Respiratory distress in a neonate: Inflation of a third branchial anomaly with positive airway pressure
Key Clinical Message
Positive airway pressure from noninvasive ventilation is an essential tool for many pediatric patients with respiratory distress. We present a case of an unknown third branchial anomaly that was diagnosed following inflation with continuous positive airway pressure (CPAP), which exacerbated the infant's respiratory distress.
1 INTRODUCTION
Branchial cleft anomalies are responsible for up to 20% of all pediatric neck masses.1 Although present at birth, they may not be recognized until later in life by pediatricians and general practitioners. Knowledge of the embryological origins of the branchial arch derivatives is essential for accurate diagnosis and management. Branchial cleft cysts can often be identified by their location. In general, first branchial cysts are located between the ear and submandibular region, second branchial cysts along the lower third of the sternocleidomastoid muscle, and third branchial cysts in the lower anterior neck.1 Third branchial cleft anomalies have a prevalence of 2% of all branchial cleft anomalies and are almost exclusively left sided.2, 3 The embryological third branchial pouch originates at the piriform sinus and gives rise to the inferior parathyroid glands and thymus.3 As a result of incomplete obliteration, cysts, sinuses, or fistulae can be formed.4 Third branchial anomalies have a range of presentations, most commonly recurrent left-sided neck abscesses or acute suppurative thyroiditis.5, 6 However, their presentation can vary widely. To our best knowledge, we report the first case of a third branchial cleft cyst that was diagnosed following inflation with positive pressure ventilation.
2 CASE REPORT
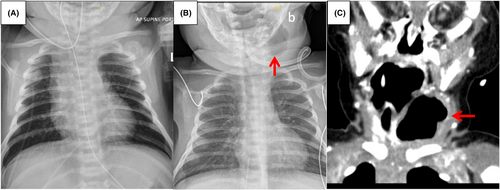
Following an uncomplicated pregnancy and delivery, a 36 + 1 week neonate was transferred to the NICU for hypoglycemia with poor feeding on day-of-life (DOL) 1. Subsequently, the baby developed sepsis with fever, lethargy, bradypnea, and respiratory acidosis on DOL 3. Chest X-ray was normal at this time, demonstrating no abnormalities in the neck or chest (Figure 1A). The baby's respiratory status worsened, requiring CPAP and eventually transfer to a quaternary care hospital on DOL 5. Chest X-ray was normal prior to the initiation of CPAP, demonstrating no abnormalities in the neck or chest (Figure 1A). The baby was started on broad-spectrum antibiotics for presumed culture-negative sepsis. Shortly after a period of stabilization and trial of weaning to room air, the baby developed hypercapneic respiratory distress and was transferred back to the NICU and restarted on CPAP. New onset stridor was noted following re-initiation of CPAP. Otolaryngology was consulted, with flexible endoscopy findings of laryngomalacia and upper airway edema with no obvious source of obstruction. The baby then developed further increased work of breathing requiring proning and increased positive airway settings. Repeat scope at that time demonstrated a new posterolateral pharyngeal wall bulge but no obvious upper airway abnormality or neck mass on physical examination. A repeat chest X-ray at this time demonstrated a new large left-sided neck lesion primarily filled with air (Figure 1B). A subsequent head and neck CT scan demonstrated this air-filled sac in detail with evidence of a left-sided patent piriform sinus tract communicating with the left lobe of the thyroid gland and compressive effects on the airway (Figure 1C).
3 METHODS
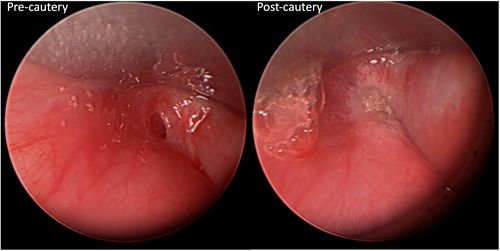
The patient was intubated and taken to interventional radiology for percutaneous needle drainage of the lesion. The patient was extubated the next day and remained stable on room air. Following an initial improvement in breathing, the patient developed mild intermittent stridor a few days later, and repeat imaging demonstrated re-accumulation of air. Definitive treatment options were presented to the patient's family, which included operating room (OR) for endoscopic evaluation and cauterization of the piriform sinus tract, repeat needle decompression, and open resection of the cyst with hemithyroidectomy. The decision was made to perform endoscopic cauterization given the risk of damage to the RLN and parathyroid glands via an open surgical resection in a small neonate was felt to be high. The patient was taken to the OR 2 weeks after the initial needle decompression for direct laryngoscopy, which demonstrated a patent left pyriform fossa sinus tract. Endoscopic cauterization of the tract with a bugbee catheter was performed (Figure 2). The baby was transferred postoperatively directly to the ward on room air, with complete resolution of stridor, and transitioned to oral intake. He was discharged home 1 week after surgery in stable condition. There has been no evidence of recurrence 2 years postcauterization on subsequent follow-ups with serial neck ultrasounds and flexible endoscopy.
4 DISCUSSION
This case report outlines a unique presentation of a third branchial cleft cyst in a neonate on CPAP, where positive pressure ventilation inflated the branchial anomaly with air, causing an expanding neck mass, upper airway obstruction, and worsening respiratory distress. Needle decompression of the air-filled branchial anomaly temporized the baby, who ultimately required endoscopic cauterization for definitive management.
Third branchial anomalies are typically found at the left lower anterior neck.3 The cysts classically run superficial to cranial nerve X and the common carotid artery, superficial to cranial nerve VII, and deep to cranial nerve IX.3 The associated tract, if present, passes through the thyrohyoid membrane above the superior laryngeal nerve and opens into the upper piriform sinus.3 Third branchial anomalies can present as an abscess, neck mass, or acute suppurative thyroiditis,5, 6 and in our case, stridor and respiratory distress upon initiation of positive pressure ventilation. Diagnosis of these anomalies can be confirmed by contrast swallow studies, CT scan, and MRI, but ultimately requires direct laryngoscopy.5, 6
Options for definitive treatment of third branchial anomalies range from complete open surgical excision of the sinus tract with thyroid lobectomy as the tract is often in close association with the left thyroid gland, simple incision and drainage, endoscopic electrocauterization of the pirifom sinus tract, and a combination of techniques.2 Historically, third branchial cleft cysts were treated definitively with open resection of the cyst and hemithyroidectomy; however, this technique poses a risk of damage to the RLN and parathyroid glands in small children, be complicated by fibrosis and scarring, as well as postoperative wound infection and salivary fistula.5, 7 Furthermore, less than 12% of all third branchial anomalies present in the neonatal age6 as in the case presented here, and a systematic review and meta-analysis showed the neonates with third branchial arch anomalies who undergo open surgical resection have a higher rate of postoperative complications (15%–17%) compared to children 1 year of age and older (4.5%).6 These authors therefore recommended against an open approach as the primary treatment modality, especially in neonates.6 Incision and drainage is most commonly performed in the context of abscess collection during the workup of a branchial anomy, with the knowledge that this technique incurs a high recurrence rate of around 94%–100%.2, 6 In the case presented here, there was a collection of air rather than abscess, for which needle decompression was effective temporarily. However, just like with aspiration of an abscess, the air did recollect.
More recently, minimally invasive endoscopic cauterization of the piriform sinus tract has been shown to have similar success rates as open resection.2, 6, 7 A recently published retrospective study demonstrated a success rate of 94% for a combined approach of surgical excision with concurrent endoscopic cauterization as primary treatment.8 Complications following endoscopic cauterization are exceedingly rare and include temporary superior or RLN paralysis.2, 6, 9 Thus, many today advocate for endoscopic cauterization as the primary treatment for third branchial cleft anomalies as it is minimally invasive, has a comparable success rate, and is associated with fewer complications compared to surgical resection.2, 7, 10 However, a recent systematic review demonstrated that surgical excision is still the most performed treatment for third branchial anomalies, despite the higher complication rate reported in the literature.2 In our patient, given the patient's age and size, which have been demonstrated to be associated with a higher risk of complications with open procedures, we elected to treat with needle decompression to temporize the airway followed by endoscopic cauterization of the fistula tract, which is consistent with a minimally invasive approach reported by Wong et al.11
Following initiation of CPAP, which is the standard of care in patients with progressive respiratory failure, our patient worsened clinically, and imaging findings demonstrated a new predominantly air filled left-sided neck mass that was ultimately determined to represent a third branchial cleft anomaly. This neck mass was not present on imaging prior to re-initiation of CPAP and increased positive pressure ventilation settings. Given the communication between the piriform sinus and the thyroid gland seen in third branchial anomalies, increasing positive airway pressure in our patient likely forced air through this patent tract and resulted in inflation of a cyst, causing compressive effects on the airway. When a left-sided neck mass is noted in conjunction with respiratory symptoms within the first 10 days of life, one should call into question the consideration of a third branchial pouch cyst.2 In our patient, however, there was never any sign of an external neck mass on clinical examination throughout his presentation. This may be explained by the fact that the mass was inflated with air in a relatively short time course.
5 CONCLUSION
This case illustrates the importance of a solid understanding of the embryology of the branchial arches in the diagnosis and treatment of branchial anomalies. It is important to consider that although positive airway pressure from noninvasive ventilation is an essential tool for many pediatric patients with respiratory distress, in certain cases due to anatomical abnormalities such as a third branchial anomaly, it may exacerbate symptoms. Additionally, not all third branchial anomalies present initially with a neck mass or abscess and it is reasonable to consider that the initiation of positive pressure ventilation may have precipitated these compressive airway symptoms, which may otherwise have remained dormant.
AUTHOR CONTRIBUTIONS
Chantal Li: Conceptualization; data curation; investigation; writing – original draft; writing – review and editing. Jennifer M. Siu: Formal analysis; methodology; writing – review and editing. Mary-Angela Woodward: Data curation; resources; writing – original draft; writing – review and editing. Nikolaus E. Wolter: Conceptualization; data curation; investigation; methodology; project administration; resources; supervision; writing – original draft; writing – review and editing.
FUNDING INFORMATION
None to report.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICS STATEMENT
This article describes a case report. Therefore, no additional Research Ethics Board approval was required.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
IRB EXEMPTION
This case report is exempt from IRB approval as indicated on the uploaded letter from the Hospital for Sick Children.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




