A rare case of eosinophilic annular erythema, an uncommon new entity of eosinophilic dermatosis
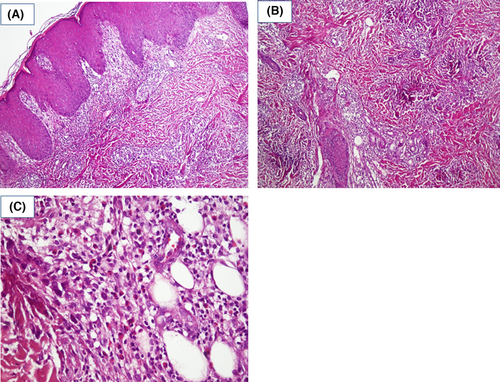
A 3-year-old boy was referred to Razi Dermatology Hospital due to multiple pruritic plaques on the trunk and proximal extremities for 2 months. His parent reported multiple, self-healing, similar pruritic skin eruptions since 1 year ago. They denied any preceding pain or edema before skin eruptions. Physical examination revealed multiple annular and arcuate-like erythematous plaques in the posterior neck, face, trunk, back, proximal, and distal lower extremities (Figure 1A–C). The central clearing was noticed in some of the lesions. Initial lab test for complete blood count, liver function, renal function, thyroid function, blood sugar, lactate dehydrogenase were within normal range. Complete blood count lacked leukocytosis and peripheral eosinophilia. A punch trunk biopsy was performed with the differential diagnosis including erythema annular centrifugum (EAC), subcutaneous lupus erythematous, urticaria vasculitis, granuloma annulare, erythema marginatum, and eosinophilic annular erythema (EAE). Histological evaluation showed the dermal infiltration of lymphocytes and numerous dermal eosinophils with a flame figure (Figure 2A–C). No signs of vasculitis, granulomatous changes, or blister formation were seen in the histopathological evaluation. The diagnosis of EAE was made depending on the clinical and pathological findings and the onset of the disease was attributed to more than 1 year ago when the child was only 2-year-old. An oral antihistamine, loratadine syrup, with topical triamcinolone acetate was started. Unfortunately, the patient did not come back for further evaluation and follow-up.

EAE is a rare eosinophilic rich, figurate erythematous dermatosis. EAE has no predilection for specific age group, but typically presents after the age of 1 year. The youngest reported case was 20-month-old and the eldest patient reported to be 82-year-old.1, 2 The precise etiology of EAE is not understood. Hypersensitivity to an unknown antigen was suggested. Also, a vague association with chronic borreliosis was reported. However, antibiotic therapy against borreliosis was not effective in clearing EAE. Other possible associations are autoimmune thyroid disorders, renal cell carcinoma, diabetes mellitus, chronic gastritis with Helicobacter pylori infection, chronic kidney disease, chronic hepatitis C virus infection, thymoma, clear cell renal carcinoma, and metastatic prostate adenocarcinoma.3-5
EAE presents as pruritic annular or arcuate plaques mimicking deep EAC or annular urticarial-type plaques, without having scales. It predominantly involves the trunk and proximal extremities. Bullae are not a standard presenting feature. However, a case of bullous EAE with negative DIF and IIF was reported.6 Plaques may show central clearing. Individual lesions last for more than 24 h; they may be asymptomatic or may present with pruritus or rarely may be painful. Post-inflammatory hyperpigmentation or fading erythema may persist after successful treatment, but with no residual scar remnants.3, 7 Histologically, a classical finding is the presence of a dense superficial, deep perivascular, and interstitial lymphocytic infiltration, In addition to eosinophilic infiltration. The flame figure is not a typical presentation, although it may be present in the longstanding lesions. Focal basal vacuolar damage and pigment incontinence may be present. Mucin deposition and vasculitis are absent. The principal differential diagnosis is the annular erythema of infancy and Wells syndrome. Other entities that should be differentiated are deep EAC, tumid lupus erythematous, Jessner lymphocytic infiltrate, urticarial phase of bullous pemphigoid, interstitial granulomatous disorders, and granuloma annulare.3, 7
Although EAE could be self-healing, it usually follows a chronic relapsing and remitting course that is resistant to multidrug treatment. Systemic steroids and antimalarial (hydroxychloroquine) are the standard first-line therapy that can clear the lesions. However, relapse after discontinuation is frequently reported.3, 4 Hydroxychloroquine combined with corticosteroid reported to be beneficial in refractory cases.8 Clinical remission with nicotinamide, cyclosporine, dapsone, indomethacin, doxycycline, mycophenolate mofetil, dupilumab and phototherapy also has been reported.3, 4, 8, 9 A 39-year-old male patient with diffuse EAE was successfully treated with doxycycline 100 mg/twice daily with substantial resolution of lesions within 3 months, complete clearance within 1 year, but with recurrence after cessation of the drug. Mycophenolate mofitel was reported to clear skin lesions of EAE in a patient with autoimmune hepatitis but was discontinued because of raised liver enzymes. Also, an eight sessions narrow-band ultraviolet B phototherapy was reported to result in complete clearance of lesions of EAE in an 8-year-old male patient. Lastly, dupilumab was reported to successfully treat 14-year-old female patient with EAE.
AUTHOR CONTRIBUTIONS
Saman Al-Zahawi: Writing – original draft; writing – review and editing. Maryam Nasimi: Conceptualization; supervision. Vahidesadat Azhari: Supervision; visualization. Zahra Razavi: Supervision; writing – original draft; writing – review and editing.
ACKNOWLEDGMENTS
The authors are grateful of the Tehran University of Medical Sciences.
FUNDING INFORMATION
No funding was received for this article.
CONFLICT OF INTEREST STATEMENT
None.
CONSENT
Written informed consent was obtained from the patient's parents.
Open Research
DATA AVAILABILITY STATEMENT
The authors elect not to share data.