterohaemorrhagiae. The causative pathogen is primarily harbored by rats 3. Leptospires excreted by rodent urine may survive for months in warm and wet soils, such as riverbanks 22. Another review of the patient's history revealed contact to stagnant water in a small branch of the Main River, where the patient had been canoeing about 12 days before the onset of illness.
In leptospirosis, the benefit of antibiotic therapy is controversial 23, especially in cases as of day 5 of clinical illness 2, 24. WHO recommends initiating treatment preferably before the fifth day after the onset of suspected leptospirosis 2. Others advise to start with antibiotics as soon as possible without taking the duration of disease into consideration 25. Experience gained from the beginning of the antibiotic era taught that high-dose penicillin treatment given to the patient up to day 4 of clinical illness, that is, before the onset of jaundice, lessened the severity of symptoms, reduced fever, and shortened the total course of illness 26. After the onset of jaundice or as of day 5 of clinical disease, antibiotics were only of little benefit to the patient 2, 4, 27. Interestingly, a recent Cochrane review found no evidence to advocate for or against the use of antibiotics in leptospirosis 24. However, only 7 studies between 1984 and 2007 were included in the review.
Our patient received a 10-day course of penicillin when he was already in convalescence.
In patients with leptospirosis who not received antibiotics leptospires may remain in immunologically sequestered sites like renal tubules and eye 28. Ocular involvement like uveitis or iridocyclitis may occur between weeks and months after the febrile stage 2, 28 caused by leptospires directly 29 or through autoimmunity 3.
Investigations from the 1960s found a prolonged excretion of leptospires in urine in untreated sick and convalescent patients up 64 days in Germany 4 and up to 134 days in Asia 30. Human-to-human transmission through urine has been discussed 30, 31 but no reference case exists in the literature.
Finally, to avoid a probable persistence of leptospires in the kidneys and in the eye, a 10-day course of penicillin was prescribed to the patient. This duration is considered effective to cure leptospirosis, provided appropriate high doses of penicillin or doxycycline are given 4.
Acknowledgment
This case was presented in part as a poster at the 64th Annual Conference of the German Society for Hygiene and Microbiology held from 30 September to 03 October 2012 in Hamburg, Germany. The abstract of the poster was published in the supplement of the International Journal of Medical Microbiology 32.
Conflict of Interest
None declared.