Multiple primary cutaneous plasmacytoma a decade after a nasal solitary extramedullary plasmacytoma: a puzzling case
Key Clinical Message
Primary cutaneous plasmacytoma should be in the differential diagnosis in case of solitary or multiple erythematous–violaceous nodules or papules. The diagnosis relies on clinical, histological, and immunochemical findings, without underlying evidence of multiple myeloma. Treatment should be individualized, and agents such as bortezomib or lenalidomide have shown to be effective.
Introduction
Multiple myeloma (MM) is a malignant hematological disease characterized by the proliferation of clonal plasma cells in the bone marrow with monoclonal immunoglobulin production leading to anemia, renal impairment, hypercalcemia, and bone lesions 1, 2. Dissemination to the skin (secondary cutaneous plasmacytomas) is usually associated with advanced stages of the disease. By contrast, primary cutaneous plasmacytoma (PCP) is a very rare skin tumor characterized by the absence of bone marrow myeloma infiltration as well as absence of organ damage 1, 3, 4.
Case History
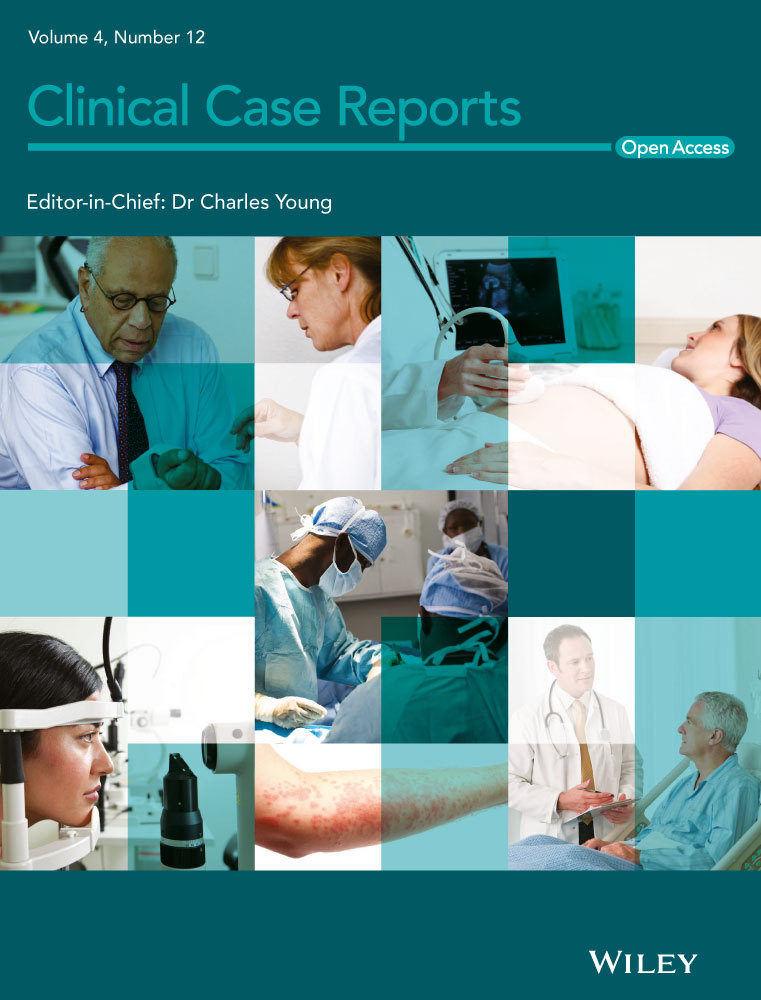
A 76-year-old man was referred to our hospital in January 2013 by his general practitioner because of asymptomatic skin lesions that had appeared 1 month earlier. The physical examination revealed erythematous–violaceous papules and nodules, measuring 0.5–2 cm on the face (Fig. 1A–C), upper chest, back (Fig. 1D), upper extremities, and legs.
Ten years before the patient had been diagnosed having a solitary extramedullary plasmacytoma (SEP) located at the left inferior nasal concha without bone marrow infiltration as well as absence of any other sign of myeloma dissemination including the lack of monoclonal M-component. He achieved and maintained complete remission after treatment with surgical excision and local radiotherapy. Complete remission was confirmed through a new nasal biopsy after treatment.
He was followed up during this period of 10 years with physical examination, evaluation of the monoclonal component by serum and urine protein electrophoresis and immunofixation serum-free light-chain (FLC) measurement and annual computed tomography (CT). The only relevant finding during this period of time was the emergence of a monoclonal IgG-Kappa band, with a normal FLC ratio in 2011, that reached 0.7 mg/dL in 2013.
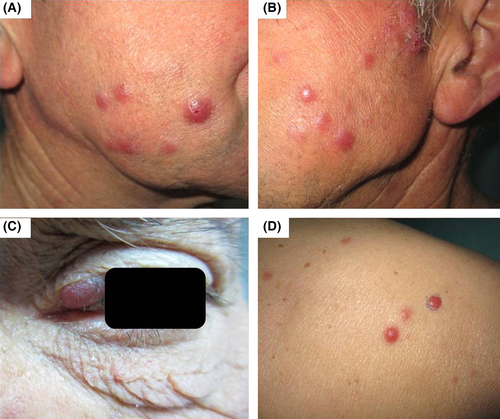
At the moment of appearance of the cutaneous lesions, an excisional skin biopsy was performed that revealed a diffuse-pattern proliferation of neoplastic plasma cells in the superficial and deep dermis reaching the subcutaneous tissue with dissection of reticular dermis collagen (Fig. 2A and B). Epidermis and papillary dermis were not affected (Fig. 2C). Cells showed an enlarged size, basophilic cytoplasm, atypical nucleus with clumped chromatin and small nucleolus (Fig. 2D).
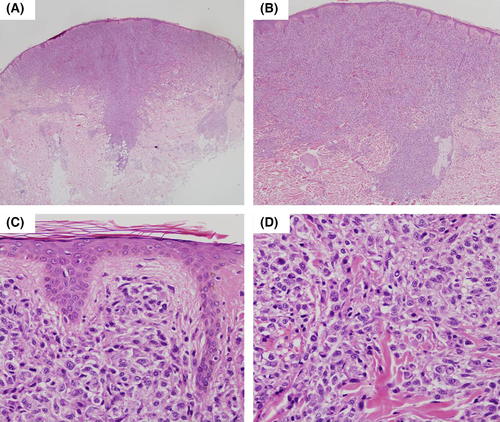
Immunohistochemical analysis revealed positivity for CD79A (Fig. 3A), CD138 (Fig. 3B), CD56, BCL2 (Fig. 3C), MUM1 (Fig. 3D), as well as negativity for CD3, CD5, CD10, CD20, CD23, CD43, PAX5, BCL6, ciclyne D1, EMA, EBER (EBV). Restriction for Kappa light chains was demonstrated. Proliferative index for Ki67 was approximately 15%.
Therefore, it was concluded that the biopsy's skin was infiltrated by a plasma cell neoplasm that was compatible with a primary multiple cutaneous plasmacytoma. The initial nasal biopsy was revised, and it was concluded that both samples were morphologically and immunohistochemically identical.
A thorough search for underlying MM was conducted using imaging techniques (skeletal survey and CT scan), serum and urine protein electrophoresis, FLC, and bone marrow aspirate. The absence of myeloma-related symptomatology or findings excluded symptomatic MM from the diagnostic possibilities.
Considering the extensive dissemination of the cutaneous involvement, and according to the age of the patient, good performance status and lack of comorbidities, the patient received systemic therapy with a regimen including bortezomib, adriamycin, melphalan, and prednisone (VAMP). After the first six cycles, complete disappearance of the skin lesions and monoclonal component was noticed, and thus, complete response (CR) was obtained. Induction treatment was well tolerated, and the patient received consolidation for six additional cycles with an alternating scheme including the previous regimen (VAMP), alternating with thalidomide, cyclophosphamide, and low-dose dexamethasone (TaCyDex).
Although a relapse of primary multiple cutaneous plasmacytoma was detected 2 years after end of treatment, the patient is still alive and remains CR under continuous lenalidomide and dexamethasone treatment.
Discussion
Monoclonal gammopathies constitute a heterogeneous group of diseases characterized by the presence of a single clone proliferation of plasma cells, typically producing a monoclonal immunoglobulin. These entities include a wide spectrum of disorders, from monoclonal gammopathy of uncertain significance to multiple myeloma, plasma cell leukemia, solitary bone plasmacytoma (SBP), or extramedullary plasmacytoma (EMP) 3, 5.
Solitary plasmacytoma (SP) is a rare neoplasm defined by localized clonal plasma cell (PC) infiltration without systemic tumor dissemination. Both the skeletal survey and the bone marrow are normal, and no related organ or tissue impairment is observed. Localized clonal PC infiltrates may arise either in the bone (SBP) or extramedular (EMP). Approximately 50% of patients with SBP and 15% with EMP will evolve into MM 6.
Within the EMP group, solitary extramedullary plasmacytomas (SEP) are usually localized in the upper respiratory tract and constitute around 3–5% of all plasma cell neoplasms 7, 8. Some patients have a small monoclonal protein, in the serum or urine, that disappears after treatment 3, 4, 9. In our patient, no monoclonal component was detected at the time of the nasal plasmacytoma; however, it was detected 2 years before the second episode. In some patients with SP, clonal plasma cells can be detected in the bone marrow using sensitive techniques such as flow cytometry and this finding is associated with higher risk of progression to active disease 6. However, in our patient, no clonal plasma cells infiltration was observed by high-sensitive flow cytometry investigation neither at diagnosis of nasal EMP nor currently.
When only the skin is affected, EMP is referred to as cutaneous plasmacytoma, which is divided into primary cutaneous plasmacytoma (PCP) when there is no evidence of underlying disease, or secondary when it is the result of cutaneous involvement of a hematological systemic disease (approximately in 10% of MM cases) 1, 3, 4, 8. PCP are infrequent tumors, comprising <5% of all primary extramedullary plasmacytomas, and show considerable overlap with the plasmacytic variant of the primary cutaneous marginal zone B-cell lymphoma (PCMZL) included in the World Health Organization-European Organization for Research and Treatment of Cancer classification 10, 11.
Diagnosis is based on clinical, histological, and immunochemical findings. Clinically, PCP patients develop solitary or multiple erythematous–violaceous subcutaneous papules, nodules, and/or plaques with a diameter from 1 to 5 cm, with a predilection for the face, trunk, and extremities 4, 9, as was our patient's case. However, some authors state that there are no predilection sites 8, 10. It seems to be more frequent in elderly male population 4. From a histological point of view, a dense monomorphic plasmacytic infiltrate is usually found in the superficial dermis with the epidermis generally spared 4. Atypia, binucleation, and increase in the mitotic activity can be present. Immunohistochemical study usually features positivity for CD79 4, CD138 9, CD38, CD56 8, and MUM1/IRF4 7, 8 and CD20 negativity 4, 7. This technique also allows distinguishing reactive plasma cell proliferation by infections or inflammatory processes from PCP 4, 8. Diagnostic criteria include cytoplasmic expression of immunoglobulins restricted to one immunoglobulin chain and exclusion of underlying myeloma through laboratory, radiological, and bone marrow investigations 9. All of these criteria were met in our patient's case.
Therapy options range from surgical excision plus radiotherapy in the case of solitary plasmacytomas 1, 6, to systemic therapy in the case of multiple lesions, as occurred in our case 4, 9. Novel agents, such as proteasome inhibitors and immunomodulatory drugs, have been recently introduced in the treatment of patients with MM, and they have showed to be also effective in EMP, especially for proteasome inhibitors 15, 16. In this patient, our first choice was to combine the proteasome inhibitor bortezomib with conventional agents such as melphalan and prednisone. This combination has demonstrated to be effective in patients with MM. Due to the presence of multiple PCP, we added adryamicine to enhance the synergistic effect. Our patient achieved complete remission after six cycles, and this response was consolidated with six additional cycles of VAMP, but alternating them with an immunomodulatory drug-based combination (TaCyDex) to upgrade the response and avoid the selection of resistant clones. After the last relapse, continuous lenalidomide in combination with dexamethasone was chosen. Treatment was well tolerated and effective, achieving a sustained CR.
On the one hand, although our patient had a previous SEP, no circulating aberrant plasma cells were identified in peripheral blood using flow cytometry assessment. Although the sensitivity of the flow cytometry is high, assessments of higher sensitivity would be required to identify the clonal plasma cells. Regarding this, it is important to take into account that it is hypothesized that clonal plasma cells are able to circulate 12-14 resulting in multiple plasmacytomas 6.
On the other hand, regardless the fact that diagnosis of primary cutaneous plasmacytoma was performed after excluding the presence of both myeloma and plasmacytoma of any other organ system, it is important to note that the review of the initial nasal biopsy concluded that both samples were morphologically and immunophenotypically identical.
Therefore, it is impossible to elucidate whether the latest malignant plasma neoplasm constitutes a late relapse, or instead both episodes are not related with the patient presenting a multiple PCP after an ESP.
Conclusion
We present the case of a patient with a multiple cutaneous plasma cell neoplasm with a dermatopathology analysis that favors the option of a common origin of the latest episodes and the previous nasal plasmacytoma. To our knowledge, this is the first case of a multiple PCP with such a long history of previous ESP and good response to treatment.
Conflict of Interest
None declared.