A worn Björk–Shiley prosthetic valve without valve dysfunction observed during ascending aortic replacement
Key Clinical Message
The implanted first-generation Björk–Shiley valve in our patient was functioning well before aortic surgery, but we replaced the valve because we confirmed disc erosion 39 years after implantation during the surgery. We judged that the implanted valve was no longer capable of maintaining the patient's life.
Introduction
The original model for the Björk–Shiley mechanical valve (Shiley Inc, Irvine, CA) is at potential risk of disc deformity or fracture. Therefore, in 1971, the disc material was changed from Delrin® to pyrolite carbon. In the present case report, we replaced a well-functioning but worn Björk–Shiley valve during an emergency surgical repair of an acute aortic dissection.
Case Presentation
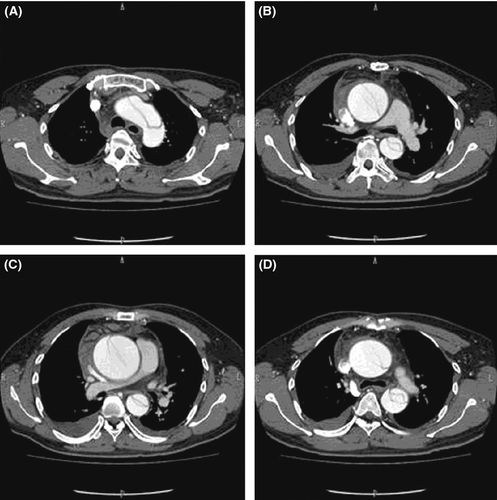
A 51-year-old man presented complaining of sharp upper back pain and right leg numbness. Thirty-nine years ago, his aortic valve was replaced with a 23-mm Björk–Shiley mechanical valve, and he was since maintained on Coumadin anticoagulant therapy. We could not get any other information about the valve. Chest and abdominal computed tomography revealed a dilated sino-tubular junction associated with a type A acute aortic dissection (Fig. 1). Echocardiographic findings showed good prosthetic valve function with 2.73 m/sec peak flow velocity and 2.0 cm2 of the prosthetic valve area. We inferred that the leg numbness was likely caused by impaired spinal cord blood flow.
He underwent an emergency aortic surgical repair of the type A dissection. Resternotomy was performed using cardiopulmonary bypass under the right axillary artery and right femoral vein cannulation. After the additional superior vena cava cannulation, the heart was arrested with antegrade cardioplegic solution followed by intermittent retrograde cardioplegic solution. We observed that the implanted Björk–Shiley valve disc was worn and concave at the site meeting the strut on the ventricular surface (Fig. 2). The intimal flap was recognized in the ascending aorta. We judged that the implanted valve was Björk–Shiley Delrin one, and that it was no longer capable of maintaining the patient's life. The worn Björk–Shiley valve was removed, and a valved conduit with a mechanical valve was implanted. The bilateral coronary artery orifices were reconstructed in an ordinary fashion. The distal anastomosis of the ascending aorta was just below the brachiocephalic artery. The brain was protected during aortic reconstruction by systemic moderate hypothermia and retrograde cerebral perfusion.

Postoperative recovery was uneventful, and the leg numbness subsided. Echocardiography showed normal prosthetic and left ventricular functions. He was discharged 12 days postoperatively, and he is doing well 2 years after the procedure.
Discussion
Mechanical valves historically have overcome many structural dysfunctions such as leaflet dislodging, disc fracture, and others. Present day mechanical valves have an extremely low rate of structural valve dysfunction.
The Björk–Shiley valve was the first tilting disc mechanical valve implanted for heart valve replacement 1. The valve disc was initially made from Derlin® 2, 3, but the material was later changed to pyrolytic carbon because of the potential risks of disc wear or fracture 4, 5. Some clinical studies have reported cases of structural valve dysfunction of the Björk–Shiley valve 6-8. In Japan, 23 cases of Björk–Shiley valve dysfunction have been reported, including structural dysfunctions 18 to 41 years after the initial implantation 9.
The implanted valve in our patient was functioning well before aortic surgery, but we replaced the valve because we confirmed disc erosion 39 years after implantation. This report may be the first describing a Björk–Shiley valve with disc erosion before the appearance of structural dysfunction. A patient with the first-generation Björk–Shiley valve may undergo repeated cardiac surgeries. In these patients, we should consider replacing the implanted valve.
Conclusions
The original Björk–Shiley mechanical valve model is at potential risk of disc deformity or fracture. We should consider replacement of this Björk–Shiley valve during future cardiac surgeries.
Conflict of Interest
Misawa Y serves as a consultant to Terumo Co. and Edwards Lifescience Co.