Neglected massive multinodular goiter during pregnancy with dyspnea and successful normal delivery: A case report
Abstract
Key Clinical Message
Prompt coordinated care enables vaginal delivery for severe goiter-induced airway compression in late pregnancy when expectant management is precluded.
Long-standing neglected multinodular goiter rarely causes life-threatening airway compression in late pregnancy. Most cases report cesarean delivery to relieve respiratory distress. Vaginal birth may also be possible, but the evidence is limited. A 30-year-old woman with a 7-year goiter history developed severe dyspnea at 34 weeks gestation. Despite the risks, labor was induced by urgent decompression. She vaginally delivered a premature but healthy infant. Her breathing improved after delivery. She later underwent an uncomplicated thyroidectomy. With careful selection and monitoring, vaginal delivery can be considered for goiter-induced respiratory compromise when expectant management is precluded. This case demonstrates successful urgent decompression and favorable maternal-fetal outcomes are possible with a coordinated approach despite the high-risk scenario.
1 INTRODUCTION
Multinodular goiter, characterized by multiple nodules in the thyroid gland, can gradually enlarge over time, particularly in iodine-deficient regions.1, 2 The condition may manifest as diffuse thyroid enlargement or a dominant solitary nodule within the multinodular gland. Assessment involves thyroid function tests, antibody levels, and imaging modalities like ultrasound, radioisotope scanning, or CT.3-5 Treatment depends on goiter size, compressive symptoms, thyroid status, and cancer risk, ranging from monitoring to levothyroxine, radioiodine, or surgery.6, 7 Pregnancy poses additional challenges, as estrogen and increased thyroid hormone demand can exacerbate goiter growth,8 rarely leading to life-threatening airway compression. Though cesarean delivery may urgently relieve respiratory distress,9 vaginal delivery with airway decompression may also be possible in selective cases,10 avoiding surgical risks.
This case describes a patient with long-standing neglected multinodular goiter first causing life-threatening respiratory compromise at 34 weeks gestation. Despite the significant risks posed by both the patient's respiratory status and premature delivery, a coordinated multidisciplinary approach allowed urgent decompression through successful induction of labor and vaginal delivery of a healthy infant. This rare case highlights that when severe goiter compresses the airway, precluding expectant management, planned vaginal birth can be considered to achieve urgent decompression if done carefully with a coordinated approach involving input from relevant specialties.
2 CASE PRESENTATION
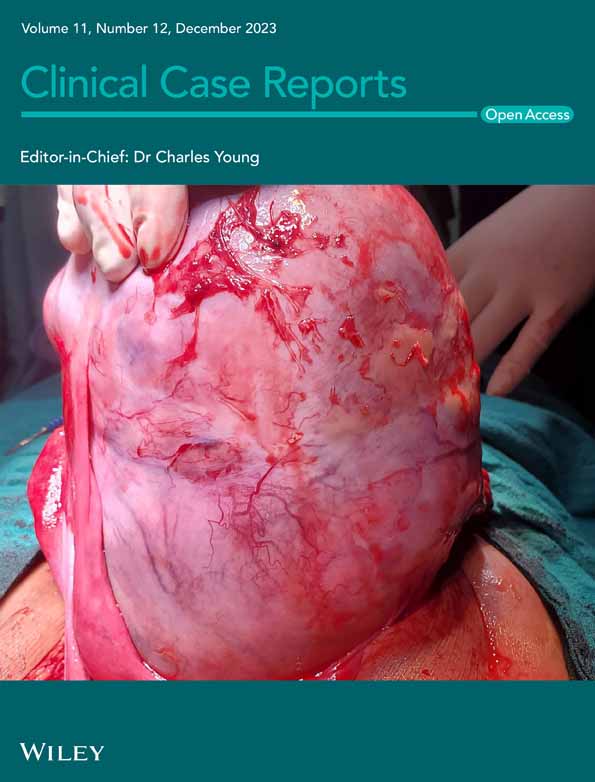
The patient was a 30-year-old woman, gravida 9 para 8, at 34 weeks gestation, who presented with a 7-year history of anterior neck mass from a long-standing multinodular goiter. Although it had not markedly increased in size during pregnancy, it recently started causing compressive symptoms, including hoarseness, chest tightness, and dyspnea. The examination showed a massive multinodular goiter with jugular vein distension and audible stridor, oxygen saturation of 81%, normal blood pressure, and normal fetal heart rate (Figure 1). Due to severe respiratory compromise, urgent delivery was recommended. After counseling on risks, labor was induced using dinoprostone and oxytocin augmentation, allowing vaginal delivery of a 2.1 kg premature male infant in good condition. Dexamethasone was administered to enhance fetal lung maturity, given anticipated preterm delivery. The patient's breathing improved after delivery, and she underwent thyroidectomy postpartum after stabilization.

3 CLINICAL FINDINGS
After delivery, the patient's respiratory status and vitals improved with supplemental oxygen. Thyroid function tests were normal, and ultrasound confirmed the multinodular goiter. She underwent uncomplicated total thyroidectomy on postpartum Day 5, with histopathology showing colloid nodular goiter. She recovered well postoperatively and was discharged home in good condition on postpartum Day 7 with instructions for postoperative care and follow-up. During her 2-week follow-up, she reported significant improvements in breathing and resolution of compressive symptoms. Her incision had healed well without infection. At 6 months postpartum, the patient remained in good health with no recurrent goiter or complications while caring for her infant. She required ongoing levothyroxine replacement but was otherwise asymptomatic (Figure 2).

4 DISCUSSION
The severity of the patient's respiratory compromise at 34 weeks, including low oxygen saturation, stridor, and jugular vein distension, raised concerns about her ability to tolerate expectant management for several more weeks. The gestational age of 34 weeks was far enough along that prematurity risks were judged acceptable compared with maternal respiratory risks of delayed delivery. Steroid administration accelerated fetal lung maturity, further supporting the likelihood of a good outcome with early delivery. Avoiding the risk of thyroid surgery in the third trimester was desirable, and thyroidectomy could be performed postpartum once the patient was stabilized without the same risks as operating at 34 weeks.
This case highlights the challenges of managing severe airway compression from long-standing neglected goiter presenting in late pregnancy. Despite the risks, we pursued vaginal delivery for urgent decompression, resulting in favorable outcomes. Most reported cases describe caesarean section in this scenario.9 However, our case aligns with limited evidence suggesting vaginal birth may be appropriate for selected patients if expectant management is precluded.6, 10 Close monitoring for fetal distress was prudent given prematurity and maternal compromise. Reassuringly, the premature infant had good Apgar scores, likely aided by antenatal steroids. The two-stage approach allowed fetal protection while providing definitive treatment. Postpartum thyroidectomy is essential to prevent recurrence and complications.10
This case demonstrates that with a coordinated multidisciplinary approach, airway decompression and delivery of a premature but healthy infant via vaginal birth are possible despite the high-risk scenario. It highlights the need for prompt care when managing this uncommon but life-threatening presentation in pregnancy.
5 CONCLUSION
This case illustrates the successful management of a rare but high-risk scenario—a neglected massive multinodular goiter causing severe airway compression in late pregnancy. Despite significant challenges, a coordinated multidisciplinary approach allowed stabilization, planned vaginal delivery for urgent decompression, and subsequent definitive thyroidectomy. This resulted in good outcomes for both the mother and premature but otherwise healthy newborn. The case adds to limited evidence that with appropriate patient selection, monitoring, and care team collaboration, vaginal birth can be considered to safely decompress the airway when expectant management is not feasible. This highlights the importance of prompt recognition and treatment when this life-threatening presentation occurs in pregnancy.
AUTHOR CONTRIBUTIONS
Maguzu L. Nganga: Conceptualization; data curation; investigation; methodology; writing – review and editing. Clement N. Mweya: Writing – original draft; writing – review and editing.
ACKNOWLEDGMENTS
We sincerely thank specialists and other staff in the Department of Obstetrics and Gynaecology at Mbeya Zonal Referral Hospital for their invaluable contributions and feedback, which greatly enhanced the quality of this work.
FUNDING INFORMATION
The author(s) received no financial support for this work.
CONFLICT OF INTEREST STATEMENT
All authors report no conflicts of interest with respect to the research, authorship, and/or publication of this article.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.